|
|
 |
| ............................................................. |
|
October 2017 -
Volume 15, Issue 8
|
 |
|
View
this issue in pdf formnat - the issue
has been split into two files for downloading
due to its large size: FULLpdf
(12 MB)
Part
1 &
Part
2
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
........................................................
|
|
Original Contribution/Clinical Investigation
Immunity
level to diphtheria in beta thalassemia patients
DOI: 10.5742/MEWFM.2017.93048
[pdf
version]
Abdolreza Sotoodeh Jahromi, Karamatollah Rahmanian,
Abdolali Sapidkar, Hassan Zabetian, Alireza
Yusefi, Farshid Kafilzadeh, Mohammad Kargar,
Marzieh Jamalidoust,
Abdolhossein Madani
Genetic
Variants of Toll Like Receptor-4 in Patients
with Premature Coronary Artery Disease, South
of Iran
DOI: 10.5742/MEWFM.2017.93049
[pdf
version]
Saeideh Erfanian, Mohammad Shojaei, Fatemeh
Mehdizadeh, Abdolreza Sotoodeh Jahromi, Abdolhossein
Madani, Mohammad Hojjat-Farsangi
Comparison
of postoperative bleeding in patients undergoing
coronary artery bypass surgery in two groups
taking aspirin and aspirin plus CLS clopidogrel
DOI: 10.5742/MEWFM.2017.93050
[pdf
version]
Ali Pooria, Hassan Teimouri, Mostafa Cheraghi,
Babak Baharvand Ahmadi, Mehrdad Namdari, Reza
Alipoor
Comparison
of lower uterine segment thickness among nulliparous
pregnant women without uterine scar and pregnant
women with previous cesarean section: ultrasound
study
DOI: 10.5742/MEWFM.2017.93051
[pdf version]
Taravat Fakheri, Irandokht Alimohammadi, Nazanin
Farshchian, Maryam Hematti,
Anisodowleh Nankali, Farahnaz Keshavarzi, Soheil
Saeidiborojeni
Effect
of Environmental and Behavioral Interventions
on Physiological and Behavioral Responses of
Premature Neonates Candidates Admitted for Intravenous
Catheter Insertion in Neonatal Intensive Care
Units
DOI: 10.5742/MEWFM.2017.93052
[pdf
version]
Shohreh Taheri, Maryam Marofi, Anahita Masoumpoor,
Malihe Nasiri
Effect
of 8 weeks Rhythmic aerobic exercise on serum
Resistin and body mass index of overweight and
obese women
DOI: 10.5742/MEWFM.2017.93053
[pdf
version]
Khadijeh Molaei, Ahmad Shahdadi, Reza Delavar
Study
of changes in leptin and body mass composition
with overweight and obesity following 8 weeks
of Aerobic exercise
DOI: 10.5742/MEWFM.2017.93054
[pdf
version]
Khadijeh Molaei, Abbas Salehikia
A reassessment
of factor structure of the Short Form Health
Survey (SF-36): A comparative approach
DOI: 10.5742/MEWFM.2017.93088
[pdf version]
Vida Alizad, Manouchehr Azkhosh, Ali Asgari,
Karyn Gonano
Population and Community Studies
Evaluation
of seizures in pregnant women in Kerman - Iran
DOI: 10.5742/MEWFM.2017.93056
[pdf
version]
Hossein Ali Ebrahimi, Elahe Arabpour, Kaveh
Shafeie, Narges Khanjani
Studying
the relation of quality work life with socio-economic
status and general health among the employees
of Tehran University of Medical Sciences (TUMS)
in 2015
DOI: 10.5742/MEWFM.2017.93057
[pdf version]
Hossein Dargahi, Samereh Yaghobian, Seyedeh
Hoda Mousavi, Majid Shekari Darbandi, Soheil
Mokhtari, Mohsen Mohammadi, Seyede Fateme Hosseini
Factors
that encourage early marriage and motherhood
from the perspective of Iranian adolescent mothers:
a qualitative study
DOI: 10.5742/MEWFM.2017.93058
[pdf
version]
Maasoumeh Mangeli, Masoud Rayyani, Mohammad
Ali Cheraghi, Batool Tirgari
The
Effectiveness of Cognitive-Existential Group
Therapy on Reducing Existential Anxiety in the
Elderly
DOI: 10.5742/MEWFM.2017.93059
[pdf
version]
Somayeh Barekati, Bahman Bahmani, Maede Naghiyaaee,
Mahgam Afrasiabi, Roya Marsa
Post-mortem
Distribution of Morphine in Cadavers Body Fluids
DOI: 10.5742/MEWFM.2017.93060
[pdf
version]
Ramin Elmi, Mitra Akbari, Jaber Gharehdaghi,
Ardeshir Sheikhazadi, Saeed Padidar, Shirin
Elmi
Application
of Social Networks to Support Students' Language
Learning Skills in Blended Approach
DOI: 10.5742/MEWFM.2017.93061
[pdf
version]
Fatemeh Jafarkhani, Zahra Jamebozorg, Maryam
Brahman
The
Relationship between Chronic Pain and Obesity:
The Mediating Role of Anxiety
DOI: 10.5742/MEWFM.2017.93062
[pdf
version]
Leila Shateri, Hamid Shamsipour, Zahra Hoshyari,
Elnaz Mousavi, Leila Saleck, Faezeh Ojagh
Implementation
status of moral codes among nurses
DOI: 10.5742/MEWFM.2017.93063
[pdf
version]
Maryam Ban, Hojat Zareh Houshyari Khah, Marzieh
Ghassemi, Sajedeh Mousaviasl, Mohammad Khavasi,
Narjes Asadi, Mohammad Amin Harizavi, Saeedeh
Elhami
The comparison
of quality of life, self-efficacy and resiliency
in infertile and fertile women
DOI: 10.5742/MEWFM.2017.93064
[pdf version]
Mahya Shamsi Sani, Mohammadreza Tamannaeifar
Brain MRI Findings in Children (2-4 years old)
with Autism
DOI: 10.5742/MEWFM.2017.93055
[pdf
version]
Mohammad Hasan Mohammadi, Farah Ashraf Zadeh,
Javad Akhondian, Maryam Hojjati,
Mehdi Momennezhad
Reviews
TECTA gene function and hearing: a review
DOI: 10.5742/MEWFM.2017.93065
[pdf version]
Morteza Hashemzadeh-Chaleshtori, Fahimeh Moradi,
Raziyeh Karami-Eshkaftaki,
Samira Asgharzade
Mandibular
canal & its incisive branch: A CBCT study
DOI: 10.5742/MEWFM.2017.93066
[pdf
version]
Sina Haghanifar, Ehsan Moudi, Ali Bijani, Somayyehsadat
Lavasani, Ahmadreza Lameh
The
role of Astronomy education in daily life
DOI: 10.5742/MEWFM.2017.93067
[pdf
version]
Ashrafoalsadat Shekarbaghani
Human brain
functional connectivity in resting-state fMRI
data across the range of weeks
DOI: 10.5742/MEWFM.2017.93068
[pdf version]
Nasrin Borumandnia, Hamid Alavi Majd, Farid
Zayeri, Ahmad Reza Baghestani,
Mohammad Tabatabaee, Fariborz Faegh
International Health Affairs
A
brief review of the components of national strategies
for suicide prevention suggested by the World
Health Organization
DOI: 10.5742/MEWFM.2017.93069
[pdf
version]
Mohsen Rezaeian
Education and Training
Evaluating
the Process of Recruiting Faculty Members in
Universities and Higher Education and Research
Institutes Affiliated to Ministry of Health
and Medical Education in Iran
DOI: 10.5742/MEWFM.2017.93070
[pdf
version]
Abdolreza Gilavand
Comparison
of spiritual well-being and social health among
the students attending group and individual
religious rites
DOI: 10.5742/MEWFM.2017.93071
[pdf
version]
Masoud Nikfarjam, Saeid Heidari-Soureshjani,
Abolfazl Khoshdel, Parisa Asmand, Forouzan Ganji
A
Comparative Study of Motivation for Major Choices
between Nursing and Midwifery Students at Bushehr
University of Medical Sciences
DOI: 10.5742/MEWFM.2017.93072
[pdf
version]
Farzaneh Norouzi, Shahnaz Pouladi, Razieh Bagherzadeh
Clinical Research and Methods
Barriers
to the management of ventilator-associated pneumonia:
A qualitative study of critical care nurses'
experiences
DOI: 10.5742/MEWFM.2017.93073
[pdf version]
Fereshteh Rashnou, Tahereh Toulabi, Shirin Hasanvand,
Mohammad Javad Tarrahi
Clinical
Risk Index for Neonates II score for the prediction
of mortality risk in premature neonates with
very low birth weight
DOI: 10.5742/MEWFM.2017.93074
[pdf
version]
Azadeh Jafrasteh, Parastoo Baharvand, Fatemeh
Karami
Effect
of pre-colporrhaphic physiotherapy on the outcomes
of women with pelvic organ prolapse
DOI: 10.5742/MEWFM.2017.93075
[pdf
version]
Mahnaz Yavangi, Tahereh Mahmoodvand, Saeid Heidari-Soureshjani
The
effect of Hypertonic Dextrose injection on the
control of pains associated with knee osteoarthritis
DOI: 10.5742/MEWFM.2017.93076
[pdf
version]
Mahshid Ghasemi, Faranak Behnaz, Mohammadreza
Minator Sajjadi, Reza Zandi,
Masoud Hashemi
Evaluation
of Psycho-Social Factors Influential on Emotional
Divorce among Attendants to Social Emergency
Services
DOI: 10.5742/MEWFM.2017.93077
[pdf
version]
Farangis Soltanian
Models and Systems of Health Care
Organizational
Justice and Trust Perceptions: A Comparison
of Nurses in public and private hospitals
DOI: 10.5742/MEWFM.2017.93078
[pdf
version]
Mahboobeh Rajabi, Zahra Esmaeli Abdar, Leila
Agoush
Case series and Case reports
Evaluation
of Blood Levels of Leptin Hormone Before and
After the Treatment with Metformin
DOI: 10.5742/MEWFM.2017.93079
[pdf
version]
Elham Jafarpour
Etiology,
Epidemiologic Characteristics and Clinical Pattern
of Children with Febrile Convulsion Admitted
to Hospitals of Germi and Parsabad towns in
2016
DOI: 10.5742/MEWFM.2017.93080
[pdf
version]
Mehri SeyedJavadi, Roghayeh Naseri, Shohreh
Moshfeghi, Irandokht Allahyari, Vahid Izadi,
Raheleh Mohammadi,
Faculty development
The
comparison of the effect of two different teaching
methods of role-playing and video feedback on
learning Cardiopulmonary Resuscitation (CPR)
DOI: 10.5742/MEWFM.2017.93081
[pdf
version]
Yasamin Hacham Bachari, Leila Fahkarzadeh, Abdol
Ali Shariati
Office based family medicine
Effectiveness
of Group Counseling With Acceptance and Commitment
Therapy Approach on Couples' Marital Adjustment
DOI: 10.5742/MEWFM.2017.93082
[pdf
version]
Arash Ziapour, Fatmeh Mahmoodi, Fatemeh Dehghan,
Seyed Mehdi Hoseini Mehdi Abadi,
Edris Azami, Mohsen Rezaei
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| October 2017 -
Volume 15, Issue 8 |
|
|
Evaluation of Blood Levels
of Leptin Hormone Before and After the Treatment
with Metformin
Elham Jafarpour
MSc of Biochemistry, Payam-e Noor University,
Iran
Correspondence:
Elham
Jafarpour
Payam-e Noor University, Iran
|
Abstract
The
purpose of this study was to evaluate
the blood level of leptin hormone before
and after treatment with metformin. This
research is a pre-test and post-test type.
The statistical population in this study
is 50 patients with type 2 diabetes who
referred to Ghods specialized polyclinic
in 2017. Patients with type 2 diabetes
and BMI> 35 were enrolled. Each patient
received 1000 mg of metformin twice daily
for 2 months in a pill form, and a blood
sample was taken before and after taking
the drug and frozen at -20 ° C and,
at the time of sampling, to room temperature
delivered and measured. Glucose, total
cholesterol, triglyceride, cholesterol
and cholesterol were measured by common
laboratory methods. HbA1c was measured
by ion exchange chromatography using the
Drew-DS5-UK device. Blood insulin concentration
in patients was measured by sandwich ELISA
method. Leptin was measured using the
sandwich ELISA method. The findings of
the study also indicated that body weight,
BMI, FFM / Kg, FM / Kg before and after
treatment were not significantly different.
There was no significant difference between
the mean of leptin hormone levels in the
pre- and post-test, and there was no significant
difference with the concentration of insulin
hormone either. But the mean glucose concentration
before and after treatment was statistically
significant (p <0.05). Also, the results
indicated that the effect of drug use
in pre-test and post-test on the level
of cholesterol, triglyceride and LDL cholesterol
levels in the patients was significantly
different. In this study, the effect of
metformin during the treatment period
reduced the blood glucose level of individuals,
but its effect on weight loss and HbA1c
did not significantly increase due to
the duration of treatment.
Key words:
Leptin, Metformin, Diabetes.
|
Obesity is a major public health problem in
developed countries. Today, the prevalence of
obesity is increasing in developing countries,
due to changes in lifestyle, modernization and
urbanization. Body mass index (BMI) is a numeric
measure that measures the rate of obesity by
using weight and height data. BMI does not directly
measure body fat, but research has shown that
BMI is directly related to body fat (Pevester,
2010). According to the hypothesis of lipostat,
that is the leading indicator of the relative
stability of body weight, there is a mechanism
of post-tracing (negative control) to control
eating behavior and increase energy consumption
when the body weight gain is of a certain degree
(adjustment point); such inhibitory effect will
stop when the body weigh falls below this regulatory
point (Lindel, 2008). This hypothesis predicts
the existence of a post-traumatic message that
originates from fat tissue and acts on the brain’s
control of eating habits and activity. Such
an agent was discovered in 1994, and leptin
was named. Leptin, a hormone suppressor of eating
behaviors when sufficient sources of triacylglycerol
were stored, was found to be a factor in the
blood of natural mice that, with the elimination
of leptin deficiencies, reversed the behavior
of the bulky mutated rats (Montsours, 2011).
These mutated rats were obese due to overeating,
but their body weight was reduced by injection
of leptin (Graham, 2012). There are also many
causes for obesity, among them physiological
causes play a more important role in this regard,
with the Kennedy theory of liposuction in 1953
(Brenin, 2008). Based on this theory, fat tissue
builds up a substance to regulate body composition,
a theory that led to the discovery of a gene
that later became known as the “Obesity
Gene”. This gene is called leptin, and
was discovered in 1994 by Zang et al. Leptin
comes from a Greek word Leptos, meaning “lean”,
but it’s a bit more complicated than trying
to interpret it as leptin is less than fat.
Leptin is a hormone that controls appetite and
body weight. This hormone is made up of fat
cells and sends messages to the brain about
how much energy is available to a person. The
more fat cells a person has, the more leptin
they will have. It seems that when the leptin
is not secreted, the brain thinks that there
is no fat in the body and it stimulates the
person to eat more and accumulate fat (Enfonds,
2014). The coordination of metabolism in various
tissues of a mammal is done by the neuroendocrine
system. Adjustment of this system is performed
in such a way that separate cells in a tissue
sense a change in the current condition and
respond by secreting an extracellular chemical
message and this message, after attaching to
the receptor molecule in another cell, that
causes a change in that cell. The hypothalamus
of the brain is the center of the neuroendocrine
system. Some regulatory mechanisms operate on
a very long-term basis and control nutrition
and energy consumption in a manner that maintains
the body of mammals in a state of equilibrium.
A partial imbalance in weight gain can put life
at risk. When fat tissue forms a large part
of the total body mass, life expectancy decreases.
As a result, there is a lot of interest today
in researching how to adjust body size and fat
content. Leptin was identified as a product
of a gene that was shown in laboratory mice
with OB (abbreviated to obese, meaning obese).
Mice with two defective versions of the gene
(ob / ob genotype) indicate the behavior and
physiology of animals is in a steady state of
hunger: The levels of cortication hormones increase.
They are not able to withstand heat, they grow
naturally and their appetite is maintained.
Due to the latter case, these mice are highly
obese and their weight is 3 times higher than
normal mice. These mice also have metabolic
disorders such as diabetic animals and cannot
use insulin (Robbins, 2010). By leptin injection
into mutated mice (ob / ob), their weight decreased
and locomotor activity increased and their heat
production increased. The second gene of the
mouse, also labeled DB (for diabetes), has been
found in the regulation of appetite. Mice with
two defective versions of the gene (db / db)
are obese and diabetic. It is known that the
DB gene is responsible for coding the receptor
for leptin. Leptin activity does not appear
when the leptin receptor fails. Leptin is produced
only in fat cells and less in the intestinal
epithelium and in pairs (Chen, 2013). Leptin
receptors are expressed principally in the regions
of the brain, including the arcuate nucleus
neurons, and the hypothalamic ventromedal, that
play a role in regulating eating behavior. This
receptor is also expressed in the corpuscular
cells of the adrenal glands and the beta panacea
cells, albeit at a low level. Leptin carries
a message that fat deposits are sufficient and
fuel consumption is reduced and energy consumption
is rising. Leptin reciprocating with its receptor
in the hypothalamus changes the release of an
effect on appetite. Leptin also stimulates the
sympathetic nervous system and thereby increases
blood pressure, heart rate and heat production
(producing heat at the expense of metabolic
energy) by separating electron transport from
ATP synthesis in mitochondria of fat tissue
(Yang, 2009). The common model of leptin is
a cascade of regulatory events that interact
with the interaction of leptin and its receptor
and affects the amount of hormones that stimulate
or inhibit eating and energy consumption. The
amount of leptin released from fat tissue depends
on the number and size of fat cells. The leptin
that connects to the receptor is as following:
The receptor of leptin has a single piece of
protein that is circulating in the membrane
that is dipped to the outer side by binding
leptin. Both monomers of this dimer receptor
are phosphorylated by a kinase enzyme. These
phosphorous portions act as binding sites for
three proteins that are message transducers
and transcription activators. Then these three
proteins are phosphorylated by the same kinase.
Message transducers and transcriptional activators
go to the cell nucleus after phosphorylation
by kinase and, by binding specific DNA sequences,
stimulate the expression of specific target
genes. Eventually, the products of these genes
affect the nutritional behavior of energy. One
of the products of these genes is the -melanocyte
stimulating hormone that acts as an appetite
suppressor. The increase in catabolism and the
production of heat by leptin is due in part
to the increase of the u.p-1 mitochondrial protein
in fat cells. Leptin stimulates the synthesis
of ucp-1 by altering synaptic transmission of
neurons in the arcoat core and hybridization
of some hypothalamic neurons. With the creation
of a channel, the ucp-1 protein increases the
entry of protons into the mitochondrial matrix
without passing through the synthase ATP complex.
This prevents the oxidation of fuels (fatty
acids inside a fat cell) without the synthesis
of ATP and releases energy in the form of heat,
thus consuming calories or stored fats in large
amounts (Freelit, 2010). Metformin is a type
2 diabetes regulator. Metformin has a cell-mediated
sensitivity to insulin and anti-hyperglycemia,
and is used to treat insulin in Non-Insulin-dependent
diabetes mellitus (NIDDM). The precise mechanism
of metformin has not been identified, but one
of the proposed actions is the clearance of
peripheral glucose in low insulin concentrations.
Studies indicate that obesity in adults with
metformin with type 2 diabetes leads to weight
loss, and glucose tolerance and fat stores are
corrected. Metformin mainly effects its anti-hyperglycemic
effect by reducing glucose output through inhibition
of gluconeogenesis. Additionally, the use of
metformin in non-diabetic obese adults leads
to reduced intake of food and weight loss along
with a decrease in glucose, lipids, and insulin
in fasting conditions. There are reports that
metformin, in addition to the above effects,
also reduces plasma leptin levels and fat stores
(Jinjirik, 2012).
The current study, based on the purpose of
the applied type and based on its nature, is
a type of pre-test and post-test. The statistical
population in this study is type II diabetic
patients (including adolescent and youth) referring
to Ghods specialized polyclinic in 2012, that
is 50 people. In this research, using a simple
random sampling method, due to the wide extent
of the statistical society and the impossibility
of conducting research on the whole society,
has been used. Patients with type 2 diabetes
and BMI> 35 were enrolled. Each patient received
1000 mg of metformin twice daily for 2 months
in a pill from, and a blood sample was taken
before and after taking the drug and frozen
at -20 ° C and, at the time of sampling,
to room temperature, delivered and measured.
Glucose, total cholesterol, triglyceride, cholesterol
and cholesterol were measured by common laboratory
methods. HbA1c was measured using a Drew-DS5-UK
device using ion exchange chromatography. Blood
insulin concentration in patients was measured
using Sandwich Elise method. Leptin was measured
using the sandwich ELISA method. The results
of the measured factors were expressed as mean
and standard deviation. For statistical analysis,
the results of glucose, blood lipids and HbA1c,
and leptin and insulin, as well as body weight,
BMI, body fat mass, and FFM body mass index
from T was used.
Blood leptin hormone levels were measured in
the two experimental groups. The results indicated
that the mean of this hormone was 6.5 g / ml
± 3.3 g / ml. Also, the amount of insulin
was 27.1 ± 28.11 IU / mL. And the mean
glucose was 159 mg / dl. Finally, glycosylated
hemoglobin was 7.5%. The results indicate an
inverse relationship between leptin and insulin
showing this difference and the correlation
between leptin and insulin, glucose, HbA1c,
cholesterol and triglyceride, and BMI in the
current study.
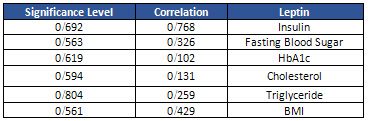
Table 1 indicates the correlation between leptin
and insulin, glucose, HbA1c, cholesterol, triglyceride
and BMI.
Table 1: Correlation between research variables
Also, to evaluate the effect of metformin on
weight factors, scores were compared before
and after treatment. The results are shown in
Table 2.
Table 2: Scores of individuals’ weight
factors in pre and post tests
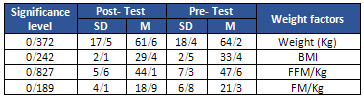
As shown in Table 2, body weight, BMI, FFM
/ Kg, FM / Kg before and after treatment were
not significantly different. Also, to evaluate
the effect of metformin on biochemical and metabolic
factors in pre and post test (Table 3).
Table 3: Scores of biochemical parameters
in pre and post tests
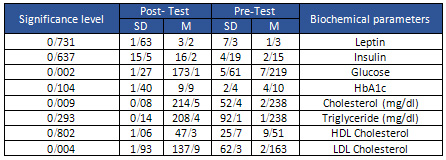
The results indicated that the mean of leptin
hormone levels in pre- and post-test, as well
as the concentration of insulin hormone was
not significantly different. However, the mean
of glucose concentration before and after treatment
indicated a statistically significant difference
(p <0.05). Also, the effect of drug use in
pre-test and post-test on the level of cholesterol,
triglyceride and LDL cholesterol in patients
was significantly different. Correlation analysis
was also used to assess the relationship between
leptin and biochemical parameters. The results
are shown in Table 4.
Table 4: Correlation between leptin with biochemical
parameters
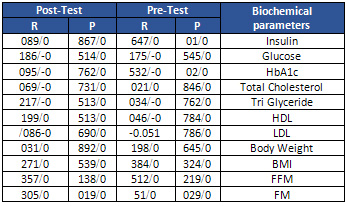
The results of Table 4 indicated that there
was no significant relationship between leptin
of blood and any of the biocompatibility parameters.
| DISCUSSION
AND
CONCLUSION
|
Obesity
is
a
complex
complication
characterized
by
excessive
accumulation
of
fat
tissue.
Obesity
is
associated
with
many
health
problems,
including
vascular
diseases.
The
discovery
of
leptin
hormone
has
led
to
further
research
on
obesity.
The
main
reason
for
this
progress
was
that
it
indicated
that
the
fat
tissue
of
the
signals
is
transmitted
to
the
central
nervous
system.
The
Leptin
produced
by
the
obesity
gene
is
a
protein
hormone
with
a
molecular
weight
of
16
kDa,
which
is
mainly
secreted
from
fat
tissue,
and
has
a
key
role
in
regulating
body
weight.
It
is
better
to
say
that
leptin
acts
as
a
warning
mechanism
for
regulating
body
fat.
This
hormone
increases
energy
consumption
by
increasing
the
activity
of
the
sympathetic
nervous
system
and
lipolysis.
Leptin
also
inhibits
appetite
by
influencing
hypothalamic
receptors.
Therefore,
the
net
effect
of
leptin
is
to
reduce
weight,
but
deficiency
of
the
hormones
or
resistance
to
its
effects
can
both
lead
to
weight
gain.
Leptin
resistance,
that
is
associated
with
its
increase
in
blood,
is
much
more
common
in
human
obesity
than
the
deficiency
of
this
hormone.
In
recent
years,
numerous
studies
have
been
conducted
on
the
association
of
leptin
with
arterial
hypertension
and
heart
rate.
Leptin
independent
of
CRP,
that
is
an
inflammatory
marker,
is
associated
with
vascular
disease,
and
this
finding
points
to
the
importance
of
body
fat
in
cardiovascular
problems
(Astling,
2011).
Leptin
receptors
are
on
the
endothelium
wall
and
smooth
vascular
muscle
cells.
For
this
reason,
leptin
imposes
intermediate
is
effective
on
ability
and
vascular
growth.
At
the
cellular
level,
leptin
stimulates
smooth
muscle
for
proliferation.
Vascular
calcification
is
accelerated
by
leptin
in
empirical
models.
This
hormone
increases
the
oxidative
pressure
in
the
vascular
wall,
which
can
damage
them.
Therefore,
as
a
general
conclusion,
it
can
be
concluded
that
leptin
levels
in
blood
are
related
to
cardiovascular
health
(Thomas,
2014).
The
findings
also
indicated
that
body
weight,
BMI,
FFM
/
Kg,
FM
/
Kg
before
and
after
treatment
were
not
significantly
different.
The
results
of
the
study
indicated
that
the
mean
of
leptin
hormone
levels
in
pre-
and
post-test
patients,
as
well
as
in
the
concentration
of
hormone
insulin
no
significant
difference
was
found.
But
the
mean
glucose
concentration
before
and
after
treatment
was
statistically
significant
(p
<0.05).
Also,
the
results
indicated
that
the
effect
of
drug
use
in
pre-test
and
post-test
on
the
level
of
cholesterol,
triglyceride
and
LDL
cholesterol
levels
in
the
patients
was
significantly
different.
In
this
study,
the
effect
of
metformin
during
the
treatment
period
reduced
the
blood
glucose
level
of
individuals,
but
its
effect
on
weight
loss
and
HbA1c
did
not
significantly
increase
due
to
the
duration
of
treatment.
Various
studies
have
shown
that
the
effect
of
metformin
has
significantly
reduced
blood
lipids,
which
is
consistent
with
the
recent
study
that
indicated
that
cholesterol
and
triglyceride
and
LDL
cholesterol
decreased
after
treatment.
These
findings
suggest
that
the
drug
has
an
effect
on
metabolic
pathways
in
addition
to
glucose
lowering
the
lipids
in
these
patients.
Most
studies
have
shown
that
a
balanced,
low-fat
diet
and
physical
activity
reduce
levels
of
leptin
in
the
blood,
even
if
no
significant
weight
loss
occurs.
Reduced
leptin
levels
through
exercise,
changes
in
energy
balance,
improved
insulin
sensitivity
and
changes
in
blood
lipids
are
appropriate.
The
study
of
changes
in
leptin
with
physical
activity
is
one
of
the
issues
that
is
especially
important
in
adolescent
and
youth
obesity.
At
the
same
time,
there
are
still
no
other
risk
factors
for
vascular
diseases,
while
many
studies
point
to
the
onset
of
dryness
and
vascular
trauma
in
adolescents.
Pellestor
F.,
Andreo
B.,
Arnal
F.,
Humeau
C.,
Demaille
J.
Maternal
aging
and
chromosomal
abnormalities:
new
data
drawn
from
in
vitro
unfertilized
human
oocytes.
Hum
Genet.
2010;112(2):
195-203.
Lindell
K.,
Svensson
E.,
Bergh
C.,
Lind
P.,
et
al.
Expression
of
functional
leptin
receptors
in
the
human
ovary.
J
Clin
Endocrinol
Metab.
2008;82(12):
4144-8.
Mantzoros
C.S.,
Cramer
D.W.
Liberman
R.F.,
Barbieri
R.L.
Predictive
value
of
serum
and
follicular
fluid
leptin
concentrations
during
assisted
reproductive
cycles
in
normal
women
and
in
women
with
the
polycystic
ovarian
syndrome.
Hum
Reprod.
2011;15(3):539-44.
Graham
L.,
Danforth
D.,
et
al.
Vascular
endothelial
growth
factor,
nitric
oxide,
and
leptin
follicular
fluid
levels
correlate
negatively
with
embryo
quality
in
IVF
patients.
Fertil
Steril.
2012;72(6):1024-6.
Brannian
J.D.,
Schmidt
S.M.,
Kreger
D.O.,
Hansen
K.A.
Baseline
non-fasting
serum
leptin
concentration
to
body
mass
index
ratio
is
predictive
of
IVF
outcomes.
Hum
Reprod.
2001;
16(9):1819-26.
Anifandis
G.,
Koutselini
E.,
Louridas
K.,
Liakopoulos
V.,
Leivaditis
K.,
et
al.
Estradiol
and
leptin
as
conditional
prognostic
IVF
markers.
Reproduction.
2014;
129(4):531-4.
Robins
J.C.,
Srivastava
R.,
Mershon
J.L.,
Thomas
M.A.
Association
of
leptin
with
poor
ovarian
stimulation
during
in
vitro
fertilization.
J
Reprod
Med.
2005;
50(5):356-60.
Chen
R.,
Fisch
B.,
Ben-Haroush
A.,
Kaplan
B.,
Hod
M.,
Orvieto
R.
Serum
and
follicular
fluid
leptin
levels
in
patients
undergoing
controlled
ovarian
hyperstimulation
for
in
vitro
fertilization
cycle.
Clin
Exp
Obstet
Gynecol.
2013;
31(2):103-6.
Yang
X.F.,
Huang
H.F.
Impact
of
leptin
levels
on
outcome
of
in
vitro
fertilization-
embryo
transfer.
Zhejiang
Da
Xue
Xue
Bao
Yi
Xue
Ban.
2009;31(3):
155-158.Chinese.
Frelut,
M.L,
Childhood
obesity:
from
clinics
to
leptin,
Int.
J.
Obes.
Relat.
Metab.
Disord.
2010,
21
(Suppl.2):
5137.
Ma
Z,
Gingerich
RL,
Santiago
JV,
Klein
S,
Smith
CH,
and
Landt
M,
Radioimmunoassay
of
leptin
in
human
plasma,
Clin.
Chern.
2012;
42:
942.
Stehling
0,
Doring
H,
Ertl
J,
Preibisch
G,
and
Schmidt
I,
Leptin
reduces
juvenile
fat
stores
by
altering
the
circadian
cycle
of
energy
expenditure,
Am.
J.
Physiol
2011;
271,
Rl170.
Tumas
MEA,
Duncan
JS,
and
Rayner
DV.
Effect
of
fasting
and
refeeding
on
Ob
gene
expression
in
white
adipose
tissue
of
lean
and
obese
mice,
FFBS
Let,
2014;
365:488-90.
|
|
.................................................................................................................

|
| |
|

