|
|
 |
| ............................................................. |
|
October 2017 -
Volume 15, Issue 8
|
 |
|
View
this issue in pdf formnat - the issue
has been split into two files for downloading
due to its large size: FULLpdf
(12 MB)
Part
1 &
Part
2
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
........................................................
|
|
Original Contribution/Clinical Investigation
Immunity
level to diphtheria in beta thalassemia patients
DOI: 10.5742/MEWFM.2017.93048
[pdf
version]
Abdolreza Sotoodeh Jahromi, Karamatollah Rahmanian,
Abdolali Sapidkar, Hassan Zabetian, Alireza
Yusefi, Farshid Kafilzadeh, Mohammad Kargar,
Marzieh Jamalidoust,
Abdolhossein Madani
Genetic
Variants of Toll Like Receptor-4 in Patients
with Premature Coronary Artery Disease, South
of Iran
DOI: 10.5742/MEWFM.2017.93049
[pdf
version]
Saeideh Erfanian, Mohammad Shojaei, Fatemeh
Mehdizadeh, Abdolreza Sotoodeh Jahromi, Abdolhossein
Madani, Mohammad Hojjat-Farsangi
Comparison
of postoperative bleeding in patients undergoing
coronary artery bypass surgery in two groups
taking aspirin and aspirin plus CLS clopidogrel
DOI: 10.5742/MEWFM.2017.93050
[pdf
version]
Ali Pooria, Hassan Teimouri, Mostafa Cheraghi,
Babak Baharvand Ahmadi, Mehrdad Namdari, Reza
Alipoor
Comparison
of lower uterine segment thickness among nulliparous
pregnant women without uterine scar and pregnant
women with previous cesarean section: ultrasound
study
DOI: 10.5742/MEWFM.2017.93051
[pdf version]
Taravat Fakheri, Irandokht Alimohammadi, Nazanin
Farshchian, Maryam Hematti,
Anisodowleh Nankali, Farahnaz Keshavarzi, Soheil
Saeidiborojeni
Effect
of Environmental and Behavioral Interventions
on Physiological and Behavioral Responses of
Premature Neonates Candidates Admitted for Intravenous
Catheter Insertion in Neonatal Intensive Care
Units
DOI: 10.5742/MEWFM.2017.93052
[pdf
version]
Shohreh Taheri, Maryam Marofi, Anahita Masoumpoor,
Malihe Nasiri
Effect
of 8 weeks Rhythmic aerobic exercise on serum
Resistin and body mass index of overweight and
obese women
DOI: 10.5742/MEWFM.2017.93053
[pdf
version]
Khadijeh Molaei, Ahmad Shahdadi, Reza Delavar
Study
of changes in leptin and body mass composition
with overweight and obesity following 8 weeks
of Aerobic exercise
DOI: 10.5742/MEWFM.2017.93054
[pdf
version]
Khadijeh Molaei, Abbas Salehikia
A reassessment
of factor structure of the Short Form Health
Survey (SF-36): A comparative approach
DOI: 10.5742/MEWFM.2017.93088
[pdf version]
Vida Alizad, Manouchehr Azkhosh, Ali Asgari,
Karyn Gonano
Population and Community Studies
Evaluation
of seizures in pregnant women in Kerman - Iran
DOI: 10.5742/MEWFM.2017.93056
[pdf
version]
Hossein Ali Ebrahimi, Elahe Arabpour, Kaveh
Shafeie, Narges Khanjani
Studying
the relation of quality work life with socio-economic
status and general health among the employees
of Tehran University of Medical Sciences (TUMS)
in 2015
DOI: 10.5742/MEWFM.2017.93057
[pdf version]
Hossein Dargahi, Samereh Yaghobian, Seyedeh
Hoda Mousavi, Majid Shekari Darbandi, Soheil
Mokhtari, Mohsen Mohammadi, Seyede Fateme Hosseini
Factors
that encourage early marriage and motherhood
from the perspective of Iranian adolescent mothers:
a qualitative study
DOI: 10.5742/MEWFM.2017.93058
[pdf
version]
Maasoumeh Mangeli, Masoud Rayyani, Mohammad
Ali Cheraghi, Batool Tirgari
The
Effectiveness of Cognitive-Existential Group
Therapy on Reducing Existential Anxiety in the
Elderly
DOI: 10.5742/MEWFM.2017.93059
[pdf
version]
Somayeh Barekati, Bahman Bahmani, Maede Naghiyaaee,
Mahgam Afrasiabi, Roya Marsa
Post-mortem
Distribution of Morphine in Cadavers Body Fluids
DOI: 10.5742/MEWFM.2017.93060
[pdf
version]
Ramin Elmi, Mitra Akbari, Jaber Gharehdaghi,
Ardeshir Sheikhazadi, Saeed Padidar, Shirin
Elmi
Application
of Social Networks to Support Students' Language
Learning Skills in Blended Approach
DOI: 10.5742/MEWFM.2017.93061
[pdf
version]
Fatemeh Jafarkhani, Zahra Jamebozorg, Maryam
Brahman
The
Relationship between Chronic Pain and Obesity:
The Mediating Role of Anxiety
DOI: 10.5742/MEWFM.2017.93062
[pdf
version]
Leila Shateri, Hamid Shamsipour, Zahra Hoshyari,
Elnaz Mousavi, Leila Saleck, Faezeh Ojagh
Implementation
status of moral codes among nurses
DOI: 10.5742/MEWFM.2017.93063
[pdf
version]
Maryam Ban, Hojat Zareh Houshyari Khah, Marzieh
Ghassemi, Sajedeh Mousaviasl, Mohammad Khavasi,
Narjes Asadi, Mohammad Amin Harizavi, Saeedeh
Elhami
The comparison
of quality of life, self-efficacy and resiliency
in infertile and fertile women
DOI: 10.5742/MEWFM.2017.93064
[pdf version]
Mahya Shamsi Sani, Mohammadreza Tamannaeifar
Brain MRI Findings in Children (2-4 years old)
with Autism
DOI: 10.5742/MEWFM.2017.93055
[pdf
version]
Mohammad Hasan Mohammadi, Farah Ashraf Zadeh,
Javad Akhondian, Maryam Hojjati,
Mehdi Momennezhad
Reviews
TECTA gene function and hearing: a review
DOI: 10.5742/MEWFM.2017.93065
[pdf version]
Morteza Hashemzadeh-Chaleshtori, Fahimeh Moradi,
Raziyeh Karami-Eshkaftaki,
Samira Asgharzade
Mandibular
canal & its incisive branch: A CBCT study
DOI: 10.5742/MEWFM.2017.93066
[pdf
version]
Sina Haghanifar, Ehsan Moudi, Ali Bijani, Somayyehsadat
Lavasani, Ahmadreza Lameh
The
role of Astronomy education in daily life
DOI: 10.5742/MEWFM.2017.93067
[pdf
version]
Ashrafoalsadat Shekarbaghani
Human brain
functional connectivity in resting-state fMRI
data across the range of weeks
DOI: 10.5742/MEWFM.2017.93068
[pdf version]
Nasrin Borumandnia, Hamid Alavi Majd, Farid
Zayeri, Ahmad Reza Baghestani,
Mohammad Tabatabaee, Fariborz Faegh
International Health Affairs
A
brief review of the components of national strategies
for suicide prevention suggested by the World
Health Organization
DOI: 10.5742/MEWFM.2017.93069
[pdf
version]
Mohsen Rezaeian
Education and Training
Evaluating
the Process of Recruiting Faculty Members in
Universities and Higher Education and Research
Institutes Affiliated to Ministry of Health
and Medical Education in Iran
DOI: 10.5742/MEWFM.2017.93070
[pdf
version]
Abdolreza Gilavand
Comparison
of spiritual well-being and social health among
the students attending group and individual
religious rites
DOI: 10.5742/MEWFM.2017.93071
[pdf
version]
Masoud Nikfarjam, Saeid Heidari-Soureshjani,
Abolfazl Khoshdel, Parisa Asmand, Forouzan Ganji
A
Comparative Study of Motivation for Major Choices
between Nursing and Midwifery Students at Bushehr
University of Medical Sciences
DOI: 10.5742/MEWFM.2017.93072
[pdf
version]
Farzaneh Norouzi, Shahnaz Pouladi, Razieh Bagherzadeh
Clinical Research and Methods
Barriers
to the management of ventilator-associated pneumonia:
A qualitative study of critical care nurses'
experiences
DOI: 10.5742/MEWFM.2017.93073
[pdf version]
Fereshteh Rashnou, Tahereh Toulabi, Shirin Hasanvand,
Mohammad Javad Tarrahi
Clinical
Risk Index for Neonates II score for the prediction
of mortality risk in premature neonates with
very low birth weight
DOI: 10.5742/MEWFM.2017.93074
[pdf
version]
Azadeh Jafrasteh, Parastoo Baharvand, Fatemeh
Karami
Effect
of pre-colporrhaphic physiotherapy on the outcomes
of women with pelvic organ prolapse
DOI: 10.5742/MEWFM.2017.93075
[pdf
version]
Mahnaz Yavangi, Tahereh Mahmoodvand, Saeid Heidari-Soureshjani
The
effect of Hypertonic Dextrose injection on the
control of pains associated with knee osteoarthritis
DOI: 10.5742/MEWFM.2017.93076
[pdf
version]
Mahshid Ghasemi, Faranak Behnaz, Mohammadreza
Minator Sajjadi, Reza Zandi,
Masoud Hashemi
Evaluation
of Psycho-Social Factors Influential on Emotional
Divorce among Attendants to Social Emergency
Services
DOI: 10.5742/MEWFM.2017.93077
[pdf
version]
Farangis Soltanian
Models and Systems of Health Care
Organizational
Justice and Trust Perceptions: A Comparison
of Nurses in public and private hospitals
DOI: 10.5742/MEWFM.2017.93078
[pdf
version]
Mahboobeh Rajabi, Zahra Esmaeli Abdar, Leila
Agoush
Case series and Case reports
Evaluation
of Blood Levels of Leptin Hormone Before and
After the Treatment with Metformin
DOI: 10.5742/MEWFM.2017.93079
[pdf
version]
Elham Jafarpour
Etiology,
Epidemiologic Characteristics and Clinical Pattern
of Children with Febrile Convulsion Admitted
to Hospitals of Germi and Parsabad towns in
2016
DOI: 10.5742/MEWFM.2017.93080
[pdf
version]
Mehri SeyedJavadi, Roghayeh Naseri, Shohreh
Moshfeghi, Irandokht Allahyari, Vahid Izadi,
Raheleh Mohammadi,
Faculty development
The
comparison of the effect of two different teaching
methods of role-playing and video feedback on
learning Cardiopulmonary Resuscitation (CPR)
DOI: 10.5742/MEWFM.2017.93081
[pdf
version]
Yasamin Hacham Bachari, Leila Fahkarzadeh, Abdol
Ali Shariati
Office based family medicine
Effectiveness
of Group Counseling With Acceptance and Commitment
Therapy Approach on Couples' Marital Adjustment
DOI: 10.5742/MEWFM.2017.93082
[pdf
version]
Arash Ziapour, Fatmeh Mahmoodi, Fatemeh Dehghan,
Seyed Mehdi Hoseini Mehdi Abadi,
Edris Azami, Mohsen Rezaei
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| October 2017 -
Volume 15, Issue 8 |
|
|
Comparison of postoperative
bleeding in patients undergoing coronary artery
bypass surgery in two groups taking aspirin
and aspirin plus CLS clopidogrel
Ali Pooria
(1)
Hassan Teimouri (2)
Mostafa Cheraghi (3)
Babak Baharvand Ahmadi (3)
Mehrdad Namdari (3)
Reza Alipoor (4)
(1) Assistant Professor, Department of General
Surgery, Lorestan University of Medical Sciences,
Khorramabad, Iran
(2) Associated Professor, Department of Anesthesiology,
Lorestan University of Medical Sciences, Khorramabad,
Iran
(3) Assistant Professor, Department of Cardiology,
Lorestan University of Medical Sciences, Khorramabad,
Iran
(4) Student research committee, Fasa University
of medical sciences, Fasa, Iran
Correspondence:
Mostafa Cheraghi
Address: Department of clinical training, Shohada
Ashayer hospital, Enqelab St, Khorramabad, Lorestan,
Iran
Tel/ Fax: +98-6633203004
|
Abstract
Introduction: Coronary
Artery Bypass Grafting (CABG) is a surgical
procedure that aims to ease symptoms and
reduce the risk of death in patients with
coronary artery occlusion. In this surgery,
healthy blood vessels from other parts
of the body replace occluded coronary
arteries. This surgery is done to improve
blood supply to the heart. Because of
its invasive nature, this procedure is
associated with complications including
postoperative bleeding.
Methods:
The study included 68 subjects in each
group. The inclusion criteria were age
of 40-80 years, serum creatinine under
1.5 mg/dl, platelet count above 100 thousand
per microliter, hemoglobin above 8 g per
deciliter, and normal PT and PTT. The
patients underwent the procedure through
the on-pump method. The study population
included the patients undergoing CABG
in Khorramabad Heart Hospital. The convenience,
consecutive sampling method was applied,
based on the inclusion criteria of the
study.
Results: The mean age of the patients
treated with aspirin was 60.9 ±
11.05, and the mean age of the patients
treated with aspirin plus clopidogrel
was 60.48 ± 9.8 years. The mean
FFP intake in the aspirin plus clopidogrel
group during hospitalization was significantly
higher than the mean in the aspirin group
(PV= 0.0009). The mean cell pack intake
in the aspirin plus clopidogrel group
during hospitalization was higher than
the mean in the aspirin group, but this
difference was not statistically significant
(PV=0.068)
Discussion: The rate of postoperative
bleeding in the clopidogrel plus aspirin
group was higher than the rate in the
aspirin group, but this difference was
not significant (PV=0.067). The rate of
Hb, HCT, and platelets in the aspirin
plus clopidogrel group at discharge was
higher than the rate in the aspirin group,
which was due to excess bleeding in the
aspirin plus clopidogrel group compared
to the aspirin group. The rate of FFP
intake in the aspirin plus clopidogrel
group was significantly higher than the
rate in the aspirin group, which was due
to excess bleeding in the aspirin plus
clopidogrel group (PV=0.0009).
Key words:
coronary artery bypass grafting, aspirin,
clopidogrel
|
Coronary artery bypass grafting (CABG) is a
surgical procedure that aims to ease symptoms
and reduce the risk of death in patients with
coronary artery occlusion. In these patients,
healthy vessels of other parts of the body are
grafted to replace the occluded coronary arteries
and this improves blood flow to the heart. Due
to the aggressive and invasive nature of this
surgery, it is associated with complications.
From among the complications of this surgery,
bleeding after CABG can be cited. The prevalence
of this complication is so high that 17% of
patients need blood transfusions after surgery
and approximately 3 to 5 percent of patients
require re-exploration (1). The amount of bleeding
after surgery varies based on factors such as
platelet count and pre-operative fibrinogen
concentrations (1). Also, it should be noted
that patients undergoing CABG often use antiplatelet
and anticoagulant drugs due to heart disease
and this issue affects the occurrence and severity
of postoperative bleeding. It is expected that
various antiplatelet drugs have different effects
on post-operative bleeding. One of the drugs
that nowadays is used as an antiplatelet drug
is clopidogrel. This medication irreversibly
inhibits platelet activation and aggregation
(2). Various studies conducted on the effects
of this drug on CABG post-operative bleeding
have reported mixed results. Several studies
have reported that the use of this drug has
no effect on the amount of post-operative bleeding
(3). In contrast, some studies have reported
that the use of this drug increases the rate
of postoperative bleeding (4-6). In addition,
it has been reported that the preoperative use
of clopidogrel with a loading dose of 600 mg
increases the risk of bleeding in comparison
with a loading dose of 300 mg (7). On the other
hand, the use of clopidogrel in patients undergoing
CABG shows benefits, which include a decline
in the rates of cardiovascular events (5) and
a reduction in the likelihood of replaced vessel
occlusion (3).
In this study, considering the benefits that
have been proposed for the use of clopidogrel
plus aspirin in patients undergoing CABG, and
also given the mixed results obtained from different
studies, we decided to compare postoperative
bleeding in patients undergoing coronary artery
bypass surgery in two groups taking aspirin
and aspirin plus clopidogrel.
In this study, the number of subjects in each
group was 68 patients. The inclusion criteria
included an age of between 40 and 80 years,
serum creatinine levels less than 1.5 mg/dl,
a platelet count of over 100 thousand per microliter,
hemoglobin levels of more than 8 g per dl, and
normal PT and PTT, and the use of the on-pump
CABG for the patients. The studied population
included patients who had undergone CABG in
the Specialist Cardiac Hospital of Khorramabad,
Iran. The convenience and consecutive sampling
methods were used based on the inclusion criteria
of the study.
In this study, candidate patients for angiography
underwent coronary angiography by two groups
of cardiologists. One group were specialists
who were able to perform angioplasty and the
other group was not able to perform this operation.
Cardiologists who were not able to perform angioplasty
prescribed aspirin (325 mg daily) for patients
scheduled to undergo angiography. In contrast,
given the fact that patients who are scheduled
to undergo coronary angiography may need angioplasty
too, cardiologists who were able to perform
angioplasty prescribed clopidogrel (with a dose
of 600mg per day) in addition to aspirin (with
a dose of 325mg) for the patients to be ready
to undergo angioplasty, if necessary. The advantage
of this strategy is that it spares the patient
from another procedure to perform angioplasty.
In both groups, if the findings of angiography
showed that some patients needed to undergo
CABG, cardiac surgeons subsequently operated
on them. Therefore, some of the patients who
underwent CABG had taken aspirin before surgery
and others had used clopidogrel (600 mg daily)
in addition to aspirin. In this study, patients
were divided into two group based on the use
or non-use of clopidogrel. Inclusion criteria
were an age of between 40 and 80 years, serum
creatinine levels of less than 1.5 mg/dl, a
platelet count of more than 100,000 per microliter,
hemoglobin more than 8 g/dl, and normal PT and
PTT .
Exclusion criteria included a history of hereditary
bleeding disorders, use of anticoagulant drugs
in the previous month, having undergone CABG
surgery in the past, the use of clopidogrel
before the start of the current study, a history
of taking clopidogrel in the aspirin group,
a history of allergy to clopidogrel and aspirin,
a history of cerebrovascular disease, a history
of severe hepatic disease, cancer, severe bleeding
or cardiac tamponade after surgery which needed
surgical intervention, the need for anticoagulant
drugs after surgery, and gastrointestinal bleeding
after surgery.
Demographic variables, laboratory indicators,
signs and symptoms of the patients, the amount
of postoperative bleeding, and the amount of
blood transfused (during the first 24 hours),
duration of ICU and hospital stays, and duration
of drain use in patients were recorded in the
data collection form of the study. This form
was completed by executive colleagues of the
project. To describe the data, descriptive statistical
methods (mean, standard deviation, and frequency
percentages) and, to compare the examined variables,
analytical statistical methods, including the
independent t-test, chi-square, and analysis
of variance were used.
The
mean
age
of
the
patients
treated
with
aspirin
was
60.9±11.05,
and
the
mean
age
of
the
patients
treated
with
aspirin
and
clopidogrel
was
60.48±9.8.
According
to
t-test,
the
difference
in
age
between
the
two
groups
was
not
statistically
significant
(p=0.78).
In
the
aspirin
group,
42.9%
of
the
patients
and,
in
the
aspirin
plus
clopidogrel
group,
45.7%
of
the
patients
were
younger
than
60
years
old.
The
rest
of
the
patients
of
the
two
groups
were
older
than
60
years
old.
The
difference
in
age
distribution
between
the
two
groups
was
not
statistically
significant
according
to
a
chi-square
test
(P=0.73).
The
mean
BMI
in
the
group
treated
with
aspirin
was
27.3±4.2
and
in
the
group
treated
with
clopidogrel
+
aspirin,
was
28.3±10.
According
to
t-test,
the
difference
in
mean
BMI
was
not
statistically
significant
between
the
two
groups
(p=0.46).
In
the
aspirin
group,
the
mean
EF
of
the
patients
was
46.5±10.9
percent
and,
in
the
aspirin
plus
clopidogrel
group,
was
46.2±9.2
percent,
which
difference
was
not
found
to
be
statistically
significant
(p=0.86).
None
of
the
patients
in
both
groups
were
HIV
positive
or
HCV
positive.
Based
on
chi-square
test,
the
difference
in
the
need
for
blood
transfusion
in
the
studied
groups
during
the
first
24
hours
after
surgery
was
not
statistically
significant
(p=0.8).
(Table
1)
Table
1:
The
difference
in
the
need
for
blood
transfusion
in
the
studied
groups
during
the
first
24
hours
after
surgery
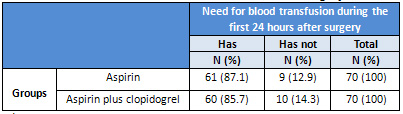
*
“N”
represents
the
number
of
patients
in
each
group
**
Statistical
test:
Chi-Square
test
Additionally,
according
to
the
above
table,
the
difference
in
the
need
for
blood
transfusions
during
hospital
stay
was
not
statistically
significant
between
the
group
receiving
aspirin
(91.4%)
and
the
group
receiving
aspirin
+
clopidogrel
(87.1%)(p=0.41)
(Table
2).
Table
2:
The
difference
in
the
need
for
blood
transfusion
in
the
studied
groups
during
hospital
stay
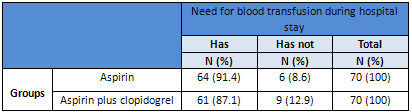
*
“N”
represents
the
number
of
patients
in
each
group
**
Statistical
test:
Chi-Square
test
According
to
the
results
of
a
repeated
measures,
test
differences
in
bleeding
in
each
group
over
time
was
statistically
significant
(time
effect).
But
the
difference
between
the
two
groups
was
not
statistically
significant
in
any
of
the
times
(24
hours
after
surgery
and
until
the
removal
of
the
drain)
(group
effect
and
the
time-group
interaction
were
not
statistically
significant
either)
(p=0.9).
According
to
an
independent
t-test,
the
difference
in
the
mean
bleeding
during
the
first
24
hours
after
surgery
was
not
statistically
significant
in
both
groups
receiving
aspirin
and
clopidogrel
+
aspirin
(p=0.067).
Although
the
amount
of
bleeding
in
the
group
receiving
aspirin
+
clopidogrel
was
more
than
the
aspirin
group,
this
difference
was
not
statistically
significant.
Despite
the
fact
that
the
group
receiving
aspirin
+
clopidogrel
had
more
bleeding
until
the
removal
of
the
drain
in
comparison
with
the
group
receiving
aspirin,
this
difference
was
not
statistically
significant
as
determined
by
a
t-test
(p=0.27).
The
mean
duration
of
ICU
stay
for
the
group
receiving
aspirin
was
53.12
hours
and
in
the
group
receiving
aspirin
+
clopidogrel,
it
was
50.35
hours.
This
difference
was
not
statistically
significant
(p=0.51).
The
mean
duration
of
drain
use
in
the
aspirin
group
was
106.2
hours
and
it
was
107.4
hours
in
the
group
receiving
aspirin
+
clopidogrel,
but
this
difference
was
not
statistically
significant
as
determined
by
a
t-test
(p>0.05).
In
the
group
receiving
aspirin,
3
patients
(4.3%)
and,
in
the
group
receiving
aspirin
+
clopidogrel,
6
patients
(8.6%)
needed
reoperation,
but
this
difference
was
not
statistically
significant,
according
to
Fisher’s
exact
test
(p=0.24).
(Table
3)
Table
3:
The
difference
in
the
need
for
need
for
reoperation
in
the
studied
groups
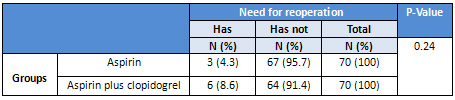
*
“N”
represents
the
number
of
patients
in
each
group
**
Statistical
test:
Fisher’s
exact
test
In
both
groups,
the
average
number
of
days
of
hospital
stay
was
6.5
days
and
the
t-test
showed
no
statistically
significant
difference
in
the
number
of
days
of
hospitalization
in
the
two
groups.
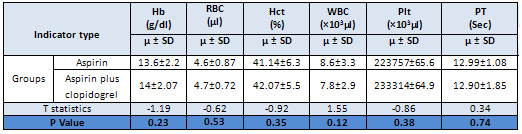
Based
on
the
obtained
results,
the
difference
in
the
mean
values
of
blood
parameters
before
the
surgery
was
not
statistically
significant
(p
>
0.05).
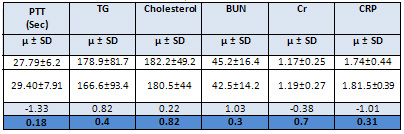
Additionally,
based
on
the
results
of
an
independent
t-test,
the
differences
in
values
of
lipid
profile,
renal
function
and
CRP
indexes
were
not
statistically
significant
in
the
two
groups
before
the
surgery
(p
>
0.05).
(Table
4)
Table
4:
The
Comparison
of
mean
and
standard
deviation
of
laboratory
indices
before
the
surgery
in
studied
groups
Table
5-
The
Comparison
of
mean
and
standard
deviation
of
laboratory
indices
in
studied
groups
at
discharge
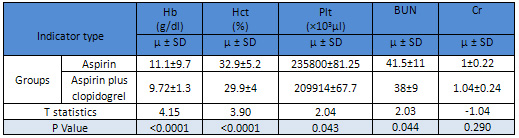
According
to
a
t-
test,
the
mean
values
of
Hb,
HCT,
PLT
and
BUN
was
significantly
higher
at
discharge
in
the
group
receiving
aspirin
than
in
the
group
receiving
aspirin
+
clopidogrel.
(Table
5).
Based
on
a
t-test,
there
was
no
significant
difference
between
the
mean
injected
platelet
units
for
the
studied
groups
during
hospital
stay
(p=0.47).
The
mean
FFP
received
during
hospital
stay
was
significantly
higher
in
the
group
receiving
aspirin
+
clopidogrel
than
in
the
group
receiving
aspirin
(p=0.0009).
Additionally,
the
mean
amounts
of
the
packed
cells
received
during
hospitalization
was
higher
in
the
group
receiving
aspirin
+
clopidogrel
than
in
the
aspirin
group.
But
this
difference
was
not
statistically
significant
(p=0.068).
75.7%
of
the
patients
receiving
aspirin
and
80%
of
the
patients
receiving
aspirin
+
clopidogrel
needed
to
receive
FFP
during
hospitalization.
According
to
a
chi-square
test,
this
difference
was
not
statistically
significant
(p=0.54).
None
of
the
patients
in
either
group
needed
receiving
whole
blood
during
hospitalization.
The
mean
postoperative
bleeding
at
various
times
after
surgery
and
Hb
and
HCT
amounts
did
not
show
any
significant
difference
in
the
aspirin-receiving
group
in
various
age
groups
(p
>
0.05).
The
need
for
blood
transfusions
in
younger
than
60
patients
in
the
aspirin
group
was
83.4%
and
in
the
older
than
60
patients
was
97.5%
and
according
to
Fisher’s
exact
test,
this
difference
was
statistically
significant
(p=0.036).
Moreover,
the
difference
in
the
amount
of
postoperative
bleeding,
hemoglobin
and
hematocrit
in
patients
receiving
aspirin
+
clopidogrel
was
not
statistically
significant
in
terms
of
age
groups
(under
60
and
60
years
and
older).
81.3%
of
the
patients
younger
than
60
years
and
92.1%
of
the
patients
60
years
and
older
who
received
aspirin
+
clopidogrel
needed
post-operative
blood
transfusions.
Fisher’s
exact
test
did
not
show
a
significant
difference
between
these
groups
(p=0.17).
Differences
in
the
frequency
distribution
of
the
number
of
grafts
in
both
groups
was
statistically
significant
(p=0.022),
but
the
mean
number
of
grafts
was
not
statistically
significant
(p=0.07).
Studies
published
in
1990
and
1991
indicated
that
the
administration
of
aspirin
preoperatively
leads
to
further
surgeries
due
to
increased
postoperative
bleeding
(6.6
vs.
1.7%
and
6.3
vs.
2.4%
in
two
studies)
(8,
9).
In
subsequent
studies,
however,
no
increase
in
bleeding
was
observed.
The
administration
of
aspirin
could
even
decrease
mortalities
in
hospitals
(10-12).
In
the
past,
concerns
about
bleeding
lead
physicians
to
advise
patients
undergoing
CABG
to
discontinue
taking
aspirin
three
to
five
days
before
surgery.
However,
this
general
view
is
not
recommended
any
more.
ACCF/AHA2011
instructions
recommend
continuing
to
take
aspirin
or
starting
it
before
CABG
surgery
(13).
Anemia
is
an
independent
risk
factor
predisposing
complications
and
mortality
after
CABG.
As
a
result,
the
transfer
of
red
blood
cells
(RBC)
is
common.
Blood
transfusion
rates
have
been
reported
to
be
between
40%
and
90%
(14).
In
the
present
study,
this
amount
was
91.4%
vs.
87.1%
which
was
lower
in
the
aspirin
+
clopidogrel
group,
but
the
difference
was
not
statistically
significant.
As
reported
in
2010,
among
more
than
82,000
patients
from
hospitals
in
the
United
States
who
had
undergone
CABG
surgery
with
cardiopulmonary
bypass
in
2008,
the
rate
of
blood
transfusions
during
surgery
was
56.1%
(15).
In
addition,
the
bleeding
which
requires
re-surgery
was
associated
with
a
strong
need
for
blood
transfusions,
and
longer
ICU
and
hospital
stays.
The
re-surgery
rates
ranged
from
4%
to
6%
(16).
However,
a
study
has
shown
that
during
1995-1997,
there
has
been
a
reduction
in
the
rates
of
re-operation
down
to
2%
(17).
In
the
present
study
too,
the
need
for
repeated
OR
in
the
aspirin
receiving
group
was
less
than
half
of
the
group
receiving
aspirin
+
clopidogrel.
However,
this
difference
was
not
statistically
significant
(3.4%vs.
6.8%).
Previous
randomized
trials
have
examined
dual
antiplatelet
therapy
with
aspirin
+
clopidogrel
in
cardiovascular
patients.
There
has
been
observed
no
clinical
benefits
in
two
studies
that
investigated
combined
antiplatelet
treatment
as
compared
with
aspirin
alone
for
patients
with
risk
factors
for
atherosclerosis,
cerebral,
cardiac
or
peripheral
vascular
disease
(18,
19).
On
the
contrary,
the
combination
of
clopidogrel
and
aspirin
as
compared
with
aspirin
alone
has
demonstrated
significant
improvements
in
the
outcome
of
patients
undergoing
percutaneous
vascular
intervention
(20),
and
in
patients
with
acute
coronary
syndrome
(21-23).
In
our
study
too,
no
benefits
were
observed
in
the
group
receiving
aspirin
+
clopidogrel.
Moreover,
the
aspirin
group
showed
significantly
lower
postoperative
bleeding
(834.67±595.81
vs.
662±506.39).
Also,
in
the
group
receiving
aspirin
the
mean
values
of
Hb,
HCT,
BUN,
and
blood
platelets
at
discharge
were
significantly
higher
than
the
group
receiving
aspirin
+
clopidogrel.
Additionally,
the
mean
amount
of
received
FFP
and
the
need
for
injections
were
lower
in
the
aspirin
group
patients
than
the
group
receiving
aspirin
+
clopidogrel
(97.5
vs.
83.13%,
p=0.0009).
If
the
above
criteria
be
considered
as
indicating
a
good
prognosis,
the
group
receiving
aspirin
had
a
better
prognosis.Often
surgeons
prescribe
clopidogrel
commonly
after
CABG,
believing
that
it
prevents
graft
occlusion,
and
possibly
improves
clinical
outcomes
(24,
25).
Although
prospective
randomized
controlled
trial
data
in
this
area
is
inadequate
(24),
previous
studies
cited
in
cardiac
surgery
literature
have
suggested
that
clopidogrel
may
improve
postoperative
outcomes
(25-27).
In
a
study
of
off-pump
CABG
patients,
Ebrahimi
et
al
demonstrated
that
adding
clopidogrel
to
aspirin
was
accompanied
with
a
tendency
toward
improvements
in
SVG
remaining
open
up
to
6
months
after
surgery
(26).
Recently,
Gao
et
al
have
reported
the
results
of
a
non-randomized
trial
in
which
197
patients
received
75
mg
clopidogrel
plus
100
mg
aspirin
the
day
after
surgery
based
on
a
weekly
replacement
therapy.
Within
7
days,
the
risk
of
life-threatening
events
or
major
bleeding
after
CABG
surgery
did
not
show
a
significant
increase
in
patients
receiving
clopidogrel
5
days
prior
to
CABG
(9.6%
vs
6.3%
with
placebo),
but
the
same
was
not
true
for
patients
who
had
discontinued
clopidogrel
five
days
or
more
before
CABG
(4.4%
vs.
5.3%)
(29).
These
findings
are
supported
by
several
other
observational
studies
(30-37).
In
our
study
too,
adding
aspirin
to
clopidogrel
did
not
lead
to
significant
differences
in
life-threatening
events,
which
confirms
the
cited
studies.
However,
in
a
study
by
Wang
et
al,
there
was
observed
a
good
response
to
adding
clopidogrel
to
aspirin
after
CABG
(38).
Given
the
obtained
results
in
the
present
study,
the
following
conclusions
can
be
drawn:
1.
The
amount
of
postoperative
bleeding
in
the
clopidogrel
+
aspirin
was
more
than
the
aspirin
group.
However,
its
P
Value
is
not
significant,
but
it
approaches
the
significance
level
(p=0.067).
2.
The
platelet,
Hb,
and
HCT
is
lower
at
discharge
in
the
clopidogrel
+
aspirin
group
than
in
the
aspirin
group,
the
cause
of
which
is
higher
blood
loss
in
the
aspirin
+
clopidogrel
group
in
comparison
with
the
aspirin
group.
3.
FFP
use
in
the
aspirin
+
clopidogrel
group
was
more
than
in
the
aspirin
group
which
is
due
to
increased
blood
loss
in
the
first
group
(p=0.000).
4.
To
get
more
accurate
results,
further
research
is
recommended
with
larger
sample
numbers.
5.
Considering
the
importance
of
the
drugs
aspirin
and
clopidogrel
in
the
prevention
of
heart
attacks
and
their
importance
in
the
health
system,
it
is
recommended
that
the
benefits
of
these
drugs
be
not
overlooked
in
comparison
with
their
possible
disadvantages.
1.
Karlsson
M,
Ternström
L,
Hyllner
M,
Baghaei
F,
Nilsson
S,
Jeppsson
A.
Plasma
fibrinogen
level,
bleeding,
and
transfusion
after
on-pump
coronary
artery
bypass
grafting
surgery:
a
prospective
observational
study.
Transfusion.
2008;
48
(10):2152-8.
2.
Angiolillo
DJ,
Guzman
LA,
Bass
TA.
Current
antiplatelet
therapies:
benefits
and
limitations.
Am
Heart
J.
2008;
156
(Suppl
2):
S3–9.
3.
Sun
JC,
Teoh
KH,
Lamy
A,
Sheth
T,
Ellins
ML,
Jung
H,
Yusuf
S,
Anand
S,
Connolly
S,
Whitlock
RP,
Eikelboom
JW.
Randomized
trial
of
aspirin
and
clopidogrel
versus
aspirin
alone
for
the
prevention
of
coronary
artery
bypass
graft
occlusion:
the
Preoperative
Aspirin
and
Postoperative
Anti-platelets
in
Coronary
Artery
Bypass
Grafting
study.
Am
Heart
J.
2010;
160
(6):
1178-84.
4.
Miceli
A,
Duggan
SM,
Aresu
G,
de
Siena
PM,
Romeo
F,
Glauber
M,
Caputo
M,
Angelini
GD.
Combined
clopidogrel
and
aspirin
treatment
up
to
surgery
increases
the
risk
of
postoperative
myocardial
infarction,
blood
loss
and
reoperation
for
bleeding
in
patients
undergoing
coronary
artery
bypass
grafting.
Eur
J
Cardiothorac
Surg.
2012
Jun
24.
[Epub
ahead
of
print]
5.
Zhou
YH,
Wei
X,
Lu
J,
Ye
XF,
Wu
MJ,
Xu
JF,
Qin
YY,
He
J.
Effects
of
combined
aspirin
and
clopidogrel
therapy
on
cardiovascular
outcomes:
a
systematic
review
and
meta-analysis.
PLoS
One.
2012;
7
(2):
e31642.
Epub
2012
Feb
13.
6.
Liu
PS,
Chen
X,
Shi
KH,
Xu
M,
Jiang
YS.
Impact
of
preoperative
clopidogrel
in
coronary
artery
bypass
grafting.
Zhonghua
Wai
Ke
Za
Zhi.
2008;
46
(4):
252-5.
7.
Cruden
NL,
Morch
K,
Wong
DR,
Klinke
WP,
Ofiesh
J,
Hilton
JD.
Clopidogrel
loading
dose
and
bleeding
outcomes
in
patients
undergoing
urgent
coronary
artery
bypass
grafting.
Am
Heart
J.
2011;
161
(2):
404-10.
8.
Goldman
S,
Copeland
J,
Moritz
T,
et
al.
Starting
aspirin
therapy
after
operation.
Effects
on
early
graft
patency.
Department
of
Veterans
Affairs
Cooperative
Study
Group.
Circulation
1991;
84:520.
9.
Sethi
GK,
Copeland
JG,
Goldman
S,
et
al.
Implications
of
preoperative
administration
of
aspirin
in
patients
undergoing
coronary
artery
bypass
grafting.
Department
of
Veterans
Affairs
Cooperative
Study
on
Antiplatelet
Therapy.
J
Am
Coll
Cardiol
1990;
15:
15.
10.
Bybee
KA,
Powell
BD,
Valeti
U,
et
al.
Preoperative
aspirin
therapy
is
associated
with
improved
postoperative
outcomes
in
patients
undergoing
coronary
artery
bypass
grafting.
Circulation
2005;
112:
I286.
11.
Dacey
LJ,
Munoz
JJ,
Johnson
ER,
et
al.
Effect
of
preoperative
aspirin
use
on
mortality
in
coronary
artery
bypass
grafting
patients.
Ann
Thorac
Surg
2000;
70:
1986.
12.
Mangano
DT,
Multicenter
Study
of
Perioperative
Ischemia
Research
Group.
Aspirin
and
mortality
from
coronary
bypass
surgery.
N
Engl
J
Med
2002;
347:
1309.
13.
Hillis
LD,
Smith
PK,
Anderson
JL,
et
al.
2011
ACCF/AHA
Guideline
for
Coronary
Artery
Bypass
Graft
Surgery:
executive
summary:
a
report
of
the
American
College
of
Cardiology
Foundation/American
Heart
Association
Task
Force
on
Practice
Guidelines.
Circulation
2011;
124:
2610.
14.
Hajjar
LA,
Vincent
JL,
Galas
FR,
et
al.
Transfusion
requirements
after
cardiac
surgery:
the
TRACS
randomized
controlled
trial.
JAMA
2010;
304:
1559.
15.
Bennett-Guerrero
E,
Zhao
Y,
O’Brien
SM,
et
al.
Variation
in
use
of
blood
transfusion
in
coronary
artery
bypass
graft
surgery.
JAMA
2010;
304:
1568.
16.
Sellman
M,
Intonti
MA,
Ivert
T.
Reoperations
for
bleeding
after
coronary
artery
bypass
procedures
during
25
years.
Eur
J
Cardiothorac
Surg
1997;
11:
521.
17.
Munoz
JJ,
Birkmeyer
NJ,
Dacey
LJ,
et
al.
Trends
in
rates
of
reexploration
for
hemorrhage
after
coronary
artery
bypass
surgery.
Northern
New
England
Cardiovascular
Disease
Study
Group.
Ann
Thorac
Surg
1999;
68:
1321.
18.
Diener
HC,
Bogousslavsky
J,
Brass
LM,
Cimminiello
C,
Csiba
L,
Kaste
M,
Leys
D,
Matias-Guiu
J,
Rupprecht
HJ.
Aspirin
and
clopidogrel
compared
with
clopidogrel
alone
after
recent
ischemic
stroke
or
transient
ischemic
attack
in
high-risk
patients
(MATCH):
randomized,
double-blind,
placebo-controlled
trial.
Lancet.
2004;
364:
331–337.
19.
Bhatt
DL,
Fox
KA,
Hacke
W,
Berger
PB,
Black
HR,
Boden
WE,
Cacoub
P,
Cohen
EA,
Creager
MA,
Easton
JD,
Flather
MD,
Haffner
SM,
Hamm
CW,
Hankey
GJ,
Johnston
SC,
Mak
KH,
Mas
JL,
Montalescot
G,
Pearson
TA,
Steg
PG,
Steinhubl
SR,
Weber
MA,
Brennan
DM,
Fabry-Ribaudo
L,
Booth
J,
Topol
EJ.
Clopidogrel
and
aspirin
versus
aspirin
alone
for
the
prevention
of
atherothrombotic
events.
N
Engl
J
Med.
2006;
354:
1706–1717.
20.
Steinhubl
SR,
Berger
PB,
Mann
JT
III,
Fry
ET,
DeLago
A,
Wilmer
C,
Topol
EJ.
Early
and
sustained
dual
oral
antiplatelet
therapy
following
percutaneous
coronary
intervention:
a
randomized
controlled
trial.
JAMA.
2002;
288:
2411–2420.
21.
Yusuf
S,
Zhao
F,
Mehta
SR,
Chrolavicius
S,
Tognoni
G,
Fox
KK.
Effects
of
clopidogrel
in
addition
to
aspirin
in
patients
with
acute
coronary
syndromes
without
ST-segment
elevation.
N
Engl
J
Med.
2001;
345:
494–502.
22.
Chen
ZM,
Jiang
LX,
Chen
YP,
Xie
JX,
Pan
HC,
Peto
R,
Collins
R,
Liu
LS.
Addition
of
clopidogrel
to
aspirin
in
45,852
patients
with
acute
myocardial
infarction:
randomized
placebo-controlled
trial.
Lancet.
2005;
366:
1607–1621.
23.
Sabatine
MS,
Cannon
CP,
Gibson
CM,
Lopez-Sendon
JL,
Montalescot
G,
Theroux
P,
Claeys
MJ,
Cools
F,
Hill
KA,
Skene
AM,
McCabe
CH,
Braunwald
E.
Addition
of
clopidogrel
to
aspirin
and
fibrinolytic
therapy
for
myocardial
infarction
with
ST-segment
elevation.
N
Engl
J
Med.2005;
352:
1179–118
24.
Kulik
A,
Chan
V,
Ruel
M.
Antiplatelet
therapy
and
coronary
artery
bypass
graft
surgery:
perioperative
safety
and
efficacy.
Expert
Opin
Drug
Saf.
2009;
8:
169–182.
25.
Kim
DH,
Daskalakis
C,
Silvestry
SC,
Sheth
MP,
Lee
AN,
Adams
S,
Hohmann
S,
Medvedev
S,
Whellan
DJ.
Aspirin
and
clopidogrel
use
in
the
early
postoperative
period
following
on-pump
and
off-pump
coronary
artery
bypass
grafting.
J
Thorac
Cardiovasc
Surg.
2009;
138:
1377–1384.
26.
Ibrahim
K,
Tjomsland
O,
Halvorsen
D,
Wiseth
R,
Wahba
A,
Karevold
A,
Haaverstad
R.
Effect
of
clopidogrel
on
midterm
graft
patency
following
off-pump
coronary
revascularization
surgery.
Heart
Surg
Forum.
2006;
9:
E581–E856.
27.
Gurbuz
AT,
Zia
AA,
Vuran
AC,
Cui
H,
Aytac
A.
Postoperative
clopidogrel
improves
mid-term
outcome
after
off-pump
coronary
artery
bypass
graft
surgery:
a
prospective
study.
Eur
J
Cardiothorac
Surg.
2006;
29:
190–195.
28.
Gao
C,
Ren
C,
Li
D,
Li
L.
Clopidogrel
and
aspirin
versus
clopidogrel
alone
on
graft
patency
after
coronary
artery
bypass
grafting.
Ann
Thorac
Surg.
2009;
88:59–62.
29.
Fox
KA,
Mehta
SR,
Peters
R,
et
al.
Benefits
and
risks
of
the
combination
of
clopidogrel
and
aspirin
in
patients
undergoing
surgical
revascularization
for
non-ST-elevation
acute
coronary
syndrome:
the
Clopidogrel
in
unstable
angina
to
prevent
recurrent
ischemic
Events
(CURE)
Trial.
Circulation
2004;
110:1202.
30.
Chu
MW,
Wilson
SR,
Novick
RJ,
et
al.
Does
clopidogrel
increase
blood
loss
following
coronary
artery
bypass
surgery?
Ann
Thorac
Surg
2004;
78:1536.
31.
Mehta
RH,
Roe
MT,
Mulgund
J,
et
al.
Acute
clopidogrel
use
and
outcomes
in
patients
with
non-ST-segment
elevation
acute
coronary
syndromes
undergoing
coronary
artery
bypass
surgery.
J
Am
Coll
Cardiol
2006;
48:281.
32.
Berger
JS,
Frye
CB,
Harshaw
Q,
et
al.
Impact
of
clopidogrel
in
patients
with
acute
coronary
syndromes
requiring
coronary
artery
bypass
surgery:
a
multicenter
analysis.
J
Am
Coll
Cardiol
2008;
52:
1693.
33.
Kim
JH,
Newby
LK,
Clare
RM,
et
al.
Clopidogrel
use
and
bleeding
after
coronary
artery
bypass
graft
surgery.
Am
Heart
J
2008;
156:
886.
34.
Bavry
AA,
Lincoff
AM.
Is
clopidogrel
cardiovascular
medicine’s
double-edged
sword?
Circulation
2006;
113:
1638.
35.
Ebrahimi
R,
Dyke
C,
Mehran
R,
et
al.
Outcomes
following
pre-operative
clopidogrel
administration
in
patients
with
acute
coronary
syndromes
undergoing
coronary
artery
bypass
surgery:
the
ACUITY
(Acute
Catheterization
and
Urgent
Intervention
Triage
strategY)
trial.
J
Am
Coll
Cardiol
2009;
53:
1965.
36.
Nijjer
SS,
Watson
G,
Athanasiou
T,
Malik
IS.
Safety
of
clopidogrel
being
continued
until
the
time
of
coronary
artery
bypass
grafting
in
patients
with
acute
coronary
syndrome:
a
meta-analysis
of
34
studies.
Eur
Heart
J
2011;
32:
2970.
37.
Vito
Antonio
Mannacio1,
Luigi
Di
Tommaso,
Anita
Antignan,
Vincenzo
De
Amicis,
Carlo
Vosa.
Aspirin
plus
clopidogrel
for
optimal
platelet
inhibition
following
off-pump
coronary
artery
bypass
surgery:
results
from
the
CRYSSA
(prevention
of
Coronary
artery
bypass
occlusion
after
off-pump
procedures)
randomized
study.
Coronary
revascularization.
2012;
(online)
38.
Wang
X,
Gong
X,
Zhu
T,
Zhang
Q,
Zhang
Y,
Wang,
et
al.
Clopidogrel
improves
aspirin
response
after
off-pump
coronary
artery
bypass
surgery.
J
Biomed
Res.
2014;
28
(2):
108-13.
|
|
.................................................................................................................

|
| |
|

