|
|
 |
| ............................................................. |
|
October 2017 -
Volume 15, Issue 8
|
 |
|
View
this issue in pdf formnat - the issue
has been split into two files for downloading
due to its large size: FULLpdf
(12 MB)
Part
1 &
Part
2
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
........................................................
|
|
Original Contribution/Clinical Investigation
Immunity
level to diphtheria in beta thalassemia patients
DOI: 10.5742/MEWFM.2017.93048
[pdf
version]
Abdolreza Sotoodeh Jahromi, Karamatollah Rahmanian,
Abdolali Sapidkar, Hassan Zabetian, Alireza
Yusefi, Farshid Kafilzadeh, Mohammad Kargar,
Marzieh Jamalidoust,
Abdolhossein Madani
Genetic
Variants of Toll Like Receptor-4 in Patients
with Premature Coronary Artery Disease, South
of Iran
DOI: 10.5742/MEWFM.2017.93049
[pdf
version]
Saeideh Erfanian, Mohammad Shojaei, Fatemeh
Mehdizadeh, Abdolreza Sotoodeh Jahromi, Abdolhossein
Madani, Mohammad Hojjat-Farsangi
Comparison
of postoperative bleeding in patients undergoing
coronary artery bypass surgery in two groups
taking aspirin and aspirin plus CLS clopidogrel
DOI: 10.5742/MEWFM.2017.93050
[pdf
version]
Ali Pooria, Hassan Teimouri, Mostafa Cheraghi,
Babak Baharvand Ahmadi, Mehrdad Namdari, Reza
Alipoor
Comparison
of lower uterine segment thickness among nulliparous
pregnant women without uterine scar and pregnant
women with previous cesarean section: ultrasound
study
DOI: 10.5742/MEWFM.2017.93051
[pdf version]
Taravat Fakheri, Irandokht Alimohammadi, Nazanin
Farshchian, Maryam Hematti,
Anisodowleh Nankali, Farahnaz Keshavarzi, Soheil
Saeidiborojeni
Effect
of Environmental and Behavioral Interventions
on Physiological and Behavioral Responses of
Premature Neonates Candidates Admitted for Intravenous
Catheter Insertion in Neonatal Intensive Care
Units
DOI: 10.5742/MEWFM.2017.93052
[pdf
version]
Shohreh Taheri, Maryam Marofi, Anahita Masoumpoor,
Malihe Nasiri
Effect
of 8 weeks Rhythmic aerobic exercise on serum
Resistin and body mass index of overweight and
obese women
DOI: 10.5742/MEWFM.2017.93053
[pdf
version]
Khadijeh Molaei, Ahmad Shahdadi, Reza Delavar
Study
of changes in leptin and body mass composition
with overweight and obesity following 8 weeks
of Aerobic exercise
DOI: 10.5742/MEWFM.2017.93054
[pdf
version]
Khadijeh Molaei, Abbas Salehikia
A reassessment
of factor structure of the Short Form Health
Survey (SF-36): A comparative approach
DOI: 10.5742/MEWFM.2017.93088
[pdf version]
Vida Alizad, Manouchehr Azkhosh, Ali Asgari,
Karyn Gonano
Population and Community Studies
Evaluation
of seizures in pregnant women in Kerman - Iran
DOI: 10.5742/MEWFM.2017.93056
[pdf
version]
Hossein Ali Ebrahimi, Elahe Arabpour, Kaveh
Shafeie, Narges Khanjani
Studying
the relation of quality work life with socio-economic
status and general health among the employees
of Tehran University of Medical Sciences (TUMS)
in 2015
DOI: 10.5742/MEWFM.2017.93057
[pdf version]
Hossein Dargahi, Samereh Yaghobian, Seyedeh
Hoda Mousavi, Majid Shekari Darbandi, Soheil
Mokhtari, Mohsen Mohammadi, Seyede Fateme Hosseini
Factors
that encourage early marriage and motherhood
from the perspective of Iranian adolescent mothers:
a qualitative study
DOI: 10.5742/MEWFM.2017.93058
[pdf
version]
Maasoumeh Mangeli, Masoud Rayyani, Mohammad
Ali Cheraghi, Batool Tirgari
The
Effectiveness of Cognitive-Existential Group
Therapy on Reducing Existential Anxiety in the
Elderly
DOI: 10.5742/MEWFM.2017.93059
[pdf
version]
Somayeh Barekati, Bahman Bahmani, Maede Naghiyaaee,
Mahgam Afrasiabi, Roya Marsa
Post-mortem
Distribution of Morphine in Cadavers Body Fluids
DOI: 10.5742/MEWFM.2017.93060
[pdf
version]
Ramin Elmi, Mitra Akbari, Jaber Gharehdaghi,
Ardeshir Sheikhazadi, Saeed Padidar, Shirin
Elmi
Application
of Social Networks to Support Students' Language
Learning Skills in Blended Approach
DOI: 10.5742/MEWFM.2017.93061
[pdf
version]
Fatemeh Jafarkhani, Zahra Jamebozorg, Maryam
Brahman
The
Relationship between Chronic Pain and Obesity:
The Mediating Role of Anxiety
DOI: 10.5742/MEWFM.2017.93062
[pdf
version]
Leila Shateri, Hamid Shamsipour, Zahra Hoshyari,
Elnaz Mousavi, Leila Saleck, Faezeh Ojagh
Implementation
status of moral codes among nurses
DOI: 10.5742/MEWFM.2017.93063
[pdf
version]
Maryam Ban, Hojat Zareh Houshyari Khah, Marzieh
Ghassemi, Sajedeh Mousaviasl, Mohammad Khavasi,
Narjes Asadi, Mohammad Amin Harizavi, Saeedeh
Elhami
The comparison
of quality of life, self-efficacy and resiliency
in infertile and fertile women
DOI: 10.5742/MEWFM.2017.93064
[pdf version]
Mahya Shamsi Sani, Mohammadreza Tamannaeifar
Brain MRI Findings in Children (2-4 years old)
with Autism
DOI: 10.5742/MEWFM.2017.93055
[pdf
version]
Mohammad Hasan Mohammadi, Farah Ashraf Zadeh,
Javad Akhondian, Maryam Hojjati,
Mehdi Momennezhad
Reviews
TECTA gene function and hearing: a review
DOI: 10.5742/MEWFM.2017.93065
[pdf version]
Morteza Hashemzadeh-Chaleshtori, Fahimeh Moradi,
Raziyeh Karami-Eshkaftaki,
Samira Asgharzade
Mandibular
canal & its incisive branch: A CBCT study
DOI: 10.5742/MEWFM.2017.93066
[pdf
version]
Sina Haghanifar, Ehsan Moudi, Ali Bijani, Somayyehsadat
Lavasani, Ahmadreza Lameh
The
role of Astronomy education in daily life
DOI: 10.5742/MEWFM.2017.93067
[pdf
version]
Ashrafoalsadat Shekarbaghani
Human brain
functional connectivity in resting-state fMRI
data across the range of weeks
DOI: 10.5742/MEWFM.2017.93068
[pdf version]
Nasrin Borumandnia, Hamid Alavi Majd, Farid
Zayeri, Ahmad Reza Baghestani,
Mohammad Tabatabaee, Fariborz Faegh
International Health Affairs
A
brief review of the components of national strategies
for suicide prevention suggested by the World
Health Organization
DOI: 10.5742/MEWFM.2017.93069
[pdf
version]
Mohsen Rezaeian
Education and Training
Evaluating
the Process of Recruiting Faculty Members in
Universities and Higher Education and Research
Institutes Affiliated to Ministry of Health
and Medical Education in Iran
DOI: 10.5742/MEWFM.2017.93070
[pdf
version]
Abdolreza Gilavand
Comparison
of spiritual well-being and social health among
the students attending group and individual
religious rites
DOI: 10.5742/MEWFM.2017.93071
[pdf
version]
Masoud Nikfarjam, Saeid Heidari-Soureshjani,
Abolfazl Khoshdel, Parisa Asmand, Forouzan Ganji
A
Comparative Study of Motivation for Major Choices
between Nursing and Midwifery Students at Bushehr
University of Medical Sciences
DOI: 10.5742/MEWFM.2017.93072
[pdf
version]
Farzaneh Norouzi, Shahnaz Pouladi, Razieh Bagherzadeh
Clinical Research and Methods
Barriers
to the management of ventilator-associated pneumonia:
A qualitative study of critical care nurses'
experiences
DOI: 10.5742/MEWFM.2017.93073
[pdf version]
Fereshteh Rashnou, Tahereh Toulabi, Shirin Hasanvand,
Mohammad Javad Tarrahi
Clinical
Risk Index for Neonates II score for the prediction
of mortality risk in premature neonates with
very low birth weight
DOI: 10.5742/MEWFM.2017.93074
[pdf
version]
Azadeh Jafrasteh, Parastoo Baharvand, Fatemeh
Karami
Effect
of pre-colporrhaphic physiotherapy on the outcomes
of women with pelvic organ prolapse
DOI: 10.5742/MEWFM.2017.93075
[pdf
version]
Mahnaz Yavangi, Tahereh Mahmoodvand, Saeid Heidari-Soureshjani
The
effect of Hypertonic Dextrose injection on the
control of pains associated with knee osteoarthritis
DOI: 10.5742/MEWFM.2017.93076
[pdf
version]
Mahshid Ghasemi, Faranak Behnaz, Mohammadreza
Minator Sajjadi, Reza Zandi,
Masoud Hashemi
Evaluation
of Psycho-Social Factors Influential on Emotional
Divorce among Attendants to Social Emergency
Services
DOI: 10.5742/MEWFM.2017.93077
[pdf
version]
Farangis Soltanian
Models and Systems of Health Care
Organizational
Justice and Trust Perceptions: A Comparison
of Nurses in public and private hospitals
DOI: 10.5742/MEWFM.2017.93078
[pdf
version]
Mahboobeh Rajabi, Zahra Esmaeli Abdar, Leila
Agoush
Case series and Case reports
Evaluation
of Blood Levels of Leptin Hormone Before and
After the Treatment with Metformin
DOI: 10.5742/MEWFM.2017.93079
[pdf
version]
Elham Jafarpour
Etiology,
Epidemiologic Characteristics and Clinical Pattern
of Children with Febrile Convulsion Admitted
to Hospitals of Germi and Parsabad towns in
2016
DOI: 10.5742/MEWFM.2017.93080
[pdf
version]
Mehri SeyedJavadi, Roghayeh Naseri, Shohreh
Moshfeghi, Irandokht Allahyari, Vahid Izadi,
Raheleh Mohammadi,
Faculty development
The
comparison of the effect of two different teaching
methods of role-playing and video feedback on
learning Cardiopulmonary Resuscitation (CPR)
DOI: 10.5742/MEWFM.2017.93081
[pdf
version]
Yasamin Hacham Bachari, Leila Fahkarzadeh, Abdol
Ali Shariati
Office based family medicine
Effectiveness
of Group Counseling With Acceptance and Commitment
Therapy Approach on Couples' Marital Adjustment
DOI: 10.5742/MEWFM.2017.93082
[pdf
version]
Arash Ziapour, Fatmeh Mahmoodi, Fatemeh Dehghan,
Seyed Mehdi Hoseini Mehdi Abadi,
Edris Azami, Mohsen Rezaei
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| October 2017 -
Volume 15, Issue 8 |
|
|
Comparison of lower uterine
segment thickness among nulliparous pregnant
women without uterine scar and pregnant women
with previous cesarean section: ultrasound study
Taravat Fakheri (1)
Irandokht Alimohammadi (2)
Nazanin Farshchian (3)
Maryam Hematti (4)
Anisodowleh Nankali (1)
Farahnaz Keshavarzi (1)
Soheil Saeidiborojeni (5)
(1) Department of Obstetrics and Gynecology,
College of Medicine, Kermanshah University of
Medical Sciences, Kermanshah, Iran
(2)Research Committee of Students, Kermanshah
University of Medical Sciences, Kermanshah,
Iran
(3) Department of Radiology, College of Medicine,
Kermanshah University of Medical Sciences, Kermanshah,
Iran
(4) Kermanshah University of Medical Sciences,
Kermanshah, Iran
(5) Science undergraduate student. Simon Faster
University, Canada.
Correspondence:
Anisodowleh Nankali ,
Department of Obstetrics and Gynecology, Kermanshah
University of Medical Sciences, Kermanshah,
Iran
Email: anis_nankali@yahoo.com
|
Abstract
Objective: To
compare the Lower Uterine Segment (LUS)
thickness among nulliparous pregnant women
without uterine scar and pregnant women
with previous cesarean section (CS) using
trans-abdominal ultrasound in the third
trimester.
Methods:
Three groups were included as 20 nulliparous
women (group 1), 31 pregnant women with
a single previous CS, and 27 pregnant
women with two or more previous CS at
gestational weeks 36 to 40. LUS thickness
was measured by transabdominal ultrasound.
The measured thickness was compared between
the three studied groups and the cut-off
value was determined by Receiver Operating
Characteristic (ROC) curve. Uterine dehiscence
during delivery was also compared between
the three groups.
Results:
Mean (±SD) LUS thickness in groups
1, 2, and 3 was respectively 6.05 (±2.5),
5.33 (±1.33), and 4.49 (±1.54)
mm (P= 0.01). Three patients (9.7%) in
group 2 has dehiscence during CS. Mean
(±SD) LUS thickness in these three
patients was 4.40 (±0.36) mm. In
group 3, two patients (7.4%) experienced
dehiscence during CS with a mean (±SD)
LUS thickness of 1.2 (±0.6) mm.
Cut-off value to predict uterine dehiscence
and rupture was 1.7 mm with a sensitivity
of 78% and specificity of 76%
Conclusions:
LUS thickness was significantly lower
in pregnant mothers with previous CS and
this led to dehiscence in such patients.
In case of LUS thickness of < 1.7 mm,
the risk of dehiscence and rupture increases.
Key words:
Ultrasonography; Cesarean section; lower
uterine segment; scar
|
Cesarean section (CS) has faced a growing trend
worldwide. During a 25-year period (1990 to
2014), the average CS rate has grown from 6.7%
to 19.1% translated to an average rise of 12.4%
(1).
One of its consequences may be cesarean scar
defect (CSD) (2). This may cause dysmenorrhea
and post menstrual bleeding in non-pregnant
uterus and uterine rupture or dehiscence during
labor or cesarean operation (3). Dehiscence
represents separation of low uterine segment
with intact serosa in contrast to uterine rupture(4).
Many investigations are conducted for early
diagnosis of uterine rupture during trial of
labor (TOL) by LUS thickness measurement(4-5)
either by Trans abdominal or Trans vaginal Ultrasonography(5,6).
Lower uterine segment (LUS) thickness is one
of the factors suggested to have prognostic
value for uterine rupture during delivery in
women with previous CS surgery (7). Uterine
rupture, though rare, is a grave complication
with significant morbidity and mortality (7).
Hence, ultrasound examination of the LUS thickness
in the third trimester has gained attention
to predict possible uterine rupture and to implement
appropriate obstetrical decisions.
Thinning of the LUS has been significantly
associated with uterine scar defect at week
37 in a way that a threshold of 2.5 mm for LUS
thickness was proposed as a risk factor (8).
LUS is thinner in the third trimester compared
to the second trimester. Ultrasound examination
of LUS is a simple and non-invasive method which
can provide useful information about the thickness
of the LUS as well as prognostic value for uterine
rupture. Integrating LUS measurement by ultrasound
has been shown to result in lower risk of uterine
rupture (9).
Although most studies have proposed cut-off
values of about 2.5 to 3.5 mm for LUS thickness,
there is controversy in the literature about
the exact thickness that can be used for prognostic
objectives (10).
Most previous studies have included patients
with previous CS and investigated the risk of
thin LUS with VBAC and uterine rupture (11,
9, 12). It should be noted that some limited
studies included patients with and without history
of CS (13-15). However, we think that more studies
are required to precisely answer the question
as to if there is a real difference regarding
LUS thickness between pregnant women with and
without history of CS. Therefore, we conducted
the current study to compare the LUS thickness
among nulliparous pregnant women without uterine
scar and pregnant women with previous cesarean
section using trans-abdominal ultrasound in
the third trimester.
From December 2014 to Dec 2016 this cross sectional
descriptive-analytic study took place in Imam
Reza hospital, Kermanshah Iran. The study sample
consisted of 78 pregnant women divided into
three groups: 20 nulliparous women without previous
CS (group 1), 27 pregnant women with a single
previous CS (group 2) and 31pregnant women with
two or more previous CSs (group 3). They were
recruited consecutively in their 36th to 40th
week of gestation when they presented for delivery
or ultrasound examination to our university
obstetric department.
The sample size was calculated using previous
data about mean (SD) LUS thickness of 4.7 (1.2)
mm and 6.6 (2) mm in patients with and without
previous CS (9). Considering =0.05, power= 90%,
the estimated sample size was calculated as
at least 20 subjects in each group (a total
of 60 cases).
Inclusion criteria were singleton pregnancy,
gestational age of 36 to 40 weeks, according
to LMP cephalic presentation, and normal volume
of amniotic fluid.
Exclusion criteria were multiple pregnancy,
active labor, abnormal amniotic fluid volume,
previous uterine rupture, placenta previa, fetal
congenital malformations, and uterine surgical
interventions other than CS.
Gestational age was estimated using the LMP
and the first-trimester ultrasound report. LUS
thickness was measured by trans-abdominal ultrasound
(VINNO, G80) with a 3.5 MHz convex probe. The
examinations were done with the bladder half-full
(bladder extension at sagittal plane was 6 to
7 cm) and in the absence of uterine contractions.
The LUS thickness was measured as the distance
between myometrium-urinary bladder wall interface
and myometrium-chorioamniotic membrane interface.
The thickness was measured successively for
three times by a board-certified radiologist
and the mean value was documented as the final
mean LUS thickness. The measurements were made
in a perpendicular plane to the uterine body.
The gathered data (maternal age, gestational
age, parity, and LUS thickness) were entered
into a checklist. In addition, the patients
were followed and the following variables were
recorded at the time of delivery: Apgar scores
at minutes 1 and 5, birth weight, and dehiscence
at delivery.
Statistical analyses
The data were gathered and entered into the
SPSS software for Windows (ver. 21.0). Descriptive
indices such as frequency, percentage, mean
and its standard deviation (±SD) were
used to express data. The Kolmogorov-Smirnov
test was used to determine normal distribution
of continuous variables. One-way ANOVA (analysis
of variance) was used to compare continuous
data with normal distribution (maternal age,
BMI, birth weight, and LUS thickness) and the
Kruskal-Wallis for non-normally distributed
variables (gestational age). In order to compare
LUS thickness of patients in groups 2 and 3
who experienced dehiscence during CS, the Student’s
t test was applied. Significance level was set
at 0.05.
Ethics
The study protocol was approved by the Ethics
Committee of our medical university. The study
objectives were explained for the patients prior
to participation and if agreed, written informed
consent was obtained from them.
A
total
of
78
subjects
were
included.
There
were
20
nulliparous
women
(25.6%)
with
a
mean
(SD)
age
of
26.16
(1.33)
years,
31
with
one
previous
CS
(39.7%)
with
a
mean
(SD)
age
of
31.46
(0.96)
years,
and
27
subjects
(34.6%)
who
had
undergone
CS
at
least
twice
and
had
a
mean
(SD)
age
of
32.5
(0.99)
years.
A
significant
difference
existed
among
the
groups
regarding
age
(P<
0.001).
Mean
gestational
age
in
groups
1,
2,
and
3
was
respectively
38,
37.26,
and
37
weeks
(P=
0.12).
There
was
no
significant
difference
regarding
mean
(±SD)
birth
weight
among
the
three
groups
(3,400
(±327.26)
gr
in
group
1,
3,253.35
(±379.81)
in
group
2,
and
3,247.35
(±388.25)
in
group
3);
P=
0.3.
Mean
BMI
values
in
groups
1,
2,
and
3
were
respectively
29.93,
29.89,
and
29.25
kg/m2
(P=
0.79).
Mean
(±SD)
LUS
thickness
in
groups
1,
2,
and
3
was
respectively
6.05
(±2.5),
5.33
(±1.33),
and
4.49
(±1.54)
mm
(P=
0.01).
Range
of
LUS
thickness
in
groups
1,
2,
and
3
was
1
to
11
mm,
3
to
8.5
mm,
and
0.8
to
7.3
mm.
Three
patients
(9.7%)
in
group
2
has
dehiscence
during
CS.
Mean
(±SD)
LUS
thickness
in
these
three
patients
was
4.40
(±0.36)
mm.
In
group
3,
two
patients
(7.4%)
experienced
dehiscence
during
CS
with
a
mean
(±SD)
LUS
thickness
of
1.2
(±0.6)
mm.
There
was
a
significant
difference
regarding
mean
LUS
thickness
between
groups
2
and
3
who
experienced
dehiscence
(P=
0.03).
Paper-thin
LUS
was
documented
in
4
patients
(12.9%)
of
group
2
with
mean
(±SD)
LUS
thickness
of
4
(±0.81)
mm.
This
finding
was
seen
in
more
patients
of
group
3
(11
cases,
40.7%)
with
a
mean
(±SD)
LUS
thickness
of
3.44
(±0.75)
mm.
Uterine
rupture
occurred
in
only
one
patient
who
was
in
group
3
whose
LUS
thickness
was
2.5
mm.
This
was
not
observed
by
ultrasound
and
rupture
was
diagnosed
during
CS.
Ultrasound
showed
dehiscence
in
only
one
patient
in
the
second
group
whose
LUS
thickness
was
3
mm.
However,
three
more
patients
in
group
2
were
diagnosed
with
rupture
during
CS
with
LUS
thickness
values
of
4,
4.5,
and
4.7
mm.
In
group
3,
two
patients
were
diagnosed
to
have
rupture
by
ultrasound.
LUS
thicknesses
of
these
two
patients
were
0.8
and
2.5
mm.
These
were
confirmed
during
CS.
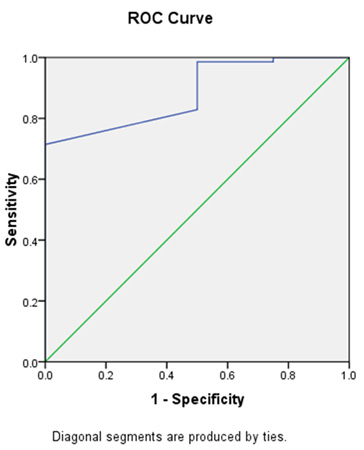
Cut-off
value
to
predict
uterine
dehiscence
and
rupture
was
1.7
mm
with
a
sensitivity
of
78%
and
specificity
of
76%
(Figure
1).
Click
here
for
Table
1:
Apgar
scores
at
minutes
1
and
5
in
the
three
studied
groups
Figure
1:
Receiver
operating
curve
for
lower
uterine
segment
thickness
of
1.7
mm
with
sensitivity
of
78%
and
specificity
of
76%
for
predicting
uterine
dehiscence
and
rupture
Based
on
the
obtained
findings,
those
who
had
previous
CS
had
significantly
thinner
LUS.
This
resulted
in
dehiscence
and
rupture
in
these
patients.
On
the
other
hand,
none
of
the
nulliparous
women
with
thicker
LUS
experienced
dehiscence
or
rupture.
The
neonates’
birth
weight
did
not
show
difference
among
groups,
so
it
is
highly
likely
that
dehiscence
and
rupture
occurred
due
to
thinner
LUS.
The
obtained
results
are
in
agreement
with
some
previous
reports.
In
a
study
involving
106
patients
with
previous
CS
and
68
without,
LUS
was
thinner
in
the
first
group
with
a
mean
value
of
4.58
mm
than
in
the
second
group
(4.8
mm)
(16).
Ultrasound
can
detect
dehiscence
by
showing
a
defective
area
where
no
myometrial
layer
is
seen
(17).
In
this
study,
in
patients
with
more
than
one
previous
CS,
US
findings
were
in
agreement
with
findings
during
CS.
The
cut-off
value
we
obtained
here
(1.7
mm)
is
very
close
to
the
reported
value
by
a
previous
study
(1.8
mm)
(18).
However,
some
studies
have
proposed
higher
values
at
2.5
to
3.5
mm
among
patients
with
previous
CS
(11).
Although
we
observed
dehiscence
and
rupture
in
patients
with
LUS
thickness
of
more
than
3
mm,
one
patient
who
experienced
rupture
had
a
LUS
thickness
of
2.5
mm.
A
previous
study
showed
that
none
of
the
patients
with
LUS
thickness
of
<3
mm
experienced
dehiscence
or
rupture
(9).
In
a
former
meta-analysis
of
about
2,700
patients,
sensitivity
and
specificity
for
cut-off
values
for
LUS
thickness
to
predict
uterine
defects
was
76%
and
92%
for
values
between
0.6
and
2
mm
(19).
Ultrasound
is
a
non-invasive
method
to
measure
LUS
thickness
and
its
ability
to
predict
dehiscence
and
rupture
has
been
investigated
previously
(9,
10).
One
of
the
limitations
in
this
study
was
that
we
were
not
able
to
gather
all
details
about
previous
CS.
Although
CS
per
se
is
considered
a
risk
factor
for
scar
formation
and
thinner
LUS,
other
factors
can
also
have
a
role
in
LUS
thickness.
In
a
previous
study,
maternal
age
of
more
than
35
years,
single
layer
uterine
closure,
and
non-elective
CS
were
factors
to
be
associated
with
LUS
thickness
(12).
All
these
factors
can
affect
healing
of
the
LUS
after
CS
and
influence
the
integrity
of
LUS.
Limitations
We
intended
to
determine
the
effect
of
multiple
previous
CS
on
LUS
thickness,
and
it
was
found
that
LUS
was
thinner
in
those
with
multiple
CSs,
however
as
the
rate
of
dehiscence
and
rupture
was
a
secondary
objective;
the
sample
size
was
not
large
enough
to
achieve
a
conclusion
in
this
regard.
Future
studies
with
larger
sample
size
can
answer
the
question
of
the
effect
of
multiple
CSs.
Another
limitation
is
that
we
were
not
able
to
perform
transvaginal
ultrasound
as
some
studies
have
demonstrated
that
transvaginal
ultrasound
provides
better
information
about
myometrial
thickness
than
transabdominal
ultrasound
(20).
However,
this
may
not
be
regarded
as
a
significant
limitation
as
there
is
evidence
of
more
than
90%
correlation
between
trans-abdominal
and
transvaginal
ultrasonography
and
a
cut-off
value
of
2.5
mm
(21).
LUS
thickness
was
significantly
lower
in
pregnant
mothers
with
previous
CS
and
this
led
to
dehiscence
in
such
patients.
In
case
of
LUS
thickness
of
<
1.7
mm,
the
risk
of
dehiscence
and
rupture
increases.
Acknowledgment
This
paper
was
taken
from
the
thesis
of
Irandokht
Alimohammadi
as
a
requirement
to
receive
PhD
in
Obstetrics
and
Gynecology
from
Kermanshah
University
of
Medical
Sciences
1.
Betrán
AP,
Ye
J,
Moller
AB,
Zhang
J,
Gülmezoglu
AM,
et
al.
(2016).
The
Increasing
Trend
in
Caesarean
Section
Rates:
Global,
Regional
and
National
Estimates:
1990-2014.
PLOS
ONE
11(2):
e0148343.
https://doi.org/10.1371/journal.pone.0148343.
2.
Wang
CB,
Chiu
WW,
Lee
CY,
Sun
YL,
Lin
YH,
Tseng
CJ.
Cesarean
scar
defect:
correlation
between
Cesarean
section
number,
defect
size,
clinical
symptoms
and
uterine
position.
Ultrasound
Obstet
Gynecol.
2009
Jul;34(1):85-9.
doi:
10.1002/uog.6405.
3.
Ushtagi
P,
Garepalli
S.
Sonographic
assessment
of
lower
uterine
segment
at
term
in
women
with
previous
cesarean
delivery.
Arch
Gynecol
Obstet.
2011
Mar;283(3):455-9.
doi:
10.1007/s00404-010-1384-6.
Epub
2010
Feb
10.
4.
Landon
MB.
Predicting
uterine
rupture
in
women
undergoing
trial
of
labor
after
prior
cesarean
delivery.
Semin
Perinatol.
2010
Aug;34(4):267-71.
5.
Abdel
Baset
F.
Mohammed,
Diaa
A.
Al-Moghazi,
Mamdouh
T.
Hamdy,
Enas
M.
Mohammed.
Middle
East
Fertility
Society
Journal.2010;15:188-193.
6.
Cheung
VY.
Sonographic
measurement
of
the
lower
uterine
segment
thickness:
is
it
truly
predictive
of
uterine
rupture?
J
Obstet
Gynaecol
Can.
2008
Feb;30(2):148-51.
7.
Jastrow
N,
Chaillet
N,
Roberge
S,
Morency
AM,
Lacasse
Y,
Bujold
E.
Sonographic
lower
uterine
segment
thickness
and
risk
of
uterine
scar
defect:
a
systematic
review.
J
Obstet
Gynaecol
Can
2010;32(4):321-7.
8.
Rozenberg
P,
Goffinet
F,
Phillippe
HJ,
Nisand
I.
Ultrasonographic
measurement
of
lower
uterine
segment
to
assess
risk
of
defects
of
scarred
uterus.
Lancet
1996;347(8997):281-4.
9.
Jastrow
N,
Demers
S,
Chaillet
N,
Girard
M,
Gauthier
RJ,
Pasquier
JC,
et
al.
Lower
uterine
segment
thickness
to
prevent
uterine
rupture
and
adverse
perinatal
outcomes:
a
multicenter
prospective
study.
Am
J
Obstet
Gynecol
2016;215(5):604.e1-604.e6.
10.
Sharma
C,
Surya
M,
Soni
A,
Soni
PK,
Verma
A,
Verma
S.
Sonographic
prediction
of
scar
dehiscence
in
women
with
previous
cesarean
section.
J
Obstet
Gynaecol
India
2015;65(2):97-103.
11.
Uharcek
P,
Brestansky
A,
Ravinger
J,
Manova
A,
Zajacova
M.
Sonographic
assessment
of
lower
uterine
segment
thickness
at
term
in
women
with
previous
cesarean
delivery.
Arch
Gynecol
Obstet
2015;292(3):609-12.
12.
Brahmalakshmy
BL,
Kushtagi
P.
Variables
influencing
the
integrity
of
lower
uterine
segment
in
post-cesarean
pregnancy.
Arch
Gynecol
Obstet
2015;291(4):755-62.
13.
Barzilay
E,
Shay
A,
Lahav-Ezra
H,
Shina
A,
Perlman
S,
Achiron
R,
et
al.
Sonographic
assessment
of
the
lower
uterine
segment
during
active
labor
in
women
with
or
without
a
uterine
scar
-
a
prospective
study.
J
Matern
Fetal
Neonatal
Med
2017:1-4.
14.
Sambaziotis
H,
Conway
C,
Figueroa
R,
Elimian
A,
Garry
D.
Second-trimester
sonographic
comparison
of
the
lower
uterine
segment
in
pregnant
women
with
and
without
a
previous
cesarean
delivery.
J
Ultrasound
Med
2004;23(7):907-11;
quiz
913-4.
15.
Fukuda
M,
Fukuda
K,
Shimizu
T,
Bujold
E.
Ultrasound
Assessment
of
Lower
Uterine
Segment
Thickness
During
Pregnancy,
Labour,
and
the
Postpartum
Period.
J
Obstet
Gynaecol
Can
2016;38(2):134-40.
16.
Kushtagi
P,
Garepalli
S.
Sonographic
assessment
of
lower
uterine
segment
at
term
in
women
with
previous
cesarean
delivery.
Arch
Gynecol
Obstet
2011;283(3):455-9.
17.
Cheung
VY,
Constantinescu
OC,
Ahluwalia
BS.
Sonographic
evaluation
of
the
lower
uterine
segment
in
patients
with
previous
cesarean
delivery.
J
Ultrasound
Med
2004;23(11):1441-7.
18.
Sanlorenzo
O,
Farina
A,
Pula
G,
Zanello
M,
Pedrazzi
A,
Martina
T,
et
al.
Sonographic
evaluation
of
the
lower
uterine
segment
thickness
in
women
with
a
single
previous
Cesarean
section.
Minerva
Ginecol
2013;65(5):551-5.
19.
Kok
N,
Wiersma
IC,
Opmeer
BC,
de
Graaf
IM,
Mol
BW,
Pajkrt
E.
Sonographic
measurement
of
lower
uterine
segment
thickness
to
predict
uterine
rupture
during
a
trial
of
labor
in
women
with
previous
Cesarean
section:
a
meta-analysis.
Ultrasound
Obstet
Gynecol
2013;42(2):132-9.
20.
Martins
WP,
Barra
DA,
Gallarreta
FM,
Nastri
CO,
Filho
FM.
Lower
uterine
segment
thickness
measurement
in
pregnant
women
with
previous
Cesarean
section:
reliability
analysis
using
two-
and
three-dimensional
transabdominal
and
transvaginal
ultrasound.
Ultrasound
Obstet
Gynecol
2009;33(3):301-6.
21.
Sen
S,
Malik
S,
Salhan
S.
Ultrasonographic
evaluation
of
lower
uterine
segment
thickness
in
patients
of
previous
cesarean
section.
Int
J
Gynaecol
Obstet
2004;87(3):215-9.
|
|
.................................................................................................................

|
| |
|

