|
|
 |
| ............................................................. |
|
October 2017 -
Volume 15, Issue 8
|
 |
|
View
this issue in pdf formnat - the issue
has been split into two files for downloading
due to its large size: FULLpdf
(12 MB)
Part
1 &
Part
2
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
........................................................
|
|
Original Contribution/Clinical Investigation
Immunity
level to diphtheria in beta thalassemia patients
DOI: 10.5742/MEWFM.2017.93048
[pdf
version]
Abdolreza Sotoodeh Jahromi, Karamatollah Rahmanian,
Abdolali Sapidkar, Hassan Zabetian, Alireza
Yusefi, Farshid Kafilzadeh, Mohammad Kargar,
Marzieh Jamalidoust,
Abdolhossein Madani
Genetic
Variants of Toll Like Receptor-4 in Patients
with Premature Coronary Artery Disease, South
of Iran
DOI: 10.5742/MEWFM.2017.93049
[pdf
version]
Saeideh Erfanian, Mohammad Shojaei, Fatemeh
Mehdizadeh, Abdolreza Sotoodeh Jahromi, Abdolhossein
Madani, Mohammad Hojjat-Farsangi
Comparison
of postoperative bleeding in patients undergoing
coronary artery bypass surgery in two groups
taking aspirin and aspirin plus CLS clopidogrel
DOI: 10.5742/MEWFM.2017.93050
[pdf
version]
Ali Pooria, Hassan Teimouri, Mostafa Cheraghi,
Babak Baharvand Ahmadi, Mehrdad Namdari, Reza
Alipoor
Comparison
of lower uterine segment thickness among nulliparous
pregnant women without uterine scar and pregnant
women with previous cesarean section: ultrasound
study
DOI: 10.5742/MEWFM.2017.93051
[pdf version]
Taravat Fakheri, Irandokht Alimohammadi, Nazanin
Farshchian, Maryam Hematti,
Anisodowleh Nankali, Farahnaz Keshavarzi, Soheil
Saeidiborojeni
Effect
of Environmental and Behavioral Interventions
on Physiological and Behavioral Responses of
Premature Neonates Candidates Admitted for Intravenous
Catheter Insertion in Neonatal Intensive Care
Units
DOI: 10.5742/MEWFM.2017.93052
[pdf
version]
Shohreh Taheri, Maryam Marofi, Anahita Masoumpoor,
Malihe Nasiri
Effect
of 8 weeks Rhythmic aerobic exercise on serum
Resistin and body mass index of overweight and
obese women
DOI: 10.5742/MEWFM.2017.93053
[pdf
version]
Khadijeh Molaei, Ahmad Shahdadi, Reza Delavar
Study
of changes in leptin and body mass composition
with overweight and obesity following 8 weeks
of Aerobic exercise
DOI: 10.5742/MEWFM.2017.93054
[pdf
version]
Khadijeh Molaei, Abbas Salehikia
A reassessment
of factor structure of the Short Form Health
Survey (SF-36): A comparative approach
DOI: 10.5742/MEWFM.2017.93088
[pdf version]
Vida Alizad, Manouchehr Azkhosh, Ali Asgari,
Karyn Gonano
Population and Community Studies
Evaluation
of seizures in pregnant women in Kerman - Iran
DOI: 10.5742/MEWFM.2017.93056
[pdf
version]
Hossein Ali Ebrahimi, Elahe Arabpour, Kaveh
Shafeie, Narges Khanjani
Studying
the relation of quality work life with socio-economic
status and general health among the employees
of Tehran University of Medical Sciences (TUMS)
in 2015
DOI: 10.5742/MEWFM.2017.93057
[pdf version]
Hossein Dargahi, Samereh Yaghobian, Seyedeh
Hoda Mousavi, Majid Shekari Darbandi, Soheil
Mokhtari, Mohsen Mohammadi, Seyede Fateme Hosseini
Factors
that encourage early marriage and motherhood
from the perspective of Iranian adolescent mothers:
a qualitative study
DOI: 10.5742/MEWFM.2017.93058
[pdf
version]
Maasoumeh Mangeli, Masoud Rayyani, Mohammad
Ali Cheraghi, Batool Tirgari
The
Effectiveness of Cognitive-Existential Group
Therapy on Reducing Existential Anxiety in the
Elderly
DOI: 10.5742/MEWFM.2017.93059
[pdf
version]
Somayeh Barekati, Bahman Bahmani, Maede Naghiyaaee,
Mahgam Afrasiabi, Roya Marsa
Post-mortem
Distribution of Morphine in Cadavers Body Fluids
DOI: 10.5742/MEWFM.2017.93060
[pdf
version]
Ramin Elmi, Mitra Akbari, Jaber Gharehdaghi,
Ardeshir Sheikhazadi, Saeed Padidar, Shirin
Elmi
Application
of Social Networks to Support Students' Language
Learning Skills in Blended Approach
DOI: 10.5742/MEWFM.2017.93061
[pdf
version]
Fatemeh Jafarkhani, Zahra Jamebozorg, Maryam
Brahman
The
Relationship between Chronic Pain and Obesity:
The Mediating Role of Anxiety
DOI: 10.5742/MEWFM.2017.93062
[pdf
version]
Leila Shateri, Hamid Shamsipour, Zahra Hoshyari,
Elnaz Mousavi, Leila Saleck, Faezeh Ojagh
Implementation
status of moral codes among nurses
DOI: 10.5742/MEWFM.2017.93063
[pdf
version]
Maryam Ban, Hojat Zareh Houshyari Khah, Marzieh
Ghassemi, Sajedeh Mousaviasl, Mohammad Khavasi,
Narjes Asadi, Mohammad Amin Harizavi, Saeedeh
Elhami
The comparison
of quality of life, self-efficacy and resiliency
in infertile and fertile women
DOI: 10.5742/MEWFM.2017.93064
[pdf version]
Mahya Shamsi Sani, Mohammadreza Tamannaeifar
Brain MRI Findings in Children (2-4 years old)
with Autism
DOI: 10.5742/MEWFM.2017.93055
[pdf
version]
Mohammad Hasan Mohammadi, Farah Ashraf Zadeh,
Javad Akhondian, Maryam Hojjati,
Mehdi Momennezhad
Reviews
TECTA gene function and hearing: a review
DOI: 10.5742/MEWFM.2017.93065
[pdf version]
Morteza Hashemzadeh-Chaleshtori, Fahimeh Moradi,
Raziyeh Karami-Eshkaftaki,
Samira Asgharzade
Mandibular
canal & its incisive branch: A CBCT study
DOI: 10.5742/MEWFM.2017.93066
[pdf
version]
Sina Haghanifar, Ehsan Moudi, Ali Bijani, Somayyehsadat
Lavasani, Ahmadreza Lameh
The
role of Astronomy education in daily life
DOI: 10.5742/MEWFM.2017.93067
[pdf
version]
Ashrafoalsadat Shekarbaghani
Human brain
functional connectivity in resting-state fMRI
data across the range of weeks
DOI: 10.5742/MEWFM.2017.93068
[pdf version]
Nasrin Borumandnia, Hamid Alavi Majd, Farid
Zayeri, Ahmad Reza Baghestani,
Mohammad Tabatabaee, Fariborz Faegh
International Health Affairs
A
brief review of the components of national strategies
for suicide prevention suggested by the World
Health Organization
DOI: 10.5742/MEWFM.2017.93069
[pdf
version]
Mohsen Rezaeian
Education and Training
Evaluating
the Process of Recruiting Faculty Members in
Universities and Higher Education and Research
Institutes Affiliated to Ministry of Health
and Medical Education in Iran
DOI: 10.5742/MEWFM.2017.93070
[pdf
version]
Abdolreza Gilavand
Comparison
of spiritual well-being and social health among
the students attending group and individual
religious rites
DOI: 10.5742/MEWFM.2017.93071
[pdf
version]
Masoud Nikfarjam, Saeid Heidari-Soureshjani,
Abolfazl Khoshdel, Parisa Asmand, Forouzan Ganji
A
Comparative Study of Motivation for Major Choices
between Nursing and Midwifery Students at Bushehr
University of Medical Sciences
DOI: 10.5742/MEWFM.2017.93072
[pdf
version]
Farzaneh Norouzi, Shahnaz Pouladi, Razieh Bagherzadeh
Clinical Research and Methods
Barriers
to the management of ventilator-associated pneumonia:
A qualitative study of critical care nurses'
experiences
DOI: 10.5742/MEWFM.2017.93073
[pdf version]
Fereshteh Rashnou, Tahereh Toulabi, Shirin Hasanvand,
Mohammad Javad Tarrahi
Clinical
Risk Index for Neonates II score for the prediction
of mortality risk in premature neonates with
very low birth weight
DOI: 10.5742/MEWFM.2017.93074
[pdf
version]
Azadeh Jafrasteh, Parastoo Baharvand, Fatemeh
Karami
Effect
of pre-colporrhaphic physiotherapy on the outcomes
of women with pelvic organ prolapse
DOI: 10.5742/MEWFM.2017.93075
[pdf
version]
Mahnaz Yavangi, Tahereh Mahmoodvand, Saeid Heidari-Soureshjani
The
effect of Hypertonic Dextrose injection on the
control of pains associated with knee osteoarthritis
DOI: 10.5742/MEWFM.2017.93076
[pdf
version]
Mahshid Ghasemi, Faranak Behnaz, Mohammadreza
Minator Sajjadi, Reza Zandi,
Masoud Hashemi
Evaluation
of Psycho-Social Factors Influential on Emotional
Divorce among Attendants to Social Emergency
Services
DOI: 10.5742/MEWFM.2017.93077
[pdf
version]
Farangis Soltanian
Models and Systems of Health Care
Organizational
Justice and Trust Perceptions: A Comparison
of Nurses in public and private hospitals
DOI: 10.5742/MEWFM.2017.93078
[pdf
version]
Mahboobeh Rajabi, Zahra Esmaeli Abdar, Leila
Agoush
Case series and Case reports
Evaluation
of Blood Levels of Leptin Hormone Before and
After the Treatment with Metformin
DOI: 10.5742/MEWFM.2017.93079
[pdf
version]
Elham Jafarpour
Etiology,
Epidemiologic Characteristics and Clinical Pattern
of Children with Febrile Convulsion Admitted
to Hospitals of Germi and Parsabad towns in
2016
DOI: 10.5742/MEWFM.2017.93080
[pdf
version]
Mehri SeyedJavadi, Roghayeh Naseri, Shohreh
Moshfeghi, Irandokht Allahyari, Vahid Izadi,
Raheleh Mohammadi,
Faculty development
The
comparison of the effect of two different teaching
methods of role-playing and video feedback on
learning Cardiopulmonary Resuscitation (CPR)
DOI: 10.5742/MEWFM.2017.93081
[pdf
version]
Yasamin Hacham Bachari, Leila Fahkarzadeh, Abdol
Ali Shariati
Office based family medicine
Effectiveness
of Group Counseling With Acceptance and Commitment
Therapy Approach on Couples' Marital Adjustment
DOI: 10.5742/MEWFM.2017.93082
[pdf
version]
Arash Ziapour, Fatmeh Mahmoodi, Fatemeh Dehghan,
Seyed Mehdi Hoseini Mehdi Abadi,
Edris Azami, Mohsen Rezaei
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| October 2017 -
Volume 15, Issue 8 |
|
|
Mandibular canal and
its incisive branch: A CBCT study
Sina Haghanifar (1)
Ehsan Moudi (2)
Ali Bijani (3)
Somayyehsadat Lavasani (4)
Ahmadreza Lameh (5)
(1) Oral and Maxillofacial Radiology Department,
Dental School, Babol University of Medical Science,
Babol, Iran
(2) Oral and Maxillofacial Radiology Department,
Dental School, Babol University of Medical Science,
Babol, Iran
(3) Social Determinants of Health Research Center,
Babol University of Medical Sciences, Babol,
Iran
(4) Oral and Maxillofacial Radiology Department,
Dental School, Babol University of Medical Science,
Babol, Iran
(5) Radiology Department, Medical School, Mashhad
University of Medical Sciences, Mashhad, Iran
Correspondence:
Somayyehsadat Lavasani*
Oral and Maxillofacial Radiology Department,
Dental School, Babol University of Medical Science,
Babol, Iran
Email : roya_lavasani@yahoo.com
|
Abstract
Objective: Prevention
from damage to the mandibular canal (MC)
during invasive dental procedures is essential.
The aim of this study was to determine
the course of MC, anterior branch and
its relation to mandibular teeth.
Materials and
Methods: In cross-sectional view,
the MC diameter, the distance from root
apex to MC, the distance of MC to mandibular
lower border, the distance of MC from
buccal and lingual cortical borders, from
the distal root of third molar to first
premolar in apex roots area of all posterior
teeth were identified by using 207 CBCT
images. The presence of the anterior loop,
the position of mental foramen, position
and diameter of incisive branch on the
last visible point were also determined.
Examples were divided into the groups
in terms of age, sex and side and were
analyzed with descriptive statistics.
Results: The
nearest root to the MC was the distal
root of third molar in women less than
30 years (0.38±0.58 mm) and the
most distant root was the second premolar
tooth in men 30-50 years (6.06±2.20
mm). The most common site for mental foramen,
was between premolars and the area between
the first premolar and canine teeth was
the most common site for incisive canal
on the last point of view. There was no
significant differences between right
and left mandibular measurements.
Conclusion:
The position of MC towards mandibular
posterior teeth is more influenced by
age and sex. Also, the position of MC
towards the bucco-lingual plate depends
on the antero-posterior position of mental
foramen. So any procedures in the mandibular
posterior area should be performed with
sufficient knowledge of the nervous canal.
Key words:
Anatomy, Mandibular canal, Mental foramen,
Incisive canal, CBCT
|
According to various mandibular surgeries,
such as removing impacted third molar to implant
placement, awareness of the position of inferior
alveolar nerve is essential to ensure no damage
to the nerve. (1,2). To achieve a successful
treatment plan, adequate knowledge of the mandibular
canal (MC) course and tooth roots is essential
to reduce procedure bias (3). So, it is important
to be aware of MC anatomy and possible variations
in position, shape and course of canal for local
anesthesia and during surgery (4). MC contains
artery and inferior alveolar nerve, which have
branches to the mandibular teeth and adjacent
structures. MC can exhibit important anatomical
variations and may be affected by inflammatory,
infectious, neoplastic, idiopathic or iatrogenic
lesions (5,6).
Full knowledge of anatomical structures in
mental foramen area and the anterior loop is
essential to prevent direct or indirect injury
to the neurovascular bundle (7-9). Also, if
the treatment plan includes surgical procedures
in the area between mental and lingual foramen,
the incisive branch of inferior alveolar nerve
must be considered (9).In a study conducted
in 2008 to evaluate the prognosis of mandibular
molars apical surgeries, it was found that patients
experienced more pain when the lesions were
within 2 mm of the canal as depicted on a panoramic
radiograph and there was a 19.4 % failure rate
for lesions close to the canal. So, the accurate
knowledge of the MC location can be useful not
only during surgery, but also in the prognosis
for surgery and evaluation of the patient’s
post-operative situation (10).
Findings from studies using cadavers may not
be generalized to patient populations due to
differences in age or disease. Dry skull studies
often lack relevant data such as age or gender
(11,12). Based on the results of studies that
tried to compare the measurements made by the
CBCT images and direct measurements on human
samples, it was indicated that CBCT scans are
excellent evaluation tools for the canal observations,
which is similarly matched the anatomical measurements
(10). Position of inferior alveolar canal and
its connections have been described for a very
long time, and many studies reported that the
characteristics of these structures seem to
be associated with race. For example, the mental
foramen were often variable in position or even
completely absent in some rare cases in different
populations (13). Previous studies on human
populations were more focused on the anatomical
traits, while the relationship of these structures
with each other and their relationship with
the teeth apexes have been less described (3,13-18).
The aim of this study was to evaluate the MC
course and its anterior branch, and the impact
of factors such as age, sex and side on canal
status.
In this cross-sectional study, 207 mandibular
scans of patients over 18 years (110 female
and 97 male) with a mean age of 45.7±13.83
years, during 2013-2015 who referred to the
maxillofacial radiology center were used. All
scans were performed using Cranex 3D (Soredex,
Helsinki, Finland) with Flat panel detector
with the specifications of KVP=89, mA=6, Voxel
size=0.2 mm and FOV=8 × 6 cm. The images
were assessed using a personal monitor Macbook
Air MD 760 (Apple Ltd, California, USA) with
LCD 13-inch, Pix Resolution 900 × 1440
and assessed by Ondem and 3D Dental software.
Scans were examined by a maxillofacial radiologist
to evaluate the relationship between MC and
mandibular posterior teeth. Exclusion criteria
included: 1. Any pathosis around teeth or in
the mandibular body which can disturb the measurements
2. Supernumerary or impacted teeth in the mandible
3. Third molars with horizontal positions in
the mandible 4. Single root molars in the mandible.
Measurements were started in the cross-sectional
view (Interval =1 mm, Thickness =1 mm), if there
was a distal root of third molar, and the MC
diameter (D), the minimum distance of apex to
superior border of MC (AP), the distance from
inferior border of MC to the inferior border
of the mandible (IC), the distance of MC from
the cortical buccal border (BC) and the distance
of MC from the cortical lingual border of mandible
(LC) was traced (Figure 1). The bone width in
the MC area (W) was also calculated by the sum
of D, BC and LC. Then the same measurements
were made again on the third molar mesial root
and measurements continued forward on all posterior
teeth roots to the first premolar. The measurements
were made on both sides of the mandible. In
the examination of mental foramen, its location
and the presence or absence of anterior loop
was evaluated. The diameter and position of
incisive branch was evaluated at the last visible
point.
The subjects were divided into three age groups:
Group I (18-30 years = 34 patients), Group II
(30-50 years = 87 patients) and Group III (over
50 years = 86 patients). The samples were separated
according to gender and side. Data were analyzed
using three ways (gender, age, side) by statistical
tests: T-Test, ANOVA and SPSS version 18. P-value
less than 0.05 was considered statistically
significant.
Among 207 patients under this study, the results
showed that the distance of MC from posterior
teeth apex, the nearest root was the distal
root of third molar in women less than 30 years
(0.38±0.58 mm) and the most distant root
was second premolar tooth in men 30-50 years
(6.06±2.20 mm). This distance in women
was significantly less than men (P <0.05)
(Table 1 and Figure 2) and under age 30 years
was also significantly less than other age groups
(P <0.05).
Table 1: The prevalence and rate of incisive
canal at the last visible point according to
gender and position
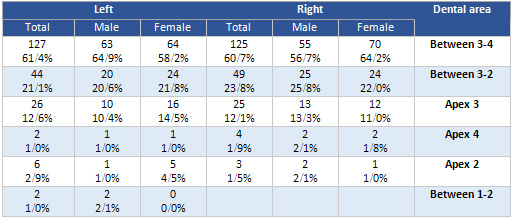
Figure 1: measurements in posterior teeth
roots area in Cross-sectional view, D: MC diameter,
AP: distance from root apex to superior border
of MC, IC: distance from inferior border of
MC to mandibular inferior border, BC: distance
from MC to buccal cortical border, LC: distance
from MC to lingual cortical border.
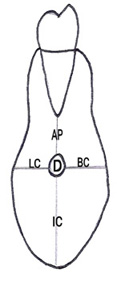
Figure 2: The path of measurements according
to gender
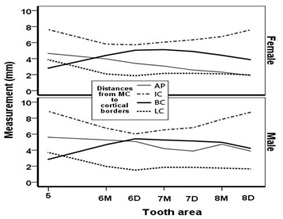
Figure 3: The mandibular width in MC area
of posterior teeth according to age and gender
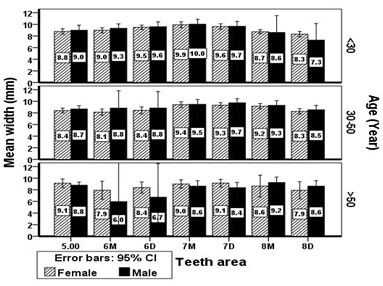
Figure 4: The mandibular canal diameter in posterior
teeth
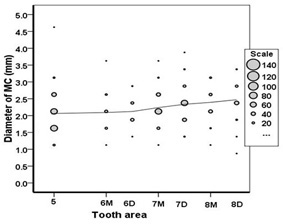
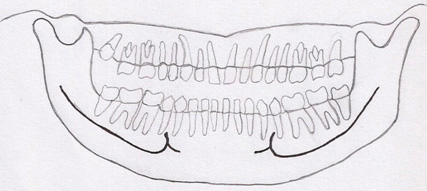
Figure 5: The course of MC in horizontal
schematic view

Figure 6: The course of MC in schematic panoramic
view
Click here for
Table 2: The measured
distances of MC in mandibular posterior teeth
according to gender
Minimum and maximum distance of MC from inferior
mandibular cortex belonged to the distal root
of the third molar in women over 50 years (4.66±0.52mm),
and second premolar tooth in men over 50 years
(9.29±1.94mm) respectively. This distance
was lower in women than men (P<0.05) (Table
1 and Figure 2) and under age 30 years was also
significantly less than other age groups (P<0.05).
In the assessment of MC distance from buccal
and lingual cortical borders, the minimum buccal
distance belonged to the second premolar tooth
in women over 50 years (2.49±0.94mm),
and the minimum lingual distance was located
in the distal root of third molars in women
over 50 years (0.90±0.32mm). These measured
distances were significantly lower in women
than men (P<0.05) (Table 1 and Fig 2) and
it was observed that the distance of canal to
the buccal cortical plate in patients over 50
years was less than other age groups (P<0.05).
The maximum horizontal bone width at MC area
(10.22±1.15mm) was the mesial root of
second molar in men under 30. Bone width in
this area was significantly lower in women than
men (P<0.05) (Table 1); and in patients over
50 years, it was significantly less than other
age groups (P<0.05) (Figure 3).
It was observed that the minimum MC diameter
on average was in the second premolar tooth
in women 30-50 years (1.80±0.37mm), and
the highest diameter on average was the distal
root of the third molars in men 30-50 years
(2.75±0.54mm). Over all, the MC diameter
had a similar pattern in both sexes and three
age groups from posterior to anterior. So that,
the diameter was higher in posterior and it
was reduced with a gentle slope to the anterior
area (Figure 4).
The area between premolars was the most common
site for the presence of mental foramen on the
right (69.6%) and left (62.3%) side. Then, the
second premolar apex, distal of second premolar
and first premolar apex were located, respectively.
197 patients (95.2%) had anterior loop on both
sides, in which, it was found that age and gender
have no significant effect on the presence of
loop and mental foramen position. In incisive
canal examinations, it was observed that the
average canal diameter on the last visible point
was 1.12±0.31 mm and 1.06±0.28
mm on right and left side respectively. The
most common area on the last point of view for
incisive canal, according to its frequency,
was on the right (60.4%) and left (61.4%) side
between the first premolar and canine. After
that, there was an area between the canine and
lateral teeth. In both sides lateral incisor
apex, was the lowest region to end its canal.
Also, no relationship was observed between age
and sex with incisive canal diameter and its
location (Table 2).
Secondary findings from this study showed that
11 patients had bifid canal, in which 3 cases
had two bifid canals on both sides. When this
occurred the closest MC to the cortical plates
was used for measurements. 12 patients had accessory
mental foramen, in which 4 cases had multiple
mental foramen on both sides. The MC course
was started from an area near the lingual plate
of posterior mandibular teeth and in the second
premolar tooth reached to the mid bucco-lingual
plate. In the vertical dimension, canal was
closer to the posterior teeth roots than inferior
cortex. Regardless of age and sex, there was
no significant difference between all measured
distances in the left and right sides (Figure
5).
The
results
of
this
study
on
the
distance
of
MC
from
posterior
teeth
roots
showed
that
the
distal
root
of
third
molar
was
the
closest
root
to
canal,
so
that,
the
average
distance
between
the
left
and
right
sides
was
2.88
and
2.49
mm,
respectively.
By
moving
towards
the
anterior
area,
the
canal
gets
farther
away
from
posterior
teeth
apex,
so
that,
the
average
distance
of
mesial
root
of
the
first
molar
on
the
left
and
right
sides
was,
3.96
to
4.64
mm,
respectively.
Fewer
studies
were
performed
to
examine
the
distance
of
the
third
molars
roots
from
MC,
and
most
studies
in
this
field
only
tried
to
examine
the
canal
course
in
the
impacted
and
unerupted
third
molar
area
(19,
20).
Chong
et
al.
on
272
second
mandibular
molars,
reported
that
in
55%
of
cases,
the
distance
between
the
root
apex
and
inferior
alveolar
nerve
was
less
and
equal
to
3
mm,
which
is
close
to
the
results
of
this
study
(21).
Simonton
in
a
study
reported
that
the
distance
of
MC
from
mesial
root
of
first
molar
was
4.9
mm
in
women
and
6.2
mm
in
men,
which
is
closely
consistent
with
the
results
of
this
study
(22).
In
this
study,
MC
distance
from
the
inferior
mandibular
cortex
in
the
distal
root
of
third
molar
area
was
7.52
to
8.41
mm
on
the
right
and
left
sides
respectively,
and
this
distance
decreased
gradually
by
moving
forward
to
the
mesial
root
of
first
molar
and
increased
again
in
the
premolar
area.
Rajchel
et
al.
in
a
study
on
cadavers
reported
that
this
distance
was
mm10
in
the
third
molar
area
(23);
with
respect
to
the
fact
that
mandibular
form
vary
in
different
people
and
in
different
age
ranges,
so
the
differences
in
measurement
seems
normal.
Also
in
this
study,
it
was
observed
that
MC
was
closer
to
the
apex
of
posterior
teeth
rather
than
the
inferior
mandibular
cortex.
Sato
in
a
study
on
panoramic
images
indicated
that
the
MC
course
in
the
vertical
dimension
was
closer
to
the
apex
of
first
and
second
molars
rather
than
inferior
mandibular
cortex
(24).
The
MC
distance
from
buccal
and
lingual
cortical
borders,
it
was
observed
that
distal
root
of
third
molar
was
the
closest
root
to
lingual
plate
and
the
second
premolar
tooth
was
the
closest
root
to
buccal
plate.
The
average
distance
of
MC
to
the
lingual
cortical
plate
in
the
distal
root
of
third
molar
was
1.64
and
1.98
mm
on
the
right
and
left
sides,
respectively.
In
Rajchel’s
study,
the
canal
in
the
third
molar
area
had
approximately
2mm
distance
from
the
lingual
plate,
which
is
very
close
to
our
results
(23).
In
the
present
study
the
average
distance
of
MC
from
buccal
cortex
in
the
mesial
root
of
the
first
molar
was
4.44
and
4.53
mm
on
the
right
and
left
sides,
respectively.
Leith
et
al.
in
a
study
on
157
CBCT
images
of
patients
with
a
mean
age
of
48
years,
this
distance
was
4.4
mm
in
75%
of
cases,
which
is
very
close
to
the
results
of
this
study
(5).
For
the
MC
diameter,
it
was
observed
that
the
average
minimum
and
maximum
canal
diameter
was
1.80
and
2.75mm
in
second
premolar
and
the
distal
root
of
third
molar,
respectively.
Canal
diameter
from
the
posterior
to
the
anterior
decreased
with
a
gentle
slope.
Rajechel
demonstrated
that
when
proximal
to
the
third
molar,
MC
diameter
was
2
to
2.4
mm.
on
measurements
obtained
from
105
mandibular
cadavers;
Obradovic
et
al.
also
found
that
the
mean
MC
diameter
in
its
horizontal
part
was
2.6
mm,
which
is
closely
consistent
with
these
results
(23).
One
of
the
common
but
inadvertant
complications
in
the
anterior
mandible
during
implant
placement
is
neurosensory
alteration.
Mental
foramen
shows
many
anatomical
variations
in
shape,
size
and
position.
In
the
present
study,
95.2%
of
patients
had
anterior
loop
and
the
area
between
premolars
on
both
sides
was
the
most
common
site
for
that.
Investigations
that
compared
radiographic
and
cadaveric
dissection
data
with
respect
to
identifying
the
anterior
loop
reported
that
radiographic
assessments
result
in
a
high
percentage
of
false-positive
and
false-negative
findings
(25).
Perhaps
these
varied
results
may
be
attributed
to
different
criteria
used
to
define
the
anterior
loop
and
dissimilar
diagnostic
techniques.
Arzouman
showed
92
to
96%
of
direct
measurements
on
cadavers
had
detected
anterior
loop,
while
only
56
to
76
%
of
the
panoramic
machines
showed
the
loop
(25).
With
regard
to
the
mental
foramen,
apex
of
the
second
premolars
or
the
area
between
premolars
have
been
reported
as
the
most
common
site
for
that.
In
the
study
by
Haqhanifar
et
al.
on
panoramic
images,
the
area
between
premolars
was
the
most
common
area
for
mental
foramen,
which
is
consistent
with
the
results
of
this
study
(14).
The
mean
incisive
canal
diameter
in
the
last
visible
point
was
1.12±0.31mm
on
the
right
and
1.06±0.28mm
on
the
left
side.
Jacobs
et
al.
examined
230
spiral
CT
where
the
incisive
canal
was
identified
in
93%
of
the
cases,
and
they
reported
the
average
inner
diameter
was
1.1
mm,
which
is
consistent
with
our
results
(25).
For
assessing
the
amount
of
incisive
branch
progression,
an
area
between
the
first
premolar
and
canine
teeth
was
observed
as
the
most
common
visible
area
for
that
on
both
sides.
Most
studies
have
investigated
quantitative
measures
of
incisive
nerve
length
and
there
is
no
study
that
has
tried
to
investigate
the
progression
level
of
the
canal
compared
to
other
surrounding
anatomic
structures.
Mardinger
et
al.
have
examined
anatomical
and
radiographic
course
of
incisive
canal
in
46
cadaver
mandibles,
they
found
that
the
canal
walls
in
some
cases
were
complete,
some
incomplete
and
in
others
without
corticated
limits.
They
concluded
that
there
are
correlations
between
the
anatomical
structure
and
visible
radiographic
limits(26).
The
visibility
or
invisibility
of
incisive
canal
largely
depends
on
racial
differences,
radiologists’
experiences
and
radiographic
technique.
Pieres
et
al.
showed
that
the
incisive
canal
is
better
seen
in
CBCT
images
rather
than
panoramic
radiography.
They
reported
the
average
length
of
incisive
canal
was
about
7±3.8mm
(27).
This
distance
is
almost
where
the
mandibular
canine
apex
can
be
placed.
The
results
of
this
study
are
very
close
to
our
results.
For
the
assessment
of
gender
effect
on
the
measured
distances,
it
was
found
that
the
overall
pattern
of
MC
course
was
similar
in
both
genders,
but
in
general
women
have
lesser
distances
than
men,
which
is
consistent
with
results
of
other
studies
in
this
domain
(22,
28).
About
the
influence
of
age
on
the
measured
points,
it
was
observed
that
the
average
distance
of
MC
from
root
apex
and
from
the
lower
mandibular
border
was
significantly
less
in
under
30
years
than
other
age
groups;
Given
that
skeletal
growth
in
these
patients
is
not
yet
complete,
this
result
is
justified.
It
was
also
observed
that
in
patients
over
age
50,
bone
width
was
slightly
less
than
other
age
groups,
and
according
to
the
first
molar
was
the
most
missing
tooth
in
this
age
group;
reduced
bone
width
was
more
evident
in
this
area.
Simonton
et
al.
have
also
reported
reduced
bone
width
in
patients
in
their
50s-60s
(22).
Perhaps
the
rationale
reason
is
that
older
patients
have
generally
less
bone
mass
than
the
younger
age
groups.
It
should
be
mentioned,
CBCT
images
in
horizontal
and
vertical
planes
can
help
in
the
examination
of
the
MC
course,
because
the
canal
can
pass
different
courses
in
each
view
for
different
patients.
Anderson
et
al.
in
a
study
on
panoramic
radiographs
found
that
the
MC
may
slowly
come
down
from
anterior
to
posterior
or
have
a
gentle
progressive
curve,
or
even
a
combination
of
these
two
(23).
Also,
in
the
horizontal
plane
the
canal
course
extends
from
lingual
to
the
buccal
border,
which
in
most
cases,
the
canal
in
the
first
molar
area
is
in
the
middle
distance
between
the
bucco-lingual
plates
(23).
In
the
present
study,
the
second
premolar
apex
was
located
in
the
middle
of
bucco-lingual
plates;
given
that
in
this
study,
the
most
common
area
for
mental
foramen
was
between
premolar
teeth,
it
is
justified.
As
Simonton
said
that
as
the
mental
foramen
became
more
distally
positioned,
the
MC
became
more
buccally
located
within
the
mandible,
and
in
relation
to
the
roots
of
the
mandibular
first
molar
(22).
This
study
was
conducted
on
adult
patients
most
images
taken
due
to
the
replacement
of
single
edentulous
area
and
there
are
a
few
studies
that
tried
to
examine
the
relationship
between
canal
and
all
mandibular
posterior
teeth
by
CBCT
imaging,
and
this
is
one
of
the
salient
points
of
this
study.
However,
given
that
in
this
study,
measurements
were
performed
on
patients
with
partial
and
complete
tooth,
and
classification
of
the
age
groups
needed
more
details,
this
limitation
cannot
be
forgotten.
It
is
recommended
to
perform
further
investigation
with
a
greater
sample
size
with
complete
teeth
and
considering
panoramic
and
CBCT
images
can
have
many
clinical
benefits
during
surgical
procedures
in
this
area.
The
appropriate
sensitivity
and
specificity
of
CBCT
in
the
detection
of
these
alterations
reinforces
its
use
in
oral
and
maxillofacial
radiology,
and
since
the
bone
dimensions
are
not
fixed
in
one’s
life,
providing
CBCT
before
surgery
is
necessary.
According
to
this
study
an
important
consideration
in
pre-surgical
planning
is
that
the
measurements
obtained
from
a
CBCT
scan
will
not
stay
constant
throughout
a
person’s
lifetime,
and
a
current
CBCT
might
be
recommended
before
surgical
treatment.
Collectively
these
data
indicate
that
both
age
and
gender
have
a
marked
effect
on
anatomic
relationship
and
should
be
considered
in
pre-surgical
treatment.
Acknowledgment
We
would
like
to
thank
the
Scientific
Research
Foundation
in
Babol
University
of
Medical
Sciences
for
supporting
this
research.
1.
Main
Q,
Yaxiong
L,
Ling
W,
Jiankang
H,
Ming
X,
Chengge
H.
Design
and
optimization
of
the
fixing
plate
for
customized
mandible
implant.
J
CMFS.
2015
DOI:
org/10.1016/i.icmfs.
20150060003
2.
Schneider
T,
Filo
K,
Kruse
AL,
Locher
M,
Gratz
KW,
Lubbers
HT.
Variations
in
the
anatomical
positioning
of
impacted
mandibular
wisdom
teeth
and
their
practical
implications.
J
Research
and
Science.
2014;
5:
(124):
520-529.
3.
Torres
A,
Jacobs
R,
Lambrechts
P,
Brizuela
C,
Cabera
C,
Concha
G
et
al.
Characterization
of
mandibular
molar
root
and
canal
morphology
using
cone
beam
computed
tomography
and
it’s
variability
in
Belgian
and
Chilean
samples.
J
Imaging
science
in
dentistry.
2015;
45:
95-101
4.
Khojastepour
L,
Mirbeigi
S,
Mirhadi
S,
Safaee
A.
Location
of
mental
foramen
in
a
selected
Iranian
population:
a
CBCT
assessment.
Iranian
Endodontic
journal.
2015;
10(2):
117-21
5.
Leite
MF,
Lana
JP,
Machado
VC,
Manzi
FR,
Souza
PEA,
Horta
MCR.
Anatomic
variations
and
lesions
of
the
mandibular
canal
detected
by
cone
beam
computed
tomography.
J
SurgRadiol
Anat.
2013;
DOI:
10.1007/s
00276-013-1247-5
6.
Tyler
K,
Mansur
A,
Walter
RB.
Proximity
of
the
mandibular
canal
to
the
tooth
apex.
JOE.
2011;
37:
311-315
7.
Yoshioka
I,
Tatsurou
T,
Khanal
A,
Habu
M,
Kito
S,
Kodama
M,
et
al.
Relationship
between
inferior
alveolar
nerve
canal
position
at
mandibular
second
molar
in
patient
with
prognathism
and
possible
occurence
of
neurosensory
disturbance
after
saggital
split
ramus
osteotomy.
J
Oral
Maxillofacial
Surg.
2010;
68:
3022-27
8.
Orhan
K,
Aksay
S,
Bilecenoglu
B,
Sakul
UB,
Paksoy
CS.
Evaluation
of
bifid
mandibular
canals
with
cone-beam
computed
tomography
in
Turkish
adult
population:
a
retrospective
study.
J
SurgRadiol
Ant.
2011;
33:
501-7
9.
Kyounq
YS,
Kim
S,
Kang
SG,
Kim
JH,
Lim
KO,
Hwang
SI
et
al.
Morphological
assessment
of
the
anterior
loop
of
the
mandibular
canal
in
Koreans.
J
Anatomy
and
Cell
Biology.
2015;
DOI:
Org/10.5115/acb.2015.48.1.75
10.
Kim
TS,
Caruso
JM,
Christensen
H,
Torabinejad
M.
A
comparison
of
cone-beam
computed
tomography
and
direct
measurement
in
the
examination
of
the
mandibular
canal
and
adjacent
structures.
JOE.
2010;
36:
1191-94
11.
Angel
JS,
Mincer
HH,
Chaudhry
J,
Scarbecz
M.
Cone-beam
computed
tomography
for
analyzing
variations
in
inferior
alveolar
canal
location
in
adults
in
relation
to
age
and
sex.
J
Forensic
Sci.
2011;
56(1):
216-19
12.
Levin
MH,
Goddard
AL,
Dodson
TB.
Inferior
alveolar
nerve
canal
position:
a
clinical
and
radiographic
study.
J
Oral
Maxillofacial
Surg.
2007;
65(3):
470-90
13.
Yun
X,
Ning
S,
Xiufen
T,
Fei
L,
Guangxin
Z,
Xioaoran
L
et
al.
Anatomic
study
on
mental
canal
and
incisive
nerve
canal
in
interforaminal
region
in
Chinese
population.
J
SurgRadiol
Ant.
2014;
DOI:
10.1007/s00276-014-1402-7
14.
Haghanifar
S,
Rokouei
M.
Radiographic
evaluation
of
mental
foramen
in
a
selected
Iranian
population.
J
Indian
Jur
of
Dent
Research.
2009;
20:
150-52
15.
Green
RM.
The
position
of
the
mental
foramen:
a
comparison
between
the
southern
(Hong
Kong)
Chinese
and
other
ethnic
and
racial
groups.
J
Oral
Surg
Oral
Med
Oral
Pathol.
1987;
63(3):
287-90
16.
Guo
JL,
Su
L,
Zhao
JL,
Yang
L,
Lv
DL,
Li
YQ
et
al.
Location
of
mental
foramen
based
on
soft
and
hard
tissues
landmarks
in
a
Chinese
population.
J
Craniofac
Surg.
2009;
20(6):
2235-37
17.
Santini
A,
Alayan
I.
A
comparative
anthropometric
study
of
the
position
of
the
mental
foramen
in
three
populations.
Br
Dent
J.
2012;
212(4):
E7
18.
Santini
A,
Land
M.
A
comparative
of
the
position
of
the
mental
foramen
in
Chinese
and
British
mandibles.
ActaAnat
J.
1990;
137(3):
208-12.
19.
Dalili
Z,
Mahjoub
P,
Khalighi
AS.
Comparison
between
cone
beam
computed
tomography
and
panoramic
radiography
in
the
assessment
of
the
relationship
between
the
mandibular
canal
and
impacted
class
c
mandibular
third
molars.
J
Dental
Research.
2011;
8(4):
203-210
20.
Jung
YH,
Nah
KS,
Cho
BH.
Correlation
of
panoramic
radiographs
and
cone
beam
computed
tomography
in
the
assessment
of
a
superimposed
relationship
between
the
mandibular
canal
and
impacted
third
molars.
J
Imaging
Science
in
Dentistry.
2012;
42:121-7
21.
Chong
BS,
Quinn
A,
Pawar
RR,
Makdissi
J,
Sidhu
Sk.
The
anatomical
relationship
between
the
roots
of
mandibular
second
molars
and
the
inferior
alveolar
nerve.
J
International
Endodontic.
2014;
DOI:10.1111/iej.12348
22.
Simonton
JD,
Azevedo
B,
Schindler
WG,
Hargreaves
KM.
Age
and
gender
related
differences
in
the
position
of
the
inferior
alveolar
nerve
by
using
cone
beam
computed
tomography.
JOE.
2009;
35(7):944-49
23.
Joudzbalys
G,
Wang
HL,
Sabalys
G.
Anatomy
of
mandibular
vital
structures.
Part
II
:
Mandibular
canal
and
inferior
neurovascular
bundle
in
relation
with
dental
implantology.J
Oral
Maxillofac
Res.2010;DOI:10.5037/jomr.2010.1102
24.
Sato
I,
Ueno
R,
Kawai
T,
Yosue
T.
Rare
courses
of
the
mandibular
canal
in
the
molar
regions
of
the
human
mandible:
a
cadaveric
study.
J
Okajimas
Folia
AnatJpn.
2005;
82(3):95-101.
DOI:10
2535/
ofaj.
82.95
25.
Joudzbalys
G,
Wang
HL,
Sabalys
G.
Anatomy
of
mandibular
vital
structures.
Part
II:
Mandibular
incisive
canal,
mental
foramen
and
associated
neurovascular
bundles
in
relation
with
dental
implantology.
J
Oral
Maxillofac
Res.2010;
DOI:10.5037/jomr.2010.1103
26.
Mardinger
O,
Chaushu
G,
Arensburg
B,
Taicher
S,
Kaffe
I.
Anterior
loop
of
mental
Canal:
an
anatomical
–
Radiologic
Study.
Implant
Dent.
2009;
9(2):
120-5.
27.
Pieres
CA,
Bissada
NF,
Becker
JJ,
Kanawati
A,
Landres
MA.
Mandibular
Incisive
Canal:
Cone
Beam
Computed
Tomography.
Clin
Implant
Dent
Relat
Res.
2009
Aug6;
DoI:10.1111j.1708-8208.
2009.00228.n
28.
Adiguzel
O,
yigit-ozer
S,
Kaya
S,
Akkus
Z.
Patient
specific
factors
in
the
proximity
of
the
inferior
alveolar
nerve
to
the
tooth
apex.
J
Med
Oral
Pathol
Oral
Cir
Bucal.
2012;
DoI:10.4317/medoral.18190
|
|
.................................................................................................................

|
| |
|

