|
|
 |
| ............................................................. |
|
October 2017 -
Volume 15, Issue 8
|
 |
|
View
this issue in pdf formnat - the issue
has been split into two files for downloading
due to its large size: FULLpdf
(12 MB)
Part
1 &
Part
2
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
........................................................
|
|
Original Contribution/Clinical Investigation
Immunity
level to diphtheria in beta thalassemia patients
DOI: 10.5742/MEWFM.2017.93048
[pdf
version]
Abdolreza Sotoodeh Jahromi, Karamatollah Rahmanian,
Abdolali Sapidkar, Hassan Zabetian, Alireza
Yusefi, Farshid Kafilzadeh, Mohammad Kargar,
Marzieh Jamalidoust,
Abdolhossein Madani
Genetic
Variants of Toll Like Receptor-4 in Patients
with Premature Coronary Artery Disease, South
of Iran
DOI: 10.5742/MEWFM.2017.93049
[pdf
version]
Saeideh Erfanian, Mohammad Shojaei, Fatemeh
Mehdizadeh, Abdolreza Sotoodeh Jahromi, Abdolhossein
Madani, Mohammad Hojjat-Farsangi
Comparison
of postoperative bleeding in patients undergoing
coronary artery bypass surgery in two groups
taking aspirin and aspirin plus CLS clopidogrel
DOI: 10.5742/MEWFM.2017.93050
[pdf
version]
Ali Pooria, Hassan Teimouri, Mostafa Cheraghi,
Babak Baharvand Ahmadi, Mehrdad Namdari, Reza
Alipoor
Comparison
of lower uterine segment thickness among nulliparous
pregnant women without uterine scar and pregnant
women with previous cesarean section: ultrasound
study
DOI: 10.5742/MEWFM.2017.93051
[pdf version]
Taravat Fakheri, Irandokht Alimohammadi, Nazanin
Farshchian, Maryam Hematti,
Anisodowleh Nankali, Farahnaz Keshavarzi, Soheil
Saeidiborojeni
Effect
of Environmental and Behavioral Interventions
on Physiological and Behavioral Responses of
Premature Neonates Candidates Admitted for Intravenous
Catheter Insertion in Neonatal Intensive Care
Units
DOI: 10.5742/MEWFM.2017.93052
[pdf
version]
Shohreh Taheri, Maryam Marofi, Anahita Masoumpoor,
Malihe Nasiri
Effect
of 8 weeks Rhythmic aerobic exercise on serum
Resistin and body mass index of overweight and
obese women
DOI: 10.5742/MEWFM.2017.93053
[pdf
version]
Khadijeh Molaei, Ahmad Shahdadi, Reza Delavar
Study
of changes in leptin and body mass composition
with overweight and obesity following 8 weeks
of Aerobic exercise
DOI: 10.5742/MEWFM.2017.93054
[pdf
version]
Khadijeh Molaei, Abbas Salehikia
A reassessment
of factor structure of the Short Form Health
Survey (SF-36): A comparative approach
DOI: 10.5742/MEWFM.2017.93088
[pdf version]
Vida Alizad, Manouchehr Azkhosh, Ali Asgari,
Karyn Gonano
Population and Community Studies
Evaluation
of seizures in pregnant women in Kerman - Iran
DOI: 10.5742/MEWFM.2017.93056
[pdf
version]
Hossein Ali Ebrahimi, Elahe Arabpour, Kaveh
Shafeie, Narges Khanjani
Studying
the relation of quality work life with socio-economic
status and general health among the employees
of Tehran University of Medical Sciences (TUMS)
in 2015
DOI: 10.5742/MEWFM.2017.93057
[pdf version]
Hossein Dargahi, Samereh Yaghobian, Seyedeh
Hoda Mousavi, Majid Shekari Darbandi, Soheil
Mokhtari, Mohsen Mohammadi, Seyede Fateme Hosseini
Factors
that encourage early marriage and motherhood
from the perspective of Iranian adolescent mothers:
a qualitative study
DOI: 10.5742/MEWFM.2017.93058
[pdf
version]
Maasoumeh Mangeli, Masoud Rayyani, Mohammad
Ali Cheraghi, Batool Tirgari
The
Effectiveness of Cognitive-Existential Group
Therapy on Reducing Existential Anxiety in the
Elderly
DOI: 10.5742/MEWFM.2017.93059
[pdf
version]
Somayeh Barekati, Bahman Bahmani, Maede Naghiyaaee,
Mahgam Afrasiabi, Roya Marsa
Post-mortem
Distribution of Morphine in Cadavers Body Fluids
DOI: 10.5742/MEWFM.2017.93060
[pdf
version]
Ramin Elmi, Mitra Akbari, Jaber Gharehdaghi,
Ardeshir Sheikhazadi, Saeed Padidar, Shirin
Elmi
Application
of Social Networks to Support Students' Language
Learning Skills in Blended Approach
DOI: 10.5742/MEWFM.2017.93061
[pdf
version]
Fatemeh Jafarkhani, Zahra Jamebozorg, Maryam
Brahman
The
Relationship between Chronic Pain and Obesity:
The Mediating Role of Anxiety
DOI: 10.5742/MEWFM.2017.93062
[pdf
version]
Leila Shateri, Hamid Shamsipour, Zahra Hoshyari,
Elnaz Mousavi, Leila Saleck, Faezeh Ojagh
Implementation
status of moral codes among nurses
DOI: 10.5742/MEWFM.2017.93063
[pdf
version]
Maryam Ban, Hojat Zareh Houshyari Khah, Marzieh
Ghassemi, Sajedeh Mousaviasl, Mohammad Khavasi,
Narjes Asadi, Mohammad Amin Harizavi, Saeedeh
Elhami
The comparison
of quality of life, self-efficacy and resiliency
in infertile and fertile women
DOI: 10.5742/MEWFM.2017.93064
[pdf version]
Mahya Shamsi Sani, Mohammadreza Tamannaeifar
Brain MRI Findings in Children (2-4 years old)
with Autism
DOI: 10.5742/MEWFM.2017.93055
[pdf
version]
Mohammad Hasan Mohammadi, Farah Ashraf Zadeh,
Javad Akhondian, Maryam Hojjati,
Mehdi Momennezhad
Reviews
TECTA gene function and hearing: a review
DOI: 10.5742/MEWFM.2017.93065
[pdf version]
Morteza Hashemzadeh-Chaleshtori, Fahimeh Moradi,
Raziyeh Karami-Eshkaftaki,
Samira Asgharzade
Mandibular
canal & its incisive branch: A CBCT study
DOI: 10.5742/MEWFM.2017.93066
[pdf
version]
Sina Haghanifar, Ehsan Moudi, Ali Bijani, Somayyehsadat
Lavasani, Ahmadreza Lameh
The
role of Astronomy education in daily life
DOI: 10.5742/MEWFM.2017.93067
[pdf
version]
Ashrafoalsadat Shekarbaghani
Human brain
functional connectivity in resting-state fMRI
data across the range of weeks
DOI: 10.5742/MEWFM.2017.93068
[pdf version]
Nasrin Borumandnia, Hamid Alavi Majd, Farid
Zayeri, Ahmad Reza Baghestani,
Mohammad Tabatabaee, Fariborz Faegh
International Health Affairs
A
brief review of the components of national strategies
for suicide prevention suggested by the World
Health Organization
DOI: 10.5742/MEWFM.2017.93069
[pdf
version]
Mohsen Rezaeian
Education and Training
Evaluating
the Process of Recruiting Faculty Members in
Universities and Higher Education and Research
Institutes Affiliated to Ministry of Health
and Medical Education in Iran
DOI: 10.5742/MEWFM.2017.93070
[pdf
version]
Abdolreza Gilavand
Comparison
of spiritual well-being and social health among
the students attending group and individual
religious rites
DOI: 10.5742/MEWFM.2017.93071
[pdf
version]
Masoud Nikfarjam, Saeid Heidari-Soureshjani,
Abolfazl Khoshdel, Parisa Asmand, Forouzan Ganji
A
Comparative Study of Motivation for Major Choices
between Nursing and Midwifery Students at Bushehr
University of Medical Sciences
DOI: 10.5742/MEWFM.2017.93072
[pdf
version]
Farzaneh Norouzi, Shahnaz Pouladi, Razieh Bagherzadeh
Clinical Research and Methods
Barriers
to the management of ventilator-associated pneumonia:
A qualitative study of critical care nurses'
experiences
DOI: 10.5742/MEWFM.2017.93073
[pdf version]
Fereshteh Rashnou, Tahereh Toulabi, Shirin Hasanvand,
Mohammad Javad Tarrahi
Clinical
Risk Index for Neonates II score for the prediction
of mortality risk in premature neonates with
very low birth weight
DOI: 10.5742/MEWFM.2017.93074
[pdf
version]
Azadeh Jafrasteh, Parastoo Baharvand, Fatemeh
Karami
Effect
of pre-colporrhaphic physiotherapy on the outcomes
of women with pelvic organ prolapse
DOI: 10.5742/MEWFM.2017.93075
[pdf
version]
Mahnaz Yavangi, Tahereh Mahmoodvand, Saeid Heidari-Soureshjani
The
effect of Hypertonic Dextrose injection on the
control of pains associated with knee osteoarthritis
DOI: 10.5742/MEWFM.2017.93076
[pdf
version]
Mahshid Ghasemi, Faranak Behnaz, Mohammadreza
Minator Sajjadi, Reza Zandi,
Masoud Hashemi
Evaluation
of Psycho-Social Factors Influential on Emotional
Divorce among Attendants to Social Emergency
Services
DOI: 10.5742/MEWFM.2017.93077
[pdf
version]
Farangis Soltanian
Models and Systems of Health Care
Organizational
Justice and Trust Perceptions: A Comparison
of Nurses in public and private hospitals
DOI: 10.5742/MEWFM.2017.93078
[pdf
version]
Mahboobeh Rajabi, Zahra Esmaeli Abdar, Leila
Agoush
Case series and Case reports
Evaluation
of Blood Levels of Leptin Hormone Before and
After the Treatment with Metformin
DOI: 10.5742/MEWFM.2017.93079
[pdf
version]
Elham Jafarpour
Etiology,
Epidemiologic Characteristics and Clinical Pattern
of Children with Febrile Convulsion Admitted
to Hospitals of Germi and Parsabad towns in
2016
DOI: 10.5742/MEWFM.2017.93080
[pdf
version]
Mehri SeyedJavadi, Roghayeh Naseri, Shohreh
Moshfeghi, Irandokht Allahyari, Vahid Izadi,
Raheleh Mohammadi,
Faculty development
The
comparison of the effect of two different teaching
methods of role-playing and video feedback on
learning Cardiopulmonary Resuscitation (CPR)
DOI: 10.5742/MEWFM.2017.93081
[pdf
version]
Yasamin Hacham Bachari, Leila Fahkarzadeh, Abdol
Ali Shariati
Office based family medicine
Effectiveness
of Group Counseling With Acceptance and Commitment
Therapy Approach on Couples' Marital Adjustment
DOI: 10.5742/MEWFM.2017.93082
[pdf
version]
Arash Ziapour, Fatmeh Mahmoodi, Fatemeh Dehghan,
Seyed Mehdi Hoseini Mehdi Abadi,
Edris Azami, Mohsen Rezaei
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| October 2017 -
Volume 15, Issue 8 |
|
|
Effect of Environmental
and Behavioral Interventions on Physiological
and Behavioral Responses of Premature Neonate
Candidates Admitted for Intravenous Catheter
Insertion in Neonatal Intensive Care Units
Shohreh Taheri (1)
Anahita Masoumpoor (2)
Maryam Marofi (3)
Malihe Nasiri (4)
(1) Master of Science
in Neonatal Intensive Care Nursing, International
Division of Shahid Beheshti University of Medical
Sciences, Tehran, Iran.
(2) Phd in Nursing, Pediatric department, Nursing
and Midwifery School of Shahid Beheshti University
of medical sciences, Tehran, Iran.
(3) Department of Pediatric Nursing, Nursing
and Midwifery Care Research Center, School of
Nursing and Midwifery, Esfahan University of
Medical Sciences, Hezarjrb Ave, Esfahan, Iran.
(4) Phd in biostatistics, Assistant professor
, Nursing and Midwifery School of Shahid Beheshti
University of medical sciences, Tehran, Iran
Correspondence:
Anahita Masoumpoor
Phd in Nursing,
Pediatric department,
Nursing and Midwifery School of Shahid Beheshti
University of Medical Sciences, Tehran, Iran,
|
Abstract
Background and Objective: Many
painful procedures including intravenous
catheterization are performed in the ward
without taking necessary pain-reducing
measures. The present study was conducted
with the aim to determine the effect of
environmental and behavioral interventions
on physiological and behavioral responses
of preterm infants during intravenous
catheterization.
Materials and
Methods: In the present clinical trial,
82 infants with gestational age of 30-37
weeks were randomly divided into intervention
and control groups. In the preliminary
intervention stage, measures such as dimming
light and noise, using eye patch and ear
plugs, reducing nursing manipulations,
and positioning the newborn in fetal position
30 minutes before and 30 minutes after
venepuncture were performed for the intervention
group, but the control group received
only the routine care. Data were collected
using NIPS & EDIN Scale, and analyzed
in SPSS-20.
Results: No
significant difference was observed between
the two groups in behavioral responses
to pain and stress prior to intravenous
catheterization (P>0.05) (P=0.13),
but these responses were significantly
less in the intervention group compared
to the control during and after this procedure
(P<0.05). Moreover, no significant
difference was observed between the two
groups in the mean physiological responses
(P>0.05).
Conclusion:
Dimming light and noise, reducing nursing
manipulations, and fetal positioning during
intravenous catheterization effectively
reduces neonatal pain.
Key words:
Environmental and behavioral interventions,
physiological and behavioral responses,
intravenous catheterization,
preterm infant.
|
The neonatal period includes the first moment
of delivery to one month after birth. At this
time, physical changes occur in the body and
the infant learns how to respond to many forms
of external stimuli (1). Over the past 25 years,
the prevalence of premature babies has increased
by 30 percent (2). More than 70% of preterm
infants admitted to a special care nursery have
spent time in a NICU (3). Many years ago, it
was thought that babies and infants do not feel
pain because of an immature nervous system or
they feel less pain than adults. At present,
it has been shown that the fiber nerves directing
the pain stimulations are formed during embryonic
development and in fact, term infants have the
same sensitivity to pain as older infants and
children do, and premature infants may be more
sensitive to pain than full term infants (4).
Pain as one of the defensive mechanisms of the
body, indicates abnormal conditions in the body,
so that relief from the pain is a basic requirement
and the right of all people as well as the most
important goals of medical science (5). The
results of a study on neonates in the neonatal
intensive care unit indicated that heel prick
blood sampling was the most common procedure
(56%), followed by endotracheal suction (26%)
and intravenous cannula insertion (8%), and
other procedures with fewer percentages included
venepuncture, intubation, intramuscular injection,
intravenous catheter insertion, peripheral artery
catheter placement, infusion catheter, bladder
urine sampling, cerebrospinal fluid sampling,
and arterial sampling (6). Inadequately managed
pain, for whatever reason, leads to long-term
physiological, psychosocial and behavioral consequences,
and through being aware of stressors that affect
the ill child and their family as well as by
designing and applying safe and effective interventions
to eliminate or reduce stressors, caregivers
should focus their attention on non-traumatic
care (7). Stress and pain in newborns can lead
to many complications such as such as increased
hypoxia, elevated cortisol level (8), impaired
nervous system development (9) and mental disorders
and increased length of hospitalization (10).
The infants’ responses to pain and stress
can be represented in three behavioral, physiological
and nervous-chemical ways; however, the intensity
and mode of occurrence of these responses depends
upon factors such as maternal gestational age,
severity of illness, and duration of admission
to the neonatal intensive care unit. Behavioral
responses to pain and stress in newborns include
the following: crying, body movements, facial
shrinkage, and decreased or impaired nutrition.
Physiological responses to pain and stress in
newborns include changes in blood pressure and
heart rate, hypoxia, and increased oxygen intake
(11). A high percentage of premature infants
may experience problems that result in more
than 20 days of stay in infants’ care units
(12). Since infants are unable to meet their
needs by oral feeding, one of their basic care
needs is to provide care by administering fluids,
medicines and nutrition, and for this purpose,
intravenous access is essential (13). Angiocath
is considered to be the first choice in the
newborn baby, which is ideally suited for short-term
treatments (14). In this regard, many painful
procedures, including intravenous catheters
placement, can be performed without the necessary
measures to decrease pain (15). On the other
hand, frequent intermittent catheterization
puts the infant at risk of painful experiences,
stress and the risk of infection and inability
to control the pain caused by it, causing short
and long-term complications for the baby’s
health (16), including increasing demand on
the cardiovascular system, respiratory system,
immunosuppression, increased intracranial pressure,
which can lead to intravesical hemorrhage, long-term
emotional, behavioral and learning disabilities
(17). Pain in newborns can be controlled by
non-pharmacological methods such as oral sucrose,
non-nutritional sucking, breastfeeding, mother/infant
skin-to-skin contact (kangaroo care), and music
playback during the procedure (18). Furthermore,
according to Stevens 2013, non-drug actions
such as lactation, hugging, touching, massaging,
cold and hot compress, the use of relaxation
techniques, such as playing melodies, music
and attention deviance, can effectively reduce
the infant’s pain (19, 20). Although the
use of non-pharmacological measures in the control
of anxiety is scientifically and culturally
accepted, they have been forgotten due to lack
of scientific advice in the pediatric wards
(21). Nurses as the most important members in
the treatment team, play an important role in
maintaining the health and well-being of patients
(22). Based on the evolutionary model, taking
care of these babies allows the health care
practitioner to identify the behavioral signs
of the baby, such as when the baby needs sleep
or is under stress due to manipulation and intervention
and design a care plan adapted to his/her characteristics
(23). Evolutionary care and support, integrates
the evolutionary needs of newborns admitted
to the intensive care unit for medical care.
Key concepts in evolutionary care include the
organized improvement of neuropsychological
and physiological behaviors, modifying physical
environment such as light, sound and heat to
protect the sensory and vulnerable system, in
a set of family-centered structures (24). Regarding
the long-term hospitalization of premature infants
in the neonatal intensive care unit and painful
procedures such as intravenous catheter insertion
which can cause pain and stress in the newborn,
as well as the importance of evolutionary care
in reducing pain in infants, this study was
aimed to determine the effect of environmental
and behavioral interventions on the physiological
and behavioral responses of premature neonates
during venepuncture procedure.
The present study was a double-blind clinical
trial (intervention and control group). The
research population consisted of all preterm
infants admitted to the neonatal intensive care
unit of Alzahra hospital affiliated to Isfahan
University of Medical Sciences. The babies who
had the criteria for entering the research were
identified. Having completed the consent form
and being signed by parents, the biographical
information form was completed using the medical
records of the infant. Biographical data included
infant’s name, fetal age, birth weight,
infant sex, 1 and 5 minutes Apgar score, type
of delivery, number of venepuncture attempts,
and physiological information form including
heart rate, respiratory rate and SpO2. In order
to measure pain in infants, a NIPS checklist
consisting of 6 options (facial expression,
crying pattern, breathing pattern, arm and leg
movement and irritability type), was used. The
lowest score of pain was zero and the highest
score was 7. A score greater than 3 indicated
pain (25). Validity and reliability of this
tool were confirmed according to Dilli study
(2009) (26) and Khodaie studies (2010) (28)
(r = 98). To measure the neonatal stress and
discomfort, EDIN scale containing 5 items (facial
expression, body movements, sleep status, communication
with the nurse, and relaxation) ranging from
0 to 15 was employed; its validity and reliability
were confirmed by Debillon et al., (2001) (
= 0.92) (28). In order to study the physiological
criteria, Saadat Monitoring manufactured by
Pooyandegan Rayan-Sanat, Tehran, Iran was used
and the equipment was calibrated by medical
equipment engineers prior to use. After confirmation
by the Ethics Committee coded by IR.SBMU.RETECH.REC.1395.587
and obtaining written permission from the authorities,
the researcher visited the Neonatal Intensive
Care Unit of Al-Zahra Hospital in Isfahan to
collect samples and by explaining the aims of
the study for the authorities and staff of the
neonatal intensive care unit, sampling was performed.
According to the sample size formula, 41 neonates
(in each group) were selected for participation
in the study and were randomly assigned (colored
beads) to two, intervention and control, groups.
Then, the environmental and behavioral interventions
including closing the eyes of the newborns with
an eye patch to decrease light, closing the
ears of the newborns with ear plug to reduce
the auditory stimuli and fetal positioning using
the nests provided by the researcher, were implemented
in the ward by the researcher. After 30 minutes
of interventions, an intravenous catheter insertion
was performed by an experienced nurse while
interventions continued. At the same time, another
nurse who had a work experience of at least
one year in the neonatal ward and knowing how
to fill out the measurement tools, completed
the checklist 2 minutes prior to the venepuncture,
during the venepuncture and 5 minutes later
and 30 minutes after the venepuncture while
interventions continued. Physiological data
and related checklist were completed and samples
were taken out after an hour of relevant study.
For each studied neonate, no environmental and
behavioral interventions were performed in the
control group, but all the information gathering
and checklists completing procedures were implemented
and recorded as the first one. Data analysis
was performed using SPSS version 20. In descriptive
statistics, descriptive indicators such as mean
and standard deviation were reported. The repeated
measures analysis of variance was used to compare
the two groups at different times. Also, for
comparing demographic indices in two groups,
independent t-test, Mann-Whitney and Chi-square
test were used.
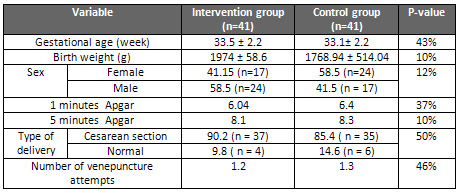
The
results
indicated
that
the
mean
gestational
age
of
infants
was
33.3
±
2.2
weeks
and
the
mean
weight
of
newborns
was
1871.2
±
547.32
g.
There
was
no
statistically
significant
difference
between
the
mean
1
and
5
minutes
Apgar
score
and
the
mean
number
of
venepuncture
in
the
two
groups
[Table
1].
The
fetal
age
of
all
subjects
was
33
weeks.
Table
1:
Frequency
distribution
of
neonatal
demographic
variables
in
both
intervention
and
control
groups
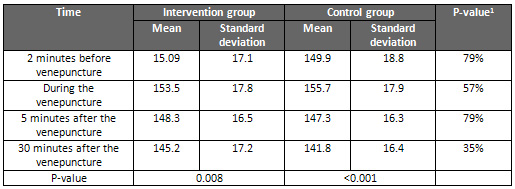
The
mean
heart
rate
in
both
groups
was
initially
found
to
be
increased
during
venepuncture
and
then
decreased
over
time
(P
<0.05),
but
the
results
showed
that
there
is
no
significant
difference
between
the
mean
heart
rate
at
different
times
between
the
two
groups
(P>
0.05)
[Table
2]
Table
2:
Comparison
of
mean
heart
rate
at
different
times
between
the
two
groups
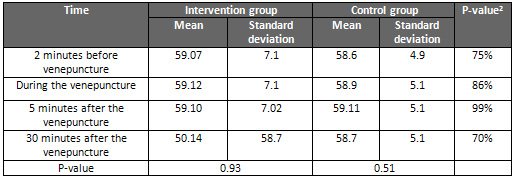
The
mean
of
respiratory
rate
in
the
intervention
group
was
59
and
in
the
control
group
58.
Although
the
mean
respiratory
rate
was
higher
in
the
intervention
group,
the
results
showed
that
there
was
no
statistically
significant
difference
in
the
respiratory
rate
over
time
in
both
groups
(p>
0.05)
[Table
3]
Table
3:
Comparison
of
mean
respiratory
rate
at
different
times
between
the
two
groups
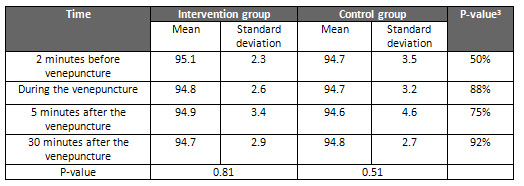
The
mean
of
arterial
oxygen
saturation
in
the
intervention
group
was
94.875
and
94.7
in
the
control
group.
Although
the
mean
of
arterial
oxygen
saturation
in
the
intervention
group
was
higher,
the
results
showed
that
there
was
no
statistically
significant
difference
in
the
mean
arterial
oxygen
saturation
during
venepuncture
in
both
groups
(p>
0.05)
[Table
4].
Table
4:
Comparison
of
mean
SP02
at
different
times
between
the
two
groups
There
was
no
statistically
significant
difference
between
the
mean
pain
intensity
score
in
the
neonates
two
minutes
before
the
venepuncture
and
30
minutes
after
the
venepuncture
between
the
intervention
and
control
groups
(p>
0.05).
However,
the
mean
score
of
pain
in
the
intervention
group
was
significantly
less
than
the
control
group
during
the
venepuncture
and
5
minutes
after
the
venepuncture
(p
<0.05)
[Table
5].
Table
5:
Comparison
of
mean
pain
intensity
at
different
times
between
the
two
groups
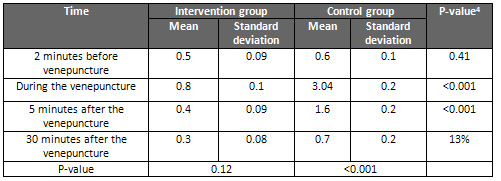
There
was
no
significant
difference
between
the
mean
severity
of
stress
and
discomfort
scores
in
the
neonates
two
minutes
before
the
venepuncture
in
two
intervention
and
control
groups
(p
=
0.13).
However,
the
mean
of
stress
and
discomfort
scores
in
the
intervention
group
was
significantly
less
than
the
control
group
during
and
5
and
30
minutes
after
the
venepuncture
(p
<0.05)
[Table
6].
Table
6:
Comparison
of
mean
stress
score
at
different
times
between
the
two
groups
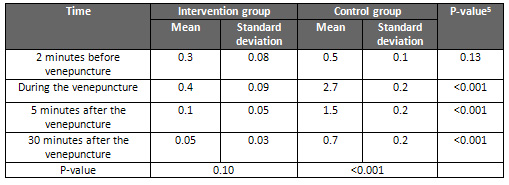
There
are
many
studies
worldwide
about
some
of
the
environmental
interventions
(light
and
noise
reduction),
neonatal
physiological
and
behavioral
responses
(heart
rate,
respiratory
rate
and
arterial
oxygen
saturation)
and
various
pain
assessment
methods,
but
no
research
has
been
found
in
relation
to
the
effect
of
environmental
and
behavioral
interventions
on
the
physiological
and
behavioral
responses
of
premature
infants
candidates
for
intravenous
catheter
insertion
admitted
to
the
neonatal
intensive
care
unit.
The
results
of
this
study
showed
that
although
the
average
heart
rate
in
the
two
groups
was
different
and
was
firstly
increased
during
the
venepuncture
and
was
decreased
over
time,
no
significant
difference
was
found
between
the
mean
heart
rate
at
different
times
between
the
two
groups.
The
mean
respiratory
rate
and
arterial
oxygen
saturation
were
higher
in
the
intervention
group,
but
these
changes
did
not
show
a
statistically
significant
difference
in
any
of
the
two
groups
over
time.
The
results
of
this
study
are
in
line
with
Marilyn’s
study
2013
(29)
in
Canada
as
well
as
the
study
by
Jacques
Sizun
(30)
in
France
in
2002.
The
results
of
this
study
showed
significant
physiological
changes
(mean
SpO2
and
heart
rate)
among
newborns
with
evolutionary
care
before
and
after
weighing
compared
with
the
control
group,
but
the
rate
of
hypoxic
attacks
was
decreased
significantly,
which
was
in
line
with
the
results
of
studies
by
Johnston
et
al.
(31)
and
Taheri
et
al.
(32)
in
2007-2008.
In
terms
of
heart
rate
and
respiratory
rate,
the
results
of
this
study
were
consistent
with
the
study
of
Taheri
et
al.,
but
did
not
have
an
agreement
on
the
amount
of
arterial
oxygen
saturation.
This
discrepancy
can
be
due
to
the
difference
between
the
procedures
conducted
in
the
study.
The
results
of
this
study
are
consistent
with
the
results
of
the
study
by
Slevin
et
al.
(33)
in
2000.
In
addition,
the
results
of
this
study
are
consistent
with
the
results
of
the
research
by
Abdeyazdan
et
al.
(34)
(2013),
for
the
respiratory
rate,
but
are
inconsistent
in
terms
of
oxygenation
rate.
This
discrepancy
in
outcomes
can
be
attributed
to
the
difference
between
the
interventions
in
the
study.
The
results
of
this
study
are
not
consistent
with
the
results
of
the
study
by
Celine
Catelin
and
colleagues
(35)
in
France
in
2005.
Their
study
showed
that
the
implementation
of
environmental
and
behavioral
interventions
such
as
(closing
baby’s
eyes
and
ears,
non-nutritious
diet,
kangaroo
and
family-centered
care,
shaking
the
baby
and
putting
the
baby
in
a
fetal
position)
during
the
weighing
process
resulted
in
significant
changes
in
physiological
criteria;
it
suggests
that
these
interventions
have
led
to
a
decrease
in
respiratory
rate
and
a
decrease
in
heart
rate,
and
an
increase
in
arterial
oxygen
saturation,
which
can
be
due
to
the
low
number
of
samples
in
each
group
(15
neonates
for
each
group).
However
in
the
recent
study,
increasing
the
number
of
neonates
in
each
group
(n
=
41)
as
well
as
different
procedures
in
the
study
could
be
the
reasons
for
discrepancy
in
the
results.
Regarding
the
embryo’s
position,
the
results
of
this
study
are
not
consistent
with
the
results
of
the
study
by
Reyhani
et
al.
(2011)
in
Mashhad
(36).
This
discrepancy
can
be
attributed
to
individual
differences,
demographic
characteristics
of
infants,
providing
different
nursing
care
in
infants’
intensive
care
units
and
different
fetal
age.
Moreover,
the
results
of
this
study
are
not
consistent
with
the
results
of
the
study
by
Nasimi
et
al.
(2014)
in
Mashhad
(37).
This
discrepancy
can
be
due
to
the
different
procedures
conducted
in
the
study;
these
studies
have
been
done
using
an
invasive
procedure
during
a
venepuncture,
while
the
study
by
Nasimi
et
al.,
has
been
conducted
with
normal
procedures
in
the
ward.
Other
results
obtained
from
this
study
also
showed
that
there
was
no
significant
difference
between
the
mean
score
of
pain
in
newborns
2
minutes
before
venepuncture
and
30
minutes
after
venepuncture
between
the
intervention
and
control
groups
(p
>0.05);
but
the
mean
score
of
pain
in
the
intervention
group
was
significantly
less
than
that
of
the
control
group
during
and
5
minutes
after
the
venepuncture
(p
<0.05).
Additionally,
there
was
no
significant
difference
between
the
mean
stress
intensity
and
discomfort
in
the
neonates
2
minutes
before
the
venepuncture
between
the
intervention
and
control
groups
(p
=
0.13),
but
the
mean
score
of
stress
and
discomfort
in
the
intervention
group
was
significantly
less
than
that
of
the
control
group
during
as
well
as
5
and
30
minutes
after
the
venepuncture.
The
results
of
this
study
were
in
line
with
the
results
of
the
study
by
Celine
Kathleen
et
al.
(2005).
Also,
the
results
of
this
study
are
consistent
with
the
results
of
the
study
of
Reyhani
et
al.
(2011)
implying
that
the
fetal
position
decreased
the
pain
intensity
of
newborns
in
the
intervention
group
compared
to
the
control
group.
According
to
the
results,
we
can
conclude
that
there
are
no
environmental
and
behavioral
interventions
that
affect
the
physiological
and
behavioral
responses
of
the
premature
infant,
so
further
research
is
recommended.
Given
the
advantages
of
reducing
pain
and
stress
during
the
intravenous
catheters
insertion
in
premature
infants,
their
low
cost,
the
lack
of
specific
equipment
and
the
need
for
evolutionary
care,
it
is
recommended
to
use
these
interventions
in
order
to
decrease
the
pain
of
premature
neonates
during
painful
procedures
including
venpuncture.
Acknowledgement
The
authors
in
this
study
would
like
to
express
their
gratitude
to
the
staff
of
the
infant’s
intensive
care
unit
at
Al-Zahra
Hospital
in
Esfahan,
who
helped
us
carry
out
this
research.
This
article
is
based
on
the
results
of
a
Master
thesis
of
Nursing
Special
Babies,
International
Branch
of
Shahid
Beheshti
University
of
Medical
Sciences.
1-
Behrman
RE
,
Jenson
HB
,
Kligma
MR
,
Stanton
Bf
,
2007.
Nelson
Text
Book
Of
Pediatrics,
18th,
p:
23-29.
2-
Tramo
M
,
Koh
C
,
Lense
M
,
Ness
C
,
Krishnamoorthy
K
,
Kagan
J
,
et
al.
Effect
of
auditory
stimulation
with
vocal
music
on
neurophysiological
responses
to
acute
pain
in
premature
infants.
The
Institute
for
Music
&
Brain
Science.
2006.
Available
from:
www.BrainMusic.org.
Accessed
2009
.
3-
Kellam
B
&
Bhatia
J.
2008,”Sound
spectral
analysis
in
the
intensive
care
nursery:
measuring
high-
frequency
sound”,
Journal
of
Pediatric
Nursing,
Vol.23,
No.
4,
p.317-328.
4-
Sheikh
Baha’addin
Zadeh
A
,
Dr.
Rai
V.
NICU
Nursing,
Neonatal
Care
Unit,
Boshra
Publishing
(Medical
Science
Publication
Center),
Collaborating
with
Publishing
House,
2011,
pp:
69-46.(Persian)
5-
Motahedian.A.
Movahedi
Rad.
S.
Hagizadeh.
A,
Lake.
M.
Evaluation
Effect
of
music
therapy
on
postoperative
pain
in
patients
undergoing
spinal
surgery,
Journal
of
Nursing
Care
,
5
(
3
)
:
144-139.(Persian)
6-
Whipple
J
2008.The
effect
of
music-reinforced
nonnutritive
sucking
on
state
of
preterm,
low
birthweight
infants
experiencing
heelstick.
Charleston
Southern
University
Fall;
45(3):227-72.
7-
Hockenberry,
Marilyn
J
and
Wilson,
D
2011,
Wong,
essentials
of
pediatric
nursing,
8th
edn.
8-
J
Sizun,
B
Westrup,
and
the
ESF
Network
Coordination
Committee.
Early
developmental
care
for
preterm
neonates.
Arch
Dis
Child
Fetal
Neonatal
Ed
2004;
89:F384–F389.
9-
Ruthe.
Grunau,
David
W.
Haley,
Michael
F.
Whitfield,
Joanne
Weinberg,
Wayne
Yu,
and
Paul
Thiessen.
Altered
Basal
Cortisol
Levels
at
3,
6,
8
and
18
Months
in
Infants
Born
at
Extremely
Low
Gestational
Age.
J
Pediatr
2007;
150:151-6.
10-
Marofi
M,
Nikobakht
F,
Badiee
Z,
Golchin
M.
The
effect
of
melody
on
the
physiological
responses
of
heel
sticks
pain
in
neonates.
Iranian
Journal
of
Nursing
and
Midwifery
Research
|
May-June
2015
|
Vol.
20
|
Issue
3.(Persian)
11-
Rohrmeister
K,
Kretzer
V,
Berger
A,
Haiden
N,
Kohlhauser
C,
Pollak
A.
Pain
and
stress
management
in
the
Neonatal
Intensive
Care
Unit
--a
national
survey
in
Austria.
Wiener
Klinische
Wochenschrift.
2003
;
115(19):715-9.
13-
Sharp,
EL
2006,”Developing
a
nurse-directed
peripherally
inserted
central
catheter
team
in
the
neonatal
intensive
care
unit”,
Newborn
and
Infant
Nursing
Reviews,
Vol.
6,
NO.
4,
PP.225-229.
14-
Sundquist
Beauman,
S
&
Swanson,
A
2006.
“Neonatal
infusion
therapy:
preventing
Complications
and
improving
outcomes”,
Newborn
and
Infant
Nursing
Reviews,
Vol.
6,
NO.
4,
PP.
193-201.
15-
Verklan
&
Walden,
M
Terese
2010.
Pain
Assessment
and
Management:
Core
curriculum
for
neonatal
intensive
care
nursing
,
4
thed.PP.333.
16-
Dalal,
ss,
chawla,
D,
Singh
,
J,
Agarwal,
RK,
Deorari,
AK
&
Paul,
VK
2009.
“Limb
splinting
for
intravenous
cannulae
in
neonates
:
a
randomized
controlled
trial”,
Archives
of
Disease
Childhood.
Fetal.
Neonatal
EditioN,
Vol.
94,
pp.394-396.
17-
Byrd,
PJ,
Gonzales,
I
&
Parsons,
V
2009,”Exploring
barriers
to
pain
management
in
newborn
intensive
care
units,
a
pilot
survey
of
NICU
nurses,”
Advances
in
Neonatal
Care,
Vol.
9
,
NO.
6,
PP.
299-306.
18-
Campbell-Yeo
ML,
Johnston
CC,
Joseph
K,
Feeley
NL,
Chambers
CT,
Barrington
KJ
2009;
Co-bedding
as
a
Comfort
measure
For
Twins
undergoing
painful
procedures
(CComForT
Trial).
Vol
9,
pp.76.
20-
Stevens
B,
Yamada
J,
Lee
GY,
Ohlsson
A2013.
Sucrose
for
analgesia
in
newborn
infants
undergoing
painful
procedures.
Vol
1,
PP:
1069.
21-
Modiri
M
,
Dr.
Zargham
A
,
Marofi
M.
Familiarity
with
“The
Impact
of
Nursing
Contravention
Team
on
the
Anxiety
Severity
of
Children
Admitted
to
the
Pediatric
Department
of
Dezful
Hospital
in
2014”.
Master’s
thesis,
Isfahan
University
of
Medical
Sciences.(Persian)
22-
Potter
PA,
Perry
AG.
Fundamentals
of
nursing.2013.
6thed.
St.
Louis:
Elsevier
Health
Sciences,
p.315.
23-
Mouls
T,
Ramsay
J
2008,
Children’s
and
young
people’s
nursing,
2dn
ed,
Blackwell.UK.
24-
Early
care
guidelines
for
neonatal
intensive
care
units,
Future
changes
in
infants
admitted
to
intensive
care
units,
Neonatal
Health
Department,
Spring2014.
25-Taddio,
A,
Appleton,
M,
Bortolussi,
R,
Chambers,
C
&
Dubey,
V
2010.
Reducing
the
pain
of
child
hood
vaccination
,
Journal
of
Canadian
Medical
,
Vol
.
18,
pp.
1-7.
26-
Dilli
D,
Kukuk
IG,
Dallar
Y.2009.
Interventions
to
reduce
pain
during
vaccination
in
infancy,
Journal
of
Pediatrics,
Vol.
154,
pp.385-390.
27-
Khodaee.F.Boroomandfar.
KH.Abdeyazdan.
Z.
Marofi.
M.
2010.
“A
comparative
study
of
the
pain
caused
by
vaccination
in
cold
water
spraying
and
mother
feeding
during
infusion
in
infants
who
referred
to
Ibne
Sina
Health
Center
in
Isfahan.”
Master’s
thesis,
Isfahan
University
of
Medical
Sciences.(Persian)
28-
Debillon
T,
Zupan
V,
Ravault
N,
Magny
JF,
Dehan
M:
Development
and
initial
validation
of
the
EDIN
scale.
Arch
Dis
Child
Fetal
Neonatal
Ed
85:F36-41,
2001.
29-
Marilyn
A,
Celeste
J,
Céline
Goulet.
Tim
F.
Oberlander,
FRCPC3,
and
Laurie
Snider.
Intervention
Minimizing
Preterm
Infants’
Exposure
to
NICU
Light
and
Noise.
Clin
Nurs
Res
2013
22:
337
originally
published
online
28
December
2012.
30-
Jacques
Sizun.Clinical,
Physiologic,
and
Biologic
Impact
of
Environmental
and
Behavioral
Interventions
in
Neonates
During
a
Routine
Nursing
Procedure.
The
Journal
of
Pain,
Vol
6,
No
12
(December),
2005:
pp
791-797.
31-
Johnston
C
C,
Stevens
B,
Givvins
S,
Frank
LS
.Treatment
of
Pain
in
NICU.
Pediater
Clin
North
Am
2000
479(3):
633-650.
32-
Abbasi.
A.
Taheri.
P.
Dr.
Abdeyazdan.
Z.
Fathi
Zadeh.
N.
Investigating
the
Effectiveness
of
the
Program
Designed
on
the
Physiological
and
Motor
Responses
of
Premature
Infants
Admitted
to
the
Alzahra
Neonatal
Intensive
Care
Unit.
Master’s
thesis,
Isfahan
University
of
Medical
Science.(Persian)
33-
Slevin
M,
Farrington
N,
Duffy
G,
Daly
L
and
Murphy
JFA.
Altering
the
NICU
and
Measuring
Infants’
Responses.
Acta
Pediatr.
2000;
8(9):577-81.
34-
Abdeyazdan.Z.
Taheri.P.
Abbasi.E.
Fathizadeh.N.
Effects
of
a
quietness
program
in
NICU
on
body
movements,
oxygenation,
and
respiratory
rate
in
preterm
infants.
New
Care,
Journal
of
Nursing
and
Midwifery,
Birjand
University
of
Medical
Sciences,
Vol
10,
Issue
4,
2013.(Persian)
35-
Céline
Catelin,
Sylvie
Tordjman,
Vincent
Morin,
Emmanuel
Oger,
and
Jacques
Sizun.
Clinical,
Physiologic,
and
Biologic
Impact
of
Environmental
and
Behavioral
Interventions
in
Neonates
During
a
Routine
Nursing
Procedure.
The
Journal
of
Pain,
Vol
6,
No
12
(December),
2005:
pp
791-797.
36-
Reyhani
T.
Mohebbi
T.
Boskabadi
H.
Gholami
H.
Ghavami
Ghanbarabadi
V.
The
Effect
of
Facilitated
Tucking
During
Venipuncture
on
Pain
and
Physiological
Parameters
in
Preterm
Infants,
Quarterly
Journal
of
Evidence-Based
Care
/
Vol
2,
Issue
2,
2013.(Persian)
37-
Nasimi.
F.
Behnam
Vashani.
H
.
Boskabadi.
H.
Ketabi.
D.
Study
the
Effect
of
Quiet
Time
Protocol
on
Physiological
Characteristics
of
Preterm
Infants.
Quarterly
Journal
of
Evidence-Based
Care,
Vol.
5,
No.
14,
Spring
94.(Persian)
|
|
.................................................................................................................

|
| |
|

