|
|
 |
| ............................................................. |
|
October 2017 -
Volume 15, Issue 8
|
 |
|
View
this issue in pdf formnat - the issue
has been split into two files for downloading
due to its large size: FULLpdf
(12 MB)
Part
1 &
Part
2
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
........................................................
|
|
Original Contribution/Clinical Investigation
Immunity
level to diphtheria in beta thalassemia patients
DOI: 10.5742/MEWFM.2017.93048
[pdf
version]
Abdolreza Sotoodeh Jahromi, Karamatollah Rahmanian,
Abdolali Sapidkar, Hassan Zabetian, Alireza
Yusefi, Farshid Kafilzadeh, Mohammad Kargar,
Marzieh Jamalidoust,
Abdolhossein Madani
Genetic
Variants of Toll Like Receptor-4 in Patients
with Premature Coronary Artery Disease, South
of Iran
DOI: 10.5742/MEWFM.2017.93049
[pdf
version]
Saeideh Erfanian, Mohammad Shojaei, Fatemeh
Mehdizadeh, Abdolreza Sotoodeh Jahromi, Abdolhossein
Madani, Mohammad Hojjat-Farsangi
Comparison
of postoperative bleeding in patients undergoing
coronary artery bypass surgery in two groups
taking aspirin and aspirin plus CLS clopidogrel
DOI: 10.5742/MEWFM.2017.93050
[pdf
version]
Ali Pooria, Hassan Teimouri, Mostafa Cheraghi,
Babak Baharvand Ahmadi, Mehrdad Namdari, Reza
Alipoor
Comparison
of lower uterine segment thickness among nulliparous
pregnant women without uterine scar and pregnant
women with previous cesarean section: ultrasound
study
DOI: 10.5742/MEWFM.2017.93051
[pdf version]
Taravat Fakheri, Irandokht Alimohammadi, Nazanin
Farshchian, Maryam Hematti,
Anisodowleh Nankali, Farahnaz Keshavarzi, Soheil
Saeidiborojeni
Effect
of Environmental and Behavioral Interventions
on Physiological and Behavioral Responses of
Premature Neonates Candidates Admitted for Intravenous
Catheter Insertion in Neonatal Intensive Care
Units
DOI: 10.5742/MEWFM.2017.93052
[pdf
version]
Shohreh Taheri, Maryam Marofi, Anahita Masoumpoor,
Malihe Nasiri
Effect
of 8 weeks Rhythmic aerobic exercise on serum
Resistin and body mass index of overweight and
obese women
DOI: 10.5742/MEWFM.2017.93053
[pdf
version]
Khadijeh Molaei, Ahmad Shahdadi, Reza Delavar
Study
of changes in leptin and body mass composition
with overweight and obesity following 8 weeks
of Aerobic exercise
DOI: 10.5742/MEWFM.2017.93054
[pdf
version]
Khadijeh Molaei, Abbas Salehikia
A reassessment
of factor structure of the Short Form Health
Survey (SF-36): A comparative approach
DOI: 10.5742/MEWFM.2017.93088
[pdf version]
Vida Alizad, Manouchehr Azkhosh, Ali Asgari,
Karyn Gonano
Population and Community Studies
Evaluation
of seizures in pregnant women in Kerman - Iran
DOI: 10.5742/MEWFM.2017.93056
[pdf
version]
Hossein Ali Ebrahimi, Elahe Arabpour, Kaveh
Shafeie, Narges Khanjani
Studying
the relation of quality work life with socio-economic
status and general health among the employees
of Tehran University of Medical Sciences (TUMS)
in 2015
DOI: 10.5742/MEWFM.2017.93057
[pdf version]
Hossein Dargahi, Samereh Yaghobian, Seyedeh
Hoda Mousavi, Majid Shekari Darbandi, Soheil
Mokhtari, Mohsen Mohammadi, Seyede Fateme Hosseini
Factors
that encourage early marriage and motherhood
from the perspective of Iranian adolescent mothers:
a qualitative study
DOI: 10.5742/MEWFM.2017.93058
[pdf
version]
Maasoumeh Mangeli, Masoud Rayyani, Mohammad
Ali Cheraghi, Batool Tirgari
The
Effectiveness of Cognitive-Existential Group
Therapy on Reducing Existential Anxiety in the
Elderly
DOI: 10.5742/MEWFM.2017.93059
[pdf
version]
Somayeh Barekati, Bahman Bahmani, Maede Naghiyaaee,
Mahgam Afrasiabi, Roya Marsa
Post-mortem
Distribution of Morphine in Cadavers Body Fluids
DOI: 10.5742/MEWFM.2017.93060
[pdf
version]
Ramin Elmi, Mitra Akbari, Jaber Gharehdaghi,
Ardeshir Sheikhazadi, Saeed Padidar, Shirin
Elmi
Application
of Social Networks to Support Students' Language
Learning Skills in Blended Approach
DOI: 10.5742/MEWFM.2017.93061
[pdf
version]
Fatemeh Jafarkhani, Zahra Jamebozorg, Maryam
Brahman
The
Relationship between Chronic Pain and Obesity:
The Mediating Role of Anxiety
DOI: 10.5742/MEWFM.2017.93062
[pdf
version]
Leila Shateri, Hamid Shamsipour, Zahra Hoshyari,
Elnaz Mousavi, Leila Saleck, Faezeh Ojagh
Implementation
status of moral codes among nurses
DOI: 10.5742/MEWFM.2017.93063
[pdf
version]
Maryam Ban, Hojat Zareh Houshyari Khah, Marzieh
Ghassemi, Sajedeh Mousaviasl, Mohammad Khavasi,
Narjes Asadi, Mohammad Amin Harizavi, Saeedeh
Elhami
The comparison
of quality of life, self-efficacy and resiliency
in infertile and fertile women
DOI: 10.5742/MEWFM.2017.93064
[pdf version]
Mahya Shamsi Sani, Mohammadreza Tamannaeifar
Brain MRI Findings in Children (2-4 years old)
with Autism
DOI: 10.5742/MEWFM.2017.93055
[pdf
version]
Mohammad Hasan Mohammadi, Farah Ashraf Zadeh,
Javad Akhondian, Maryam Hojjati,
Mehdi Momennezhad
Reviews
TECTA gene function and hearing: a review
DOI: 10.5742/MEWFM.2017.93065
[pdf version]
Morteza Hashemzadeh-Chaleshtori, Fahimeh Moradi,
Raziyeh Karami-Eshkaftaki,
Samira Asgharzade
Mandibular
canal & its incisive branch: A CBCT study
DOI: 10.5742/MEWFM.2017.93066
[pdf
version]
Sina Haghanifar, Ehsan Moudi, Ali Bijani, Somayyehsadat
Lavasani, Ahmadreza Lameh
The
role of Astronomy education in daily life
DOI: 10.5742/MEWFM.2017.93067
[pdf
version]
Ashrafoalsadat Shekarbaghani
Human brain
functional connectivity in resting-state fMRI
data across the range of weeks
DOI: 10.5742/MEWFM.2017.93068
[pdf version]
Nasrin Borumandnia, Hamid Alavi Majd, Farid
Zayeri, Ahmad Reza Baghestani,
Mohammad Tabatabaee, Fariborz Faegh
International Health Affairs
A
brief review of the components of national strategies
for suicide prevention suggested by the World
Health Organization
DOI: 10.5742/MEWFM.2017.93069
[pdf
version]
Mohsen Rezaeian
Education and Training
Evaluating
the Process of Recruiting Faculty Members in
Universities and Higher Education and Research
Institutes Affiliated to Ministry of Health
and Medical Education in Iran
DOI: 10.5742/MEWFM.2017.93070
[pdf
version]
Abdolreza Gilavand
Comparison
of spiritual well-being and social health among
the students attending group and individual
religious rites
DOI: 10.5742/MEWFM.2017.93071
[pdf
version]
Masoud Nikfarjam, Saeid Heidari-Soureshjani,
Abolfazl Khoshdel, Parisa Asmand, Forouzan Ganji
A
Comparative Study of Motivation for Major Choices
between Nursing and Midwifery Students at Bushehr
University of Medical Sciences
DOI: 10.5742/MEWFM.2017.93072
[pdf
version]
Farzaneh Norouzi, Shahnaz Pouladi, Razieh Bagherzadeh
Clinical Research and Methods
Barriers
to the management of ventilator-associated pneumonia:
A qualitative study of critical care nurses'
experiences
DOI: 10.5742/MEWFM.2017.93073
[pdf version]
Fereshteh Rashnou, Tahereh Toulabi, Shirin Hasanvand,
Mohammad Javad Tarrahi
Clinical
Risk Index for Neonates II score for the prediction
of mortality risk in premature neonates with
very low birth weight
DOI: 10.5742/MEWFM.2017.93074
[pdf
version]
Azadeh Jafrasteh, Parastoo Baharvand, Fatemeh
Karami
Effect
of pre-colporrhaphic physiotherapy on the outcomes
of women with pelvic organ prolapse
DOI: 10.5742/MEWFM.2017.93075
[pdf
version]
Mahnaz Yavangi, Tahereh Mahmoodvand, Saeid Heidari-Soureshjani
The
effect of Hypertonic Dextrose injection on the
control of pains associated with knee osteoarthritis
DOI: 10.5742/MEWFM.2017.93076
[pdf
version]
Mahshid Ghasemi, Faranak Behnaz, Mohammadreza
Minator Sajjadi, Reza Zandi,
Masoud Hashemi
Evaluation
of Psycho-Social Factors Influential on Emotional
Divorce among Attendants to Social Emergency
Services
DOI: 10.5742/MEWFM.2017.93077
[pdf
version]
Farangis Soltanian
Models and Systems of Health Care
Organizational
Justice and Trust Perceptions: A Comparison
of Nurses in public and private hospitals
DOI: 10.5742/MEWFM.2017.93078
[pdf
version]
Mahboobeh Rajabi, Zahra Esmaeli Abdar, Leila
Agoush
Case series and Case reports
Evaluation
of Blood Levels of Leptin Hormone Before and
After the Treatment with Metformin
DOI: 10.5742/MEWFM.2017.93079
[pdf
version]
Elham Jafarpour
Etiology,
Epidemiologic Characteristics and Clinical Pattern
of Children with Febrile Convulsion Admitted
to Hospitals of Germi and Parsabad towns in
2016
DOI: 10.5742/MEWFM.2017.93080
[pdf
version]
Mehri SeyedJavadi, Roghayeh Naseri, Shohreh
Moshfeghi, Irandokht Allahyari, Vahid Izadi,
Raheleh Mohammadi,
Faculty development
The
comparison of the effect of two different teaching
methods of role-playing and video feedback on
learning Cardiopulmonary Resuscitation (CPR)
DOI: 10.5742/MEWFM.2017.93081
[pdf
version]
Yasamin Hacham Bachari, Leila Fahkarzadeh, Abdol
Ali Shariati
Office based family medicine
Effectiveness
of Group Counseling With Acceptance and Commitment
Therapy Approach on Couples' Marital Adjustment
DOI: 10.5742/MEWFM.2017.93082
[pdf
version]
Arash Ziapour, Fatmeh Mahmoodi, Fatemeh Dehghan,
Seyed Mehdi Hoseini Mehdi Abadi,
Edris Azami, Mohsen Rezaei
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| October 2017 -
Volume 15, Issue 8 |
|
|
Barriers to the management
of ventilator-associated pneumonia: A qualitative
study of critical care nurses’ experiences
Fereshteh Rashnou
(1)
Tahereh Toulabi (2,3)
Shirin Hasanvand (2,3)
Mohammad Javad Tarrahi (4)
(1) Student Research Committee, Lorestan
University of Medical Sciences, Khorramabad,
Iran.
(2) Social Determinants of Health Research Center,
Lorestan University of Medical Sciences, Khorramabad,
Iran.
(3) School of Nursing& Midwifery, Lorestan
University of Medical Sciences, Khorramabad,
Iran.
(4) Department of Epidemiology and Biostatistics,
School of Health, Isfahan University of Medical
Sciences, Isfahan, Iran.
Correspondence:Tahereh Toulabi, Social Determinants
of Health Research Center, Lorestan University
of Medical Sciences, Khorramabad, Iran.
Phone numbers: +989161613969 - +986633120140
Fax: +986633120140
Email: tolabi.t@lums.ac.ir
|
Abstract
Background & Aims: Ventilator-associated
pneumonia (VAP) is associated with serious
complications such as morbidity and mortality,
prolonged hospital stay, and great financial
burden. The purpose of this study was
to explore critical care nurses’
experiences of the barriers to VAP management.
Materials &
Methods: This descriptive qualitative
study was done in 2015 using the conventional
content analysis approach. A purposive
sample of twelve critical care nurses
was selected. Data were collected through
unstructured interviews and focus group
discussions. Graneheim and Lundman’s
qualitative content analysis was employed
for data analysis. The trustworthiness
of the data and the findings was ensured
by adopting the criteria proposed by Lincoln
and Guba.
Results:
The major barriers to VAP management were
low quality of working life and poor organizational
culture.
Conclusion:
Nurses can help manage effective VAP through
learning new and standard approaches to
care delivery and adhering to standards
of care.
Key words:
VAP management, Quality of working life,
Organizational culture
|
Nosocomial infections are a major global health
problem (1, 2) and the commonest complication
of hospital care (3). The most prevalent and
fatal nosocomial infection in intensive care
units (ICUs) is ventilator-associated pneumonia
(VAP) (4). The prevalence of VAP is as high
as 9%–27% (5).
Intubated patients rapidly develop VAP within
the first five days after intubation (5, 6).
The risk factors for VAP are numerous and include
accumulation of secretions behind the cuff of
the endotracheal tube, impaired cough reflex,
reduced ciliary activity, immobility, lying
in the supine position (7), aging, underlying
conditions, altered consciousness, endotracheal
intubation, poor nutrition, healthcare workers’
poor hand hygiene (8), hypoxia, naso-gastric
tube, acidosis, pulmonary edema, immunosuppression
(9), burns, disorders of the central nervous
system, severity of the underlying conditions,
re-intubation, and surgery (10).
VAP extends the duration of mechanical ventilation,
prolongs ICU and hospital stay (11 and 12),
and expands hospital staff’s workload (11).
Besides, it is responsible for half of all antibiotic
prescriptions for patients receiving mechanical
ventilation (8) and imposes a heavy financial
burden on patients and healthcare systems (13).
According to Lawrence and Fulbrook (2011), VAP
adds to the cost of hospital care by 40,000
US dollars per patient per hospital admission
(14).
Given the serious complications of VAP and
the priority of prevention over treatment, VAP
prevention is the most cost-effective and optimal
way for fighting VAP (15). Studies have shown
that one third of all nosocomial infections
such as VAP are preventable (16). Currently,
VAP prevention is considered as one of the key
components of patient safety guidelines (4),
a main safety goal (17), and a quality improvement
indicator in most healthcare systems, and a
criterion for evaluating ICUs (18).
Despite many efforts for controlling VAP, its
incidence rate is still very high and it is
the most fatal nosocomial infection. Consequently,
prevention and management of VAP necessitate
continuous monitoring (19), effective problem
assessment, and all-party support. According
to Lambert et al. (2013), all hospital staff
need to receive continuing education about VAP
management. Moreover, preventive measures should
be designed to improve the quality of hospital
care (17).
Nurses are the most important component of
nosocomial infection prevention programs (20).
As healthcare providers who have constant presence
in clinical settings, nurses have significant
roles in preventing and managing health problems
and providing care to patients. In addition,
implementing VAP prevention strategies is among
the key responsibilities of nurses. Thus, exploring
their experiences is of great importance. Nonetheless,
most of the previous studies into VAP prevention
had been done by using quantitative designs,
leaving nurses’ experiences of VAP prevention
poorly explored, if at all. The present study
was made to bridge this gap. The purpose of
the study was to explore critical care nurses’
experiences of the barriers to VAP management.
Design
This descriptive qualitative study was done
by using the conventional content analysis approach
(21).
Setting
The study was conducted in 2015 in a teaching
hospital located in Lorestan Province, Iran.
Participants
Sampling was done through purposeful sampling
and was continued until reaching data saturation
(22). Consequently, twelve critical care nurses
were selected. Nurses were included if they
had at least a bachelor’s degree in nursing,
minimum work experience in ICUs of three months,
desire for sharing their experiences, and stable
psychological state for establishing communication.
We excluded them if they voluntarily withdrew
from the study or avoided sharing their experiences.
Data collection
Semi-structured interviews were carried out
with twelve nurses for data collection, each
of which lasted 30 minutes, on average. Besides,
we held two focus group discussions. The size
of each focus group was six nurses and the length
of the discussions was 25 minutes, on average.
Focus group discussions help collect data from
a large sample of participants in a short period
of time while semi-structured personal interviews
provide a deeper understanding of the intended
phenomenon (23). Broad open-ended interview
questions were employed to delve into the participants’
experiences. Some of the interview questions
were: “What care measures do you use to
prevent VAP?” “How does the physical
structure of your unit affect VAP management?”
“How do the facilities and equipment in
your unit affect VAP management?” “What
are the barriers to VAP management in your unit?”
“What are the facilitators to VAP management
in your unit?” Besides these main interview
questions, follow-up questions were also asked
to clarify ambiguities in experiences shared
by the participants. The interviews and the
focus group discussions were recorded digitally
using a MP3 recorder.
Data analysis
Concurrently with data collection, we performed
data analysis by pursuing the Graneheim and
Lundman’s five-step approach to content
analysis (21). Immediately after holding each
interview, it was transcribed word by word and
read for several times. Then, primary codes
were extracted, compared and merged with each
other, and grouped into categories based on
their similarities.
Rigor and data trustworthiness
The credibility of the data was maintained through
employing the member checking technique, allocating
adequate time to data collection, and arranging
the interviews based on the interviewees’
preferences. Moreover, confirmability was ensured
through sending the interviews, codes, and categories
to several external reviewers and asking them
to assess the accuracy of data analysis, while
dependability was maintained by immediate transcription
and analysis of each interview. The maximum
variation sampling was also employed to enhance
the transferability of the findings (24).
Ethical considerations
Ethical approval for the study was obtained
from the Ethics Committee of Lorestan University
of Medical Sciences, Khorramabad, Iran. After
explaining the aim and the methods of the study
to the participants, their informed consent
for participation in the study and recording
their interviews was secured. They were ensured
that their information would be treated as confidential
and they would have access to the findings.
Most
of
the
participants
were
female
(10
cases).
The
means
of
their
age
and
professional
experience
were
25.3
and
4.6
years,
respectively.
Their
experiences
of
the
barriers
to
VAP
management
came
into
two
main
themes
of
low
quality
of
working
life
and
poor
organizational
culture
which
are
shown
in
Table
1
and
explained
in
what
follows.
Table
1:
Main
themes,
categories
and
subcategories
of
critical
care
nurses’
experiences
of
the
barriers
to
VAP
management
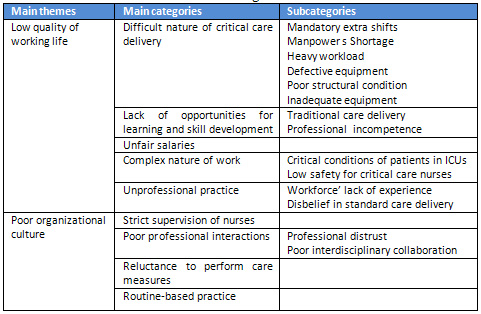
A.
Low
quality
of
working
life
Quality
of
working
life
(QWL)
is
the
result
of
workers’
satisfaction
with
their
needs
and
is
achieved
through
attending
workplaces.
In
healthcare
organizations,
QWL
is
among
the
principal
factors
behind
the
quality
of
workers’
performance
and
care.
According
to
our
participants,
low
QWL
was
among
the
main
barriers
to
effective
VAP
management.
The
five
main
categories
of
this
main
theme
were
difficult
nature
of
critical
care
delivery,
lack
of
opportunities
for
learning
and
skill
development,
unfair
salaries,
complex
nature
of
work,
and
unprofessional
practice.
A1.
Difficult
nature
of
critical
care
delivery
Critical
care
delivery
is
complex
and
difficult
because
patients
who
are
hospitalized
in
ICUs
usually
are
critically
ill
and
suffer
from
life-threatening
conditions.
The
participating
nurses
referred
to
low
nurse-patient
ratio
as
a
major
barrier
to
effective
VAP
management.
The
number
of
nurses
is
low
and
we
have
to
do
extra
working
shifts.
Therefore,
we
are
too
fatigued
to
provide
quality
care.
Or,
we
are
very
busy
at
work.
There
are
only
two
nurses
in
each
shift
and
hence,
we
have
not
adequate
time
for
implementing
care
measures
properly.
For
instance,
instead
of
letting
gavage
soup
pass
through
the
nasogastric
tube,
we
push
it
forcibly
by
using
a
gavage
syringe.
Another
instance
is
that
we
do
not
perform
suctioning
properly
in
order
to
be
able
to
carry
out
our
other
care-related
responsibilities
(P.
2).
Nursing
staff
shortage
negatively
affected
the
participants’
care
quality
through
increasing
their
workload
and
the
number
of
their
mandatory
extra
shifts.
Mandatory
extra
shift
was
referred
to
by
the
participants
as
another
barrier
to
effective
VAP
management.
Such
working
schedule
tired
them,
disturbed
their
personal
life,
broke
their
concentration,
and
reduced
the
quality
of
care.
As
I
have
a
little
baby,
I
don’t
want
to
do
extra
shifts.
However,
the
hospital
nursing
office
doesn’t
agree
and
thus,
I
have
to
do
extra
shifts.
When
doing
extra
shifts,
I’m
greatly
preoccupied
with
my
baby
and
hence,
I
cannot
perform
my
tasks
properly.
For
instance,
I
may
avoid
performing
suctioning
accurately
(P.
1).
Another
workforce-related
barrier
to
effective
VAP
management
was
lack
of
professional
physiotherapists
in
hospitals.
Therefore,
the
participants
were
required
to
do
the
extra
task
of
performing
physiotherapy
for
patients.
However,
they
considered
physiotherapy
neither
as
their
own
responsibilities
nor
as
a
routine
practice
and
hence,
it
was
usually
overlooked.
It
is
for
about
two
years
that
there
is
no
physiotherapist
in
our
hospital
and
thus,
physiotherapy
is
usually
performed
by
us
even
though
it
is
not
among
our
responsibilities.
We
perform
physiotherapy
only
for
the
sake
of
patients.
Of
course,
our
physiotherapies
are
not
standard
enough
(P.
3).
Critical
conditions
of
patients
who
are
hospitalized
in
ICUs
and
their
greater
need
for
specialized
care
services
along
with
serious
staff
shortage
had
dramatically
expanded
our
participants’
workload.
Such
a
working
condition
had
forced
them
to
pay
little
attention
to
the
quality
of
care.
On
the
other
hand,
during
shift
handover,
the
quantity
of
care
was
valued
much
greater
than
its
quality.
In
other
words,
if
nurses
performed
smaller
number
of
their
tasks
with
greater
quality,
they
were
accused
of
shirking.
Such
a
practice
had
resulted
in
the
delivery
of
low-quality
care.
When
I’m
too
busy,
I
cannot
perform
suctioning
or
other
care
measures
accurately
because
I
need
to
perform
each
measure
quickly
in
order
to
have
adequate
time
for
my
other
tasks.
Thus,
I
usually
pay
little
attention
to
the
quality
of
work
because
during
shift
handover,
no
one
values
the
quality
of
my
care;
rather,
they
only
value
the
amount
of
undone
tasks.
Therefore,
I
need
to
do
all
my
tasks
at
any
level
of
quality
in
order
not
to
be
accused
of
shirking
(P.
4).
Despite
the
necessity
to
use
high-tech
equipment
in
ICUs,
our
participants
noted
that
they
had
little
access
to
such
equipment.
They
referred
to
defective
or
inadequate
equipment
as
another
barrier
to
effective
VAP
management.
In
other
words,
they
had
many
difficulties
in
providing
quality
patient
care
due
to
having
limited
access
to
basic
critical
care
equipment.
Defective
equipment
resulted
in
providing
nonstandard
care
while
lack
of
equipment
resulted
in
failure
to
perform
some
care
measures
such
as
measuring
the
pressure
of
endotracheal
tube
cuff.
The
remote
controllers
of
the
beds
in
our
unit
are
defective.
When
we
are
too
busy
with
other
care
measures,
we
are
unable
to
change
the
controllers
and
thus,
patients
may
be
in
an
inaccurate
position
during
gavage
(P.
5).
We
never
measure
the
pressure
of
endotracheal
tube
cuff
because
we
have
no
access
to
the
necessary
equipment
(P.
7).
Another
barrier
to
effective
VAP
management
was
poor
and
nonstandard
structural
conditions
of
ICUs
both
for
patients
and
nurses.
For
instance,
the
participants’
working
unit
had
neither
an
air
conditioning
system
nor
an
isolated
room
for
patients
with
infectious
diseases.
Besides,
the
windows
to
open
space
were
kept
open
for
long
hours
and
inter-bed
distances
were
too
small.
Therefore,
the
likelihood
of
infection
transmission
was
high.
In
addition,
the
staff
resting
room
was
in
poor
condition.
The
physical
space
of
the
unit
is
too
awful.
There
is
a
small
space
between
the
beds
and
there
is
no
air
conditioning
system
in
the
unit.
In
case
of
poor
air
conditioning,
both
nurses
and
patients
are
at
risk
of
bacterial
infections
(P.
6).
A2.
Lack
of
opportunities
for
learning
and
skill
development
One
of
the
key
characteristics
of
critical
care
nurses
is
to
have
great
knowledge
of
care.
In
other
words,
nurses
who
are
not
knowledgeable
enough
cannot
work
in
these
units.
Nonetheless,
our
participants’
experiences
showed
that
critical
care
services
were
provided
based
on
usual
routines.
In
other
words,
novice
nurses
learned
the
way
of
care
delivery
from
their
experienced
colleagues
and
took
professional
knowledge-based
practice
for
granted.
Such
a
practice
had
resulted
in
nonstandard
care
delivery.
The
most
important
thing
for
us
is
that
the
endotracheal
tube
cuff
be
kept
full.
Therefore,
other
things
(such
as
the
pressure
of
the
cuff)
are
not
very
important.
We
just
inject
5
cc
of
air
into
the
cuff.
According
to
the
participants,
some
critical
care
nurses
did
not
have
enough
professional
competence
for
working
in
ICUs
due
to
poor
in-service
education.
For
instance,
some
nurses
were
not
skillful
enough
for
measuring
the
pressure
of
endotracheal
tube
cuff
or
doing
physiotherapy.
Moreover,
as
attending
physicians
or
anesthesiologist
refrained
from
setting
ventilators,
nurses
were
obliged
to
do
this
task
despite
having
received
no
in-depth
training
in
this
area.
Consequently,
they
set
ventilators
based
on
their
own
personal
experience.
I
have
no
adequate
knowledge
about
ventilators.
Thus,
there
may
be
an
opportunity
for
weaning
a
patient
from
the
ventilator
while
I
cannot
take
advantage
of
such
opportunity
due
to
having
poor
weaning
skills.
Therefore,
the
patient
may
unnecessarily
receive
mechanical
ventilation
for
many
days
(P.
8).
A3.
Unfair
salaries
Because
of
their
heavier
workload
and
stressful
work
condition,
the
participating
nurses
expected
to
receive
higher
salaries
compared
with
nurses
in
other
hospital
wards.
However,
hospital
administrators’
inattention
to
fair
budget
and
resource
allocation
had
reduced
their
motivation
for
work.
Financial
issues
were
so
important
to
the
nurses
that
they
referred
to
them
as
a
significant
factor
behind
care
quality.
The
salaries
of
critical
care
nurses
should
be
different
from
those
of
nurses
in
other
hospital
wards.
However,
there
is
no
difference
between
the
salaries
of
these
two
groups
in
our
hospital.
Sometimes,
critical
care
nurses’
salaries
are
even
less
than
other
nurses.
Such
practice
significantly
contributes
to
our
poor
motivation
for
work
(P.
1).
A4.
Complex
nature
of
work
When
providing
care
to
critically-ill
patients
in
critical
situations,
the
nurses
focused
mainly
on
saving
patients’
life
and
paid
little
attention,
if
any,
to
the
requirements
of
each
care-related
activity.
Accordingly,
they
might
insert
an
intra-tracheal
tube
or
perform
suctioning
under
unsterile
conditions,
resulting
in
greater
risk
for
VAP.
The
likelihood
of
such
an
unsterile
practice
was
greater
in
stressful
situations
such
as
in
emergencies
or
once
working
with
an
inexperienced
colleague.
When
a
patient
is
critically-ill
and
needs
intubation,
I
just
focus
on
intubating
him/her
irrespective
of
the
quality
or
the
sterility
of
the
procedure.
The
most
important
thing
in
such
situations
is
to
prevent
patient’s
death
(P.
9;
group
discussion).
Shortage
of
personal
protective
equipment
had
also
caused
most
of
the
participants
to
develop
hospital-acquired
respiratory
infections.
They
referred
to
this
fact
as
a
negative
experience
and
mentioned
that
they
avoid
providing
standard
care
to
patients
with
serious
infections
in
order
to
protect
themselves
against
infections.
Here,
I
developed
pneumonia
several
times.
In
order
to
prevent
another
episode
of
pneumonia,
I
perform
suctioning
for
patients
with
pneumonia
in
a
very
short
period
of
time.
Such
practice
reduces
the
quality
of
my
care
(P.
6).
A5.
Unprofessional
practice
Due
to
the
critical
conditions
of
patients
who
are
hospitalized
in
ICUs,
critical
care
nurses
need
to
have
high
levels
of
critical
care
specialty,
knowledge,
and
experience.
They
not
only
need
to
be
highly
knowledgeable,
but
also
should
properly
use
their
knowledge
in
their
practice.
Nonetheless,
nursing
staff
shortage
in
the
study
setting
had
resulted
in
the
recruitment
of
inexperienced
nurses
for
ICU.
Inexperienced
nurses
avoided
providing
care
services
independently
in
order
not
to
be
involved
in
malpractice
lawsuits.
I
avoid
weaning
a
patient
from
ventilator
independently
and
attempt
to
do
it
after
obtaining
my
senior
or
manager’s
permission.
I
usually
perform
what
they
recommend
(P.
8).
Some
of
the
participating
nurses
had
no
healthy
attitude
toward
quality
care
delivery
and
hence,
they
used
to
provide
care
based
on
their
own
beliefs
and
experience.
For
instance,
some
of
them
did
not
maintain
sterility
while
doing
nursing
procedures
and
believed
that
such
practice
is
sound.
When
I
go
from
one
patient
to
another,
I
simply
change
my
gloves
and
believe
that
it
is
enough
for
preventing
infections.
I
have
no
firm
belief
in
washing
hands
before
doing
procedures
(P.
9,
group
discussion).
B.
Poor
organizational
culture
Another
major
barrier
to
effective
VAP
management
was
poor
organizational
culture.
Organizational
culture
has
a
significant
effect
on
organizational
and
employee
performance.
Factors
such
as
supervision
and
control,
organizational
relations,
and
managerial
support
can
contribute
to
the
formation
of
cultural
norms.
B1.
Strict
supervision
of
nurses
Our
nurses
were
continuously
monitored
by
their
administrators.
However,
they
believed
that
evaluation
of
employee
performance
is
not
performed
effectively
because
administrators
who
did
evaluations
usually
focused
more
on
nursing
documentations
than
the
process
of
care
delivery
and
attempted
to
pinpoint
employees’
weaknesses
in
order
to
punish
them
instead
of
minimizing
shortages
and
weaknesses.
Some
of
the
participants
also
argued
that
administrators
usually
evaluate
each
nurse
based
on
their
own
previous
attitudes
towards
her/him.
Such
a
poor
evaluation
had
reduced
the
participants’
motivation
for
quality
care
delivery.
Previously,
they
recruited
many
novice
staff
to
the
unit
and
thus,
several
errors
happened
in
the
unit
and
all
of
us
were
punished
consequently.
Thereafter,
they
never
pay
attention
to
the
ICU
and
our
matron
believes
that
ICU
staff
never
perform
their
tasks
appropriately
(P.
10).
B2.
Poor
professional
interactions
The
ability
to
establish
effective
communications
with
colleagues
is
a
basic
clinical
skill
and
a
key
component
of
efficient
care
delivery
in
ICUs.
Nonetheless,
most
participants
referred
to
poor
inter-
and
intra-professional
interactions
as
another
barrier
to
effective
VAP
management.
Inter-professional
distrust
and
poor
interdisciplinary
collaboration
were
among
the
participants’
main
concerns.
In
the
study
setting,
physicians
had
no
trust
in
nurses
and
accused
them
of
shirking,
resulting
in
the
reduction
of
nurses’
motivation
for
quality
care
delivery.
Every
morning,
we
wash
and
rinse
patients’
mouth
with
chlorhexidine.
However,
when
attending
the
unit,
physicians
get
angry
and
complain
that
why
we
do
not
perform
mouth
washing
for
patients.
They
do
not
trust
us
when
we
say
that
we
have
done
mouth
washing.
Such
behaviors
of
physicians
make
us
unmotivated
(P.
5).
On
the
other
hand,
there
were
weak
intra-professional
interactions
among
nurses
due
to
their
heavy
workload.
In
other
words,
they
were
unable
to
help
each
other
in
doing
care-related
activities.
Sometimes,
the
nurses
were
even
unable
to
perform
their
activities
due
to
the
lack
of
help
and
support.
I
cannot
ask
my
colleagues
to
help
me
because
they
are
heavily
involved
with
their
own
duties.
If
they
help
me,
their
duties
would
remain
undone.
Therefore,
I
cannot
efficiently
perform
suctioning
when
I’m
alone
(P.
11).
B3.
Reluctance
to
perform
care
measures
Our
participants’
detailed
another
problem
in
managing
VAP
as
their
reluctance
and
lack
of
motivation
for
performing
care
measures.
Factors
contributing
to
such
reluctance
were,
but
not
limited
to,
inaccurate
judgments,
administrators’
inattention
to
nurses,
poor
accommodation
for
nurses,
and
similar
salaries
for
critical
care
nurses
and
the
nurses
of
other
hospital
wards.
Such
situations
disappointed
the
participants
and
hence,
they
had
no
motivation
for
better
care
delivery.
Our
resting
room
is
of
poor
condition.
No
one
values
our
welfare.
When
we
go
to
the
resting
room
to
take
some
rest,
such
problems
add
psychological
fatigue
to
our
physical
fatigue
because
we
feel
that
no
one
values
us
(P.
10).
B4.
Routine-based
practice
The
other
barrier
to
effective
VAP
management
was
nurses’
routine-based
practice
due
to
lack
of
efficient
incentive
systems
and
poor
workforce
development
policies.
According
to
the
participants,
their
administrators
paid
little
attention,
if
any,
to
their
career
advancement
and
professional
development,
did
not
encourage
them,
and
used
punishment
instead
of
encouragement.
Therefore,
the
nurses
were
reluctant
to
learn
and
provide
quality
care.
If
you
do
your
tasks
correctly,
our
administrators
never
encourage
you.
However,
if
you
commit
an
error,
they
will
punish
you.
The
predominant
system
in
our
setting
is
punishment
not
incentive
(P.
1).
The
purpose
of
the
study
was
to
explore
critical
care
nurses’
experiences
of
the
barriers
to
VAP
management.
The
study
findings
indicated
that
there
were
many
barriers
to
effective
VAP
management
in
ICUs.
One
of
the
major
barriers
to
VAP
management
was
nurses’
low
QWL.
Mullen
(2015)
also
noted
that
in
the
United
States,
nurses
face
many
barriers
in
their
working
life
(25).
Long
working
hours
due
to
mandatory
extra
shifts
was
among
the
factors
which
contributed
to
the
difficulty
of
critical
care
delivery,
nurses’
fatigue,
and
reduced
quality
of
nursing
care.
Olds
et
al
(2010)
also
reported
that
increased
work
hours
raise
the
likelihood
of
adverse
events
and
errors
in
healthcare
(26).
Renata
et
al.
(2012)
also
found
nurses’
heavy
workload
as
a
risk
factor
for
nosocomial
infections
(27).
Duffin
(2014)
noted
that
higher
nurse-bed
ratio
prolongs
patients’
survival
in
ICUs
(28).
The
results
of
studies
made
by
Laschinger
et
al.
(2000)
also
illustrated
that
putting
nurses
under
pressure
leaves
them
with
feelings
such
as
dissatisfaction,
frustration,
and
powerlessness
(29)
and
affects
their
QWL.
Our
findings
also
showed
that
lack
of
professional
physiotherapists
in
hospitals
results
in
added
responsibilities
for
nurses.
It
is
noteworthy
that
as
a
key
component
of
critical
care,
physiotherapy
is
of
paramount
importance
to
effective
airway
clearance
and
VAP
management
(30).
We
also
found
that
nonstandard
physical
structure
of
ICU
and
defects
or
shortages
of
high-tech
equipment
in
this
unit
reduced
care
quality
and
interfered
with
effective
care
delivery.
This
finding
is
in
line
with
the
findings
reported
by
Matakala
et
al.
(2014)
who
reported
that
the
design
of
ICU
can
affect
care
delivery,
outcomes
of
care,
and
the
incidence
of
infections
(31).
Another
finding
of
the
study
was
that
care
services
were
provided
based
on
old
routines.
Lack
of
opportunities
for
learning
and
skill
development
requires
nurses
to
deliver
care
services
more
based
on
old
routines
and
personal
experiences
than
clinical
standards
and
guidelines.
Studies
showed
that
the
nursing
care
delivery
system
in
Iran
is
congruent
with
the
attributes
of
Johnson’s
Delegated
Medical
Care
model.
In
this
model,
the
cornerstone
of
care
is
routine-based
practice
and
execution
of
medical
orders
(32).
Evidence
shows
that
one
of
the
key
prerequisites
to
effective
VAP
prevention,
particularly
in
countries
with
limited
resources,
is
continuing
education
of
healthcare
workers
(33,
34).
In
fact,
poor
in-service
training
would
result
in
nonstandard
care
delivery.
Study
findings
also
revealed
unfair
salaries
as
another
factor
affecting
nursing
care
delivery
and
VAP
management
in
ICUs.
Administrators’
indifference
toward
same
salaries
for
critical
care
nurses
and
nurses
working
in
other
hospital
wards
had
reduced
our
participants’
motivation
for
work
and
the
quality
of
their
care.
Unfair
payment
for
different
groups
of
hospital
staff
has
been
reported
as
a
significant
factor
behind
nurses’
poor
motivation
for
work
(35
and
36).
Unfulfilled
work-related
needs
of
nurses
(such
as
need
for
personal
protective
equipment)
had
faced
the
study
participants
with
serious
complications
such
as
pneumonia
and
thereby,
reduced
the
quality
of
their
care.
According
to
Stone
et
al.
(2004),
nurses’
working
condition
is
among
the
major
risk
factors
for
healthcare-related
infections
and
occupational
exposure
to
infections
(37).
Evidence
indicates
that
healthcare
workers
are
at
risk
for
developing
hospital-acquired
infections.
Moreover,
nurses’
safety
and
occupational
health
have
been
reported
to
be
correlated
with
their
job
satisfaction
(38).
Alex
(2011)
also
found
job
satisfaction
as
a
determining
factor
behind
hospital
staff’s
performance
and
the
quality
of
their
care
services
(39).
According
to
the
findings
of
the
present
study,
nurses’
disbelief
in
standard
care
delivery
was
another
main
factor
contributing
to
VAP
management.
Such
disbelief
can
result
in
arbitrary
care
delivery.
Studies
have
shown
a
significant
correlation
between
individuals’
attitudes
and
their
behavioral
pattern.
For
instance,
Noruzi
et
al.
(2015)
found
that
nurses’
personal
attitudes
and
beliefs
are
correlated
with
their
adherence
to
infection
prevention
standards
(40).
On
the
other
hand,
study
findings
revealed
that
nurses’
professional
experience
had
a
significant
role
in
VAP
management
and
standard
care
provision.
In
other
words,
nurses
with
limited
professional
experience
provided
lower
quality
care.
The
results
of
a
study
by
Jafari
et
al.
(2012)
illustrated
that
novice
nurses’
professional
competence
is
not
proportionate
to
the
requirements
of
clinical
settings
and
hence,
they
provide
low-quality
care
(41).
Vogus
et
al.
(2014)
also
reported
that
in
their
first
year
of
professional
practice,
novice
nurses’
performance
is
significantly
affected
by
environment,
workplace
conditions,
and
work-related
factors
(42).
Generally,
workplace
culture
and
atmosphere
can
dramatically
affect
ward
outcomes
such
as
staff
performance
(43).
We
also
found
that
factors
such
as
strict
supervision
of
nurses
and
inappropriate
evaluation
of
employee
performance
reduced
the
nurses’
motivation
for
work,
gave
them
a
negative
attitude
towards
their
administrators,
and
prevented
them
from
correcting
their
errors.
The
administrators
of
the
study
settings
paid
little
attention
to
the
quality
of
care
and
focused
mainly
on
spotting
employees’
errors
and
punishing
them.
According
to
the
Social
Contracts
Theory,
nurses
who
feel
injustice
in
performance
evaluation,
experience
some
kind
of
negative
tension
and
attempt
to
reduce
their
involvement
in
the
organization’s
affairs
in
order
to
relieve
their
tension.
On
the
other
hand,
nurses
who
feel
that
performance
evaluation
is
performed
fairly
become
motivated
to
play
a
more
significant
role
in
their
organizations
(44).
The
study
findings
also
indicated
that
poor
professional
interactions
(such
as
inter-professional
distrust)
reduced
the
quality
of
VAP-related
care
services.
Moreover,
nurses’
heavy
workload
had
undermined
their
ability
to
closely
collaborate
with
each
other.
Havens
(2010)
reported
that
improving
nurses’
relationships
with
other
healthcare
professionals
can
lower
the
rate
of
nosocomial
infections
and
improve
the
quality
of
care
(45).
Two
other
significant
factors
behind
ineffective
VAP
management
in
the
study
setting
were
routine-based
practice
and
lack
of
innovation
at
work
due
to
administrators’
inattention
to
personnel
and
the
dominance
of
punishment
system.
These
findings
are
contrary
to
the
findings
reported
by
Sajadi
et
al.
(2011)
who
found
no
significant
correlation
between
nurses’
creativity
and
organizational
culture
(46).
This
contradiction
may
be
due
to
differences
in
the
design
and
the
setting
of
these
two
studies.
This
study
was
done
in
a
single
ICU
setting
and
thus,
the
findings
may
have
limited
generalizability.
Therefore,
conducting
further
studies
in
different
settings
is
recommended
in
order
to
identify
other
barriers
to
effective
VAP
management.
Poor
structural
and
process
standards
as
well
as
poor
organizational
culture
are
the
major
barriers
to
effective
VAP
management.
The
findings
of
the
present
study
enhanced
our
understanding
of
the
fact
that
administrators
need
to
adopt
strategies
to
improve
nurses’
welfare
and
motivation,
alleviate
their
problems,
boost
their
salaries,
enhance
the
quality
of
performance
supervision
and
evaluation,
and
recruit
more
nurses
into
ICUs.
On
the
other
hand,
nurses
need
to
learn
new
and
standard
approaches
to
care
delivery
in
order
to
play
a
more
significant
role
in
VAP
management.
Future
studies
are
recommended
to
develop
and
implement
strategies
to
improve
organizational
cultures
and
nurses’
QWL
as
well
as
to
change
nurses’
personal
beliefs
and
attitudes.
Acknowledgement
This
study
was
part
of
a
Master’s
thesis
in
Critical
Care
Nursing.
The
authors
are
grateful
to
all
participants
of
the
study
who
shared
their
experiences
and
the
Research
Administration
of
Lorestan
University
of
Medical
Sciences
which
approved
and
funded
the
study.
Guénou
M.
Prevalence
of
nosocomial
infections
and
anti-infective
therapy
in
Benin:
results
of
the
first
nationwide
survey
in
2012.
ARIC
2014;
3(17):
1-6.
doi:
10.1186/2047-2994-3-17
2.
Morgan
D,
Lomotan
L,
Agnes
K,
Grail
L,
Roghmann
M.
Characteristics
of
healthcare-associated
infections
contributing
to
unexpected
in-hospital
deaths.
Infect
Control
Hosp
Epidemiol
2010;
31(8):
864–866.
doi:
10.1086/655018
3.
Harris
A,
Pineles
L,
Belton
B,
Johnson
K,
Shardell
M,
Loeb
M,
et
al.
Universal
glove
and
gown
use
and
acquisition
of
antibiotic
resistant
bacteria
in
the
ICU:
a
randomized
trial.
JAMA
2013;
310(15):
1571-1580.
doi:
10.1001
4.
Bagheri
M,
Amiri
M.
Nurse’s
knowledge
of
evidence-
based
guidelines
for
preventing
ventilator-
associated
pneumonia
in
intensive
care
units.
JNMS
2014;
1(1):
44-48.
URL
http://jnms.mazums.ac.ir/browse.php?a_code=A-10-327-1&slc_lang=en&sid=1
5.
Kalanuria
A,
Zai
W,
Mirski
M.
Ventilator-associated
pneumonia
in
the
ICU.
Crit
Care
Med
2014;
18(208):
1-8.
doi:
10.1186/cc13775
6.
Sharma
S,
Kaur
J.
Randomized
control
trial
on
efficacy
of
chlorhexidine
mouth
care
in
prevention
of
ventilator-
associated
pneumonia.
NMRJ
2012;
8(2):
169-
178.
7.
Gadani
H,
Vyas
A,
Kar
AK.
A
study
of
ventilator-associated
pneumonia:
Incidence,
outcome,
risk
factors
and
measures
to
be
taken
for
prevention.
Indian
J
Anaesth.
2010;
54(6):535-40.
doi:
10.4103/0019-5049.72643.
8.
Darvishi
Khezri
H.
The
role
of
oral
care
in
prevention
of
ventilator
associated
pneumonia:
A
literature
Review.
JSSU
2014;
21(6):
840-849.
http://jssu.ssu.ac.ir/browse.php?a_code=A-10-1499-1&slc_lang=en&sid=1
9.
Behesht
Aeen
F,
Zolfaghari
M,
Asadi
Noghabi
AA.
Nurses’
performance
in
prevention
of
ventilator
associated
pneumonia.
Hayat
2013;
19(3):
17-27.
http://hayat.tums.ac.ir/browse.php?a_code=A-10-26-3&slc_lang=en&sid=1
10.
Bonsal
Cooper
V,
Haut
C.
Preventing
ventilator-
associated
pneumonia
in
children:
an
evidence-based
protocol.
Critical
Care
Nurse
2013;
33(3):
29-21.
doi:
10.4037/ccn2013204
11.
Rello
J,
Lode
H,
Cornaglia
G,
Masterton
R.
A
European
care
bundle
for
prevention
of
ventilator-associated
pneumonia.
Intensive
care
med
2010;
36(5):
773-780.
doi:
10.1007/s00134-010-1841-5
12.
Aminzadeh
Z,
Hajiekhani
B.
Bacterial
endotracheal
tube
colonization
in
intubated
patients
in
poisoning
ICU
ward
of
Loghman
Hakim
hospital
of
Tehran
in
2005.
Horizon
Med
Sci.
2007;
13
(2):12-19.
http://hms.gmu.ac.ir/browse.php?a_code=A-10-1-56&slc_lang=en&sid=1
13.
Salehifar
E,
Abed
S,
Mirzaei
E,
Kalhor
S,
Eslami
G,
Ala
S,
et
al
.
Evaluation
of
profile
of
Microorganisms
involved
in
hospital-acquired
infections
and
their
antimicrobial
resistance
pattern
in
intensive
care
units
of
Emam
Khomeini
hospital,
Sari,
2011-2012.
J
Mazandaran
Univ
Med
Sci.
2013;
22
(1):151-162.
http://jmums.mazums.ac.ir/browse.php?a_code=A-10-29-90&slc_lang=en&sid=1
14.
Lawrence
P,
Fulbrook
P.
The
ventilator
care
bundle
and
its
impact
on
ventilator-
associated
pneumonia:
a
review
of
the
evidence.
BACCN
2011;
16(5):
222-234.
doi:
10.1111/j.1478-5153.2010.00430.x.
15.
Mousavi
S,
Hasibi
M,
Mokhtari
Z,
Shaham
G.
Evaluation
of
safety
standards
in
operating
rooms
of
Tehran
University
of
Medical
Sciences(TUMS)
Hospitals
in
2010.
PAYAVARD
2011;
5(2):
10-17.
http://payavard.tums.ac.ir/browse.php?a_code=A-10-25-73&slc_lang=en&sid=1
16.
Mari
N,
Udilja
kN,
Karaula
NT,
Jurina
H,
Makovi
M,
Beki
D.
The
impact
of
interventions
to
improve
adherence
to
preventive
measures
on
the
incidence
of
nosocomial
infections
in
ICUs.
SIGNA
VITAE
2014;
9
(1):
34
–
37.
17.
Lambert
M,
Palomar
M,
Agodi
A,
Hiesmyr
M,
Lepape
A,
Ingenbleek
A.
prevention
of
ventilator-associated
pneumonia
in
intensive
care
units:
an
international
online
survey.
ARIC
2013;
2(9):
1-8.
doi:
10.1186/2047-2994-2-9
18.
Morris
A,
Everingham
K,
Culloch
C,
Nulty
J,
Brooks
O,
Swann
D.
Reducing
ventilator-
associated
pneumonia
in
intensive
care:
impact
of
implementing
a
care
bundle.
Crit
Care
Med
2011;
39(10):
2218-2224.
doi:
10.1097/CCM.0b013e3182227d52
19.
Salimi
s,
Anami
I,
Noroznia
SH.
Rastad
M,
Acdemir
N.
Effect
Of
Standardization
Of
Nursing
Cares
On
Incidence
Of
Nosocomial
Infection
In
Micu.
Urmia
Medical
Journal
2009;
19(4):
310-315.
http://umj.umsu.ac.ir/browse.php?a_code=A-10-3-40&slc_lang=en&sid=1
20.
Jain
M,
Miller
L,
Belt
D,
King
D,
Berwick
M.
Decline
in
ICU
adverse
events
/
nosocomial
infections
and
cost
through
a
quality
improvement
initiative
focusing
on
teamwork
and
culture
change.
Qual
Saf
Health
Care
2006;
15(4):
235-239.
doi:
10.1136/qshc.2005.016576
21.
Graneheim
UH,
Lundman
B.
Qualitative
content
analysis
in
nursing
research:
concepts,
procedures
and
measures
to
achieve
trustworthiness.
Nurse
education
today.
2004;
24(2):105-12.
doi:
10.1016/j.nedt.2003.10.001
22.
Carpenter
D,
Streubert
H,
Speziale
S.
Qualitative
research
in
nursing:
Advancing
the
humanistic
imperative.
Philadelphia:
Lippincott
Williams
and
Wilkins.
2011.
23.
Baraz-Pordanjani
S,
Memarian
R,
Vanaki
Z.
Damaged
professional
identity
as
a
barrier
to
Iranian
nursing
students’
clinical
learning:
a
qualitative
study.
Journal
of
Clinical
Nursing
and
Midwifery.
2014;
3
(3):1-15.
http://jcnm.skums.ac.ir/browse.php?a_code=A-10-86-1&slc_lang=fa&sid=1
24.
Nasiripour
AA,
Radfar
R,
Najaf
Begay
R,
Rahmani
H.
Factors
affecting
the
deployment
of
e-health
system
in
Iran.
jhosp.
2011;
10
(1):53-62
http://jhosp.tums.ac.ir/browse.php?a_code=A-10-25-70&slc_lang=en&sid=1
25.
Mullen
K.
Barriers
to
work-life
balance
for
hospital
nurses
.Workplace
Health
Saf
2015;
63(3):
96-9.
http://dx.doi:
10.1177/2165079914565355
26.
Olds
DM
,
Clarke
SP.
The
effect
of
work
hours
on
adverse
events
and
errors
in
health
care.
J
Safety
Res
2010;
41(2):153-62.
doi:
10.1016/j.jsr.2010.02.002.
27.
Renata
M.
Daud-Gallotti,
Silvia
F,
Thais
G,
Katia
G.
P,
Evelize
N.
I.
Nursing
Workload
as
a
Risk
Factor
for
Healthcare
Associated
Infections
in
ICU:
A
Prospective
Study.
PLoS
One.
2012;
7(12):
1-6.
doi:
10.1371/journal.pone.0052342
28.
Duffin
C.
Increase
in
nurse
numbers
linked
to
better
patient
survival
rates
in
ICU.
Nurs
Stand.
2014
Apr
16-22;
28(33):
10.
doi:10.7748/ns2014.04.28.33.10.s8.
29.
Laschinger
HKS,
Fingan
J,
Shamian
J,
Casier
S.
Organizational
trust
and
empowerment
in
registered
healthcare
setting:
effects
on
staff
nurse
commitment.
Journal
of
Nursing
Administration
2000;
30(9):
413-425.
30.
Pattanshetty
RB1,
Gaude
GS.
Effect
of
multimodality
chest
physiotherapy
in
prevention
of
ventilator-associated
pneumonia:
A
randomized
clinical
trial.
Indian
J
Crit
Care
Med.
2010
14(2):70-6.
doi:
10.4103/0972-5229.68218.
31.
Matlakala
M
C,
Bezuidenhout
MC,
Botha
ADH.
Challenges
encountered
by
critical
care
unit
managers
in
the
large
intensive
care
units.
Curationis;
2014,
37(1):
7.
doi.org/10.4102/curationis.v37i1.1146
32.
Hajbaghery
A.
Factors
influencing
Evidence-based
nursing:
A
Qualitative
study.
IJN.
2006;
19(47):
17-330.
http://ijn.iums.ac.ir/browse.php?a_code=A-10-1-125&slc_lang=en&sid=1
33.
Apisarnthanarak
A,
Pinitchai
U,
Thongphubeth
K,
Yuekyen
C,
David
K.
Warren
DK,
Zack
JE,
Warachan
B,
Victoria
JF.
Effectiveness
of
an
Educational
Program
to
Reduce
Ventilator-Associated
Pneumonia
in
a
Tertiary
Care
Center
in
Thailand:
A
4-Year
Study.
Clinical
Infectious
Diseases
2007;
45:704–11.
doi:
10.1086/520987
34.
Rosa
J,
Montserrat
S,
O´
scar
H,
Esther
C,
Concepcio´
n
T,
Inmaculada
F,
Jordi
V.
Assessment
of
a
training
programme
for
the
prevention
of
ventilator-associated
pneumonia.
Nursing
in
Critical
Care
2012;
17
(6):
285-292.
doi:
10.1111/j.1478-5153.2012.00526.x
35.
Songstad
N
G,
Rekdal
OB,
Massay
DA,
Blystad
A.
Perceived
unfairness
in
working
conditions:
The
case
of
public
health
services
in
Tanzania.
BMC
Health
Serv
Res.
2011;
11(34):
1-15.
doi:
10.1186/1472-6963-11-34
36.
Valizadeh
S,
Haririan
H.
Nurses
Work
Motivation:
A
Big
Challenge
for
Health
System;
a
Review
article.
PCNM
2015-2016:
5(2):
56-64.
http://www.zums.ac.ir/nmcjournal/browse.php?a_code=A-10-24-1&slc_lang=en&sid=1
37.
Stone
PW,
Clarke
SP,
Clarke
J,
Correa-de-Araujo
R.
Nurses’
Working
Conditions:
Implications
for
Infectious
Disease.
Emerging
Infectious
Diseases
2004;
10(11):1984-9.
www.cdc.gov/eid
38.
Jafari
M,
Shafiian
N,
Mahfozpor
S.
The
relationship
between
job
satisfaction
and
occupational
safety
and
occupational
health
status
of
nurses
in
a
hospital.
JHSW.
2012;
2
(3):41-48.
http://jhsw.tums.ac.ir/browse.php?a_code=A-10-25-37&slc_lang=en&sid=1
39.
Alex
MR.
Occupational
Hazards
for
Pregnant
Nurses
AJN,
American
Journal
of
Nursing
2011;
111(1):
28-37.
doi:
10.1097/01.NAJ.0000393056.01687.40
40.
Noruzi
T,
Rassouli
M,
Khanali
Mojen
L,
Khodakarim
S,
Torabi
F.
Factors
associated
with
nosocomial
infection
control
behavior
of
nurses
working
in
nursery
&
NICU
based
on
“Health
Belief
Model”.
JHPM.
2015;
4
(3):1-11.
http://jhpm.ir/browse.php?a_code=A-10-50-2&slc_lang=en&sid=1
41.
Jaffari
Golestan
N,
Vanaki
Z,
Memarian
R.
Organizing
“Nursing
Mentors
Committee”:
an
Effective
Strategy
for
Improving
Novice
Nurses’
Clinical
Competency.
Iranian
Journal
of
Medical
Education.
2008;
7
(2):237-247
http://ijme.mui.ac.ir/browse.php?a_code=A-10-2-288&slc_lang=fa&sid=1
42.
Vogus
TJ,
Cooil
B,
Sitterding
M,
Everett
LQ.
Safety
organizing,
emotional
exhaustion,
and
turn
over
in
hospital
nursing
units.
Medical
care.
2014;
52(10):870-6.
doi:
10.1097/MLR.0000000000000169.
43.
Guidet
B,
González-Romá
V:
Climate
and
cultural
aspects
in
intensive
care
units.
Critical
Care
2011,
15:312.
doi:
10.1186/cc10361.
http://ccforum.com/content/15/6/312
44.
Abbasnezhad
M
H,
Mehdad
A,
Asadpour
M.
The
Relationship
between
Justice
Perception
of
Performance
Appraisal
System
and
Organizational
Citizenship
Behavior
and
Organizational
Commitment
among
Nurses.
Iranian
Journal
of
Medical
Education
2015;
15(31):
240-250.
http://ijme.mui.ac.ir/browse.php?a_code=A-10-2653-1&slc_lang=fa&sid=1
45.
Havens
DS.
Relational
coordination
among
nurses
and
other
providers:
impact
on
the
quality
of
patient
care.
Journal
of
Nursing
Management
2010;
18(N):
926–937.
46.
Sajadi
A,
Rashidi
E,
Ebrahim
zadeh
F.
Determine
the
relationship
between
the
enterprise
and
creativity
of
nurses
in
government
hospitals
of
North
Khorasan.
National
Conference
on
organizational
behavior
in
nursing,
Shirvan,
Islamic
Azad
University
of
Shirvan.
2011.
http://www.civilica.com/Paper-NCQBN01-NCQBN01_025.html
|
|
.................................................................................................................

|
| |
|

