|
|
 |
| ............................................................. |
|
October 2017 -
Volume 15, Issue 8
|
 |
|
View
this issue in pdf formnat - the issue
has been split into two files for downloading
due to its large size: FULLpdf
(12 MB)
Part
1 &
Part
2
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
........................................................
|
|
Original Contribution/Clinical Investigation
Immunity
level to diphtheria in beta thalassemia patients
DOI: 10.5742/MEWFM.2017.93048
[pdf
version]
Abdolreza Sotoodeh Jahromi, Karamatollah Rahmanian,
Abdolali Sapidkar, Hassan Zabetian, Alireza
Yusefi, Farshid Kafilzadeh, Mohammad Kargar,
Marzieh Jamalidoust,
Abdolhossein Madani
Genetic
Variants of Toll Like Receptor-4 in Patients
with Premature Coronary Artery Disease, South
of Iran
DOI: 10.5742/MEWFM.2017.93049
[pdf
version]
Saeideh Erfanian, Mohammad Shojaei, Fatemeh
Mehdizadeh, Abdolreza Sotoodeh Jahromi, Abdolhossein
Madani, Mohammad Hojjat-Farsangi
Comparison
of postoperative bleeding in patients undergoing
coronary artery bypass surgery in two groups
taking aspirin and aspirin plus CLS clopidogrel
DOI: 10.5742/MEWFM.2017.93050
[pdf
version]
Ali Pooria, Hassan Teimouri, Mostafa Cheraghi,
Babak Baharvand Ahmadi, Mehrdad Namdari, Reza
Alipoor
Comparison
of lower uterine segment thickness among nulliparous
pregnant women without uterine scar and pregnant
women with previous cesarean section: ultrasound
study
DOI: 10.5742/MEWFM.2017.93051
[pdf version]
Taravat Fakheri, Irandokht Alimohammadi, Nazanin
Farshchian, Maryam Hematti,
Anisodowleh Nankali, Farahnaz Keshavarzi, Soheil
Saeidiborojeni
Effect
of Environmental and Behavioral Interventions
on Physiological and Behavioral Responses of
Premature Neonates Candidates Admitted for Intravenous
Catheter Insertion in Neonatal Intensive Care
Units
DOI: 10.5742/MEWFM.2017.93052
[pdf
version]
Shohreh Taheri, Maryam Marofi, Anahita Masoumpoor,
Malihe Nasiri
Effect
of 8 weeks Rhythmic aerobic exercise on serum
Resistin and body mass index of overweight and
obese women
DOI: 10.5742/MEWFM.2017.93053
[pdf
version]
Khadijeh Molaei, Ahmad Shahdadi, Reza Delavar
Study
of changes in leptin and body mass composition
with overweight and obesity following 8 weeks
of Aerobic exercise
DOI: 10.5742/MEWFM.2017.93054
[pdf
version]
Khadijeh Molaei, Abbas Salehikia
A reassessment
of factor structure of the Short Form Health
Survey (SF-36): A comparative approach
DOI: 10.5742/MEWFM.2017.93088
[pdf version]
Vida Alizad, Manouchehr Azkhosh, Ali Asgari,
Karyn Gonano
Population and Community Studies
Evaluation
of seizures in pregnant women in Kerman - Iran
DOI: 10.5742/MEWFM.2017.93056
[pdf
version]
Hossein Ali Ebrahimi, Elahe Arabpour, Kaveh
Shafeie, Narges Khanjani
Studying
the relation of quality work life with socio-economic
status and general health among the employees
of Tehran University of Medical Sciences (TUMS)
in 2015
DOI: 10.5742/MEWFM.2017.93057
[pdf version]
Hossein Dargahi, Samereh Yaghobian, Seyedeh
Hoda Mousavi, Majid Shekari Darbandi, Soheil
Mokhtari, Mohsen Mohammadi, Seyede Fateme Hosseini
Factors
that encourage early marriage and motherhood
from the perspective of Iranian adolescent mothers:
a qualitative study
DOI: 10.5742/MEWFM.2017.93058
[pdf
version]
Maasoumeh Mangeli, Masoud Rayyani, Mohammad
Ali Cheraghi, Batool Tirgari
The
Effectiveness of Cognitive-Existential Group
Therapy on Reducing Existential Anxiety in the
Elderly
DOI: 10.5742/MEWFM.2017.93059
[pdf
version]
Somayeh Barekati, Bahman Bahmani, Maede Naghiyaaee,
Mahgam Afrasiabi, Roya Marsa
Post-mortem
Distribution of Morphine in Cadavers Body Fluids
DOI: 10.5742/MEWFM.2017.93060
[pdf
version]
Ramin Elmi, Mitra Akbari, Jaber Gharehdaghi,
Ardeshir Sheikhazadi, Saeed Padidar, Shirin
Elmi
Application
of Social Networks to Support Students' Language
Learning Skills in Blended Approach
DOI: 10.5742/MEWFM.2017.93061
[pdf
version]
Fatemeh Jafarkhani, Zahra Jamebozorg, Maryam
Brahman
The
Relationship between Chronic Pain and Obesity:
The Mediating Role of Anxiety
DOI: 10.5742/MEWFM.2017.93062
[pdf
version]
Leila Shateri, Hamid Shamsipour, Zahra Hoshyari,
Elnaz Mousavi, Leila Saleck, Faezeh Ojagh
Implementation
status of moral codes among nurses
DOI: 10.5742/MEWFM.2017.93063
[pdf
version]
Maryam Ban, Hojat Zareh Houshyari Khah, Marzieh
Ghassemi, Sajedeh Mousaviasl, Mohammad Khavasi,
Narjes Asadi, Mohammad Amin Harizavi, Saeedeh
Elhami
The comparison
of quality of life, self-efficacy and resiliency
in infertile and fertile women
DOI: 10.5742/MEWFM.2017.93064
[pdf version]
Mahya Shamsi Sani, Mohammadreza Tamannaeifar
Brain MRI Findings in Children (2-4 years old)
with Autism
DOI: 10.5742/MEWFM.2017.93055
[pdf
version]
Mohammad Hasan Mohammadi, Farah Ashraf Zadeh,
Javad Akhondian, Maryam Hojjati,
Mehdi Momennezhad
Reviews
TECTA gene function and hearing: a review
DOI: 10.5742/MEWFM.2017.93065
[pdf version]
Morteza Hashemzadeh-Chaleshtori, Fahimeh Moradi,
Raziyeh Karami-Eshkaftaki,
Samira Asgharzade
Mandibular
canal & its incisive branch: A CBCT study
DOI: 10.5742/MEWFM.2017.93066
[pdf
version]
Sina Haghanifar, Ehsan Moudi, Ali Bijani, Somayyehsadat
Lavasani, Ahmadreza Lameh
The
role of Astronomy education in daily life
DOI: 10.5742/MEWFM.2017.93067
[pdf
version]
Ashrafoalsadat Shekarbaghani
Human brain
functional connectivity in resting-state fMRI
data across the range of weeks
DOI: 10.5742/MEWFM.2017.93068
[pdf version]
Nasrin Borumandnia, Hamid Alavi Majd, Farid
Zayeri, Ahmad Reza Baghestani,
Mohammad Tabatabaee, Fariborz Faegh
International Health Affairs
A
brief review of the components of national strategies
for suicide prevention suggested by the World
Health Organization
DOI: 10.5742/MEWFM.2017.93069
[pdf
version]
Mohsen Rezaeian
Education and Training
Evaluating
the Process of Recruiting Faculty Members in
Universities and Higher Education and Research
Institutes Affiliated to Ministry of Health
and Medical Education in Iran
DOI: 10.5742/MEWFM.2017.93070
[pdf
version]
Abdolreza Gilavand
Comparison
of spiritual well-being and social health among
the students attending group and individual
religious rites
DOI: 10.5742/MEWFM.2017.93071
[pdf
version]
Masoud Nikfarjam, Saeid Heidari-Soureshjani,
Abolfazl Khoshdel, Parisa Asmand, Forouzan Ganji
A
Comparative Study of Motivation for Major Choices
between Nursing and Midwifery Students at Bushehr
University of Medical Sciences
DOI: 10.5742/MEWFM.2017.93072
[pdf
version]
Farzaneh Norouzi, Shahnaz Pouladi, Razieh Bagherzadeh
Clinical Research and Methods
Barriers
to the management of ventilator-associated pneumonia:
A qualitative study of critical care nurses'
experiences
DOI: 10.5742/MEWFM.2017.93073
[pdf version]
Fereshteh Rashnou, Tahereh Toulabi, Shirin Hasanvand,
Mohammad Javad Tarrahi
Clinical
Risk Index for Neonates II score for the prediction
of mortality risk in premature neonates with
very low birth weight
DOI: 10.5742/MEWFM.2017.93074
[pdf
version]
Azadeh Jafrasteh, Parastoo Baharvand, Fatemeh
Karami
Effect
of pre-colporrhaphic physiotherapy on the outcomes
of women with pelvic organ prolapse
DOI: 10.5742/MEWFM.2017.93075
[pdf
version]
Mahnaz Yavangi, Tahereh Mahmoodvand, Saeid Heidari-Soureshjani
The
effect of Hypertonic Dextrose injection on the
control of pains associated with knee osteoarthritis
DOI: 10.5742/MEWFM.2017.93076
[pdf
version]
Mahshid Ghasemi, Faranak Behnaz, Mohammadreza
Minator Sajjadi, Reza Zandi,
Masoud Hashemi
Evaluation
of Psycho-Social Factors Influential on Emotional
Divorce among Attendants to Social Emergency
Services
DOI: 10.5742/MEWFM.2017.93077
[pdf
version]
Farangis Soltanian
Models and Systems of Health Care
Organizational
Justice and Trust Perceptions: A Comparison
of Nurses in public and private hospitals
DOI: 10.5742/MEWFM.2017.93078
[pdf
version]
Mahboobeh Rajabi, Zahra Esmaeli Abdar, Leila
Agoush
Case series and Case reports
Evaluation
of Blood Levels of Leptin Hormone Before and
After the Treatment with Metformin
DOI: 10.5742/MEWFM.2017.93079
[pdf
version]
Elham Jafarpour
Etiology,
Epidemiologic Characteristics and Clinical Pattern
of Children with Febrile Convulsion Admitted
to Hospitals of Germi and Parsabad towns in
2016
DOI: 10.5742/MEWFM.2017.93080
[pdf
version]
Mehri SeyedJavadi, Roghayeh Naseri, Shohreh
Moshfeghi, Irandokht Allahyari, Vahid Izadi,
Raheleh Mohammadi,
Faculty development
The
comparison of the effect of two different teaching
methods of role-playing and video feedback on
learning Cardiopulmonary Resuscitation (CPR)
DOI: 10.5742/MEWFM.2017.93081
[pdf
version]
Yasamin Hacham Bachari, Leila Fahkarzadeh, Abdol
Ali Shariati
Office based family medicine
Effectiveness
of Group Counseling With Acceptance and Commitment
Therapy Approach on Couples' Marital Adjustment
DOI: 10.5742/MEWFM.2017.93082
[pdf
version]
Arash Ziapour, Fatmeh Mahmoodi, Fatemeh Dehghan,
Seyed Mehdi Hoseini Mehdi Abadi,
Edris Azami, Mohsen Rezaei
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| October 2017 -
Volume 15, Issue 8 |
|
|
Effect of pre-colporrhaphic
physiotherapy on the outcomes of women with
pelvic organ prolapse
Mahnaz Yavangi (1)
Tahereh Mahmoodvand (2)
Saeid Heidari-Soureshjani (3)
(1) Associate Professor of Obstetrics and Gynecology,
Endometrium and Endometriosis Research Center,
Hamadan University of Medical Sciences, Hamadan,
Iran
(2) Resident of Obstetrics and Gynecology, Endometrium
and Endometriosis Research Center, Hamadan University
of Medical Sciences, Hamadan, Iran.
(3) Modeling in Health Research Center, Shahrekord
University of Medical Sciences, Shahrekord,
Iran
Correspondence:
Tahereh Mahmoodvand,
Hamadan University of Medical Sciences,
Tel: +989121232813,
Email: Tahere.mahmoodvand@yahoo.com
|
Abstract
Background and Aim: Pelvic
organ prolapse (POP) is a common gynecological
problem with numerous complications. This
study was conducted to investigate the
effects of pre-colporrhaphic physiotherapy
on the outcomes of women candidates for
colporrhaphy with moderate to severe
POP.
Methods: This
randomized clinical trial was conducted
on women aged 20-59 years with moderate
to severe POP. The subjects were randomized
to two groups of 35 each: Controls (no
intervention) and cases (undergoing 10
sessions of physiotherapy). Three months
later, the two groups were examined for
outcomes and the outcomes were recorded
in a checklist. Data analysis was conducted
by SPSS 16.
Results:
There was no significant difference in
age, height, disease duration, and parity
between the two groups (p>0.05), but
the difference in weight was statistically
significant between the two groups (p<0.05).
The mean score on quality of life after
the intervention was 57.59±5.3
in the control group and 66±5.9
in the case group (p<0.001). There
was no significant difference in the rates
of pressure in pelvic organ, urinary incontinence,
and bowel movement disorder between the
two groups (p>0.05), but sexual satisfaction
was significantly higher and dyspareunia
was significantly lower in the case group
than the control group (p<0.05).
Conclusion:
Pre-colporrhaphic physiotherapy can improve
quality of life and sexual function in
candidates for colporrhaphy.
Key words:
Physiotherapy, Colporrhaphy, Pelvic organ
prolapse
|
Pelvic organ prolapse (POP) in women refers
to descended womb, bladder, small intestine,
and large intestine as well as post-hysteroscopy
vaginal cuff leading to uterine prolapse, vaginal
prolapse, or both. In this condition, the patient
may feel pain and pressure or prolapse of a
vaginal mass (1). As the elderly population
is expected to double by the year 2030, pelvic
organ prolapse will become higher prevalent
(2). Recently, the treatments that can return
the patients to normal life after POP surgery
have attracted attention (3). The quality of
life index is disrupted in the women with POP
(4) and therapeutic interventions such as a
surgery can help to improve this index (5).
However, colporrhaphy may lead to certain anatomical
outcomes. Dyspareunia and sexual dysfunction,
gastrointestinal diseases, and urinary incontinence
are some of common complications after colporrhaphy
(6-8). However, these complications may even
occur more or less before colporrhaphy (depending
on prolapse grade) and be intensified after
this surgery (9, 10). However, other therapeutic
methods are also recommend for preventing or
treating this complication. For example, Kegel
exercise and tension-free vaginal kits are considered
preventive and protective approaches before
POP surgery, but their therapeutic potential
remains controversial (11).
Physiotherapy has been frequently studied as
a procedure for strengthening the muscles. However,
a study showed that physiotherapy before and
after the surgery helped to improve the patients’
symptoms and quality of life (12). But, another
study reported that presurgical physiotherapy
did not cause improvement of bladder function
and prolapse symptoms (13). This study was conducted
to investigate the effects of pre-colporrhaphic
physiotherapy on the outcomes of the women with
moderate to severe POP candidates for colporrhaphy.
This randomized clinical trial was conducted
on the women aged 20-59 years with moderate
to severe POP referring to Hamedan Fatemiyeh
Hospital between 2011 and 2012. The subjects
were selected by census sampling and 70 women
with inclusion criteria were enrolled in the
study within this period. According to a previous
study (2), this sample size is adequate to conduct
the current study. The inclusion criteria were
POP diagnosed with reference to the indications
upon which specialists have agreed; lack of
response to conservative treatments in the past,
grades 2 and 3 accompanied by progression of
the symptoms, willingness to undergo colporrhaphy,
candidacy for colporrhaphy, and full consent
to participate in the study.
Diabetes, obesity, urinary tract infections,
genital tract infections, grades 1 and 4 cystocele,
uterine prolapse, forceps delivery and vacuum
extraction, and history of birth of macrosomic
infant, multiple pregnancy, and pelvic fascia
and muscle surgery were considered the exclusion
criteria. Then the subjects were randomized
to two groups. To conduct randomization, the
patients who referred on the even days of the
week were assigned to the case group and those
referring on the odd days of the week were assigned
to the control group. The case (intervention)
group underwent physiotherapy before colporrhaphy
and the control group underwent the colporrhaphy
without any intervention before conducting the
surgery. Physiotherapy of the patients in the
case group was conducted by a physiotherapist.
The physiotherapy intervention consisted of
a pelvic floor muscle (PFM) strength training,
accompanied by counseling on bladder and bowel.
Vaginal examination was conducted to ensure
correct PFM contraction, without any change
in respiration or recruitment of accessory muscles;
intensified attempt to reach maximum voluntary
contraction as correct technique was maintained;
performing of a series of 6–8 sec contractions,
with an interval between each contraction for
rest. This approach was done over 10 sessions,
3 times per day performed in a variety of positions,
progressing from lying to upright (13, 14).
The physiotherapy with similar technique and
assistance of a single physiotherapist who was
blind to the research purposes and details.
Then, a single gynecologist who was blind
to the study purposes and details conducted
colporrhaphy on all subjects in the Hamedan
Fatemiyeh Hospital with a similar technique.
Afterwards, the subjects of both groups received
similar recommendations and care. All subjects
were followed up for three months, and then
they were re-examined and their descriptions
were drawn again. The patients’ data on
complaints of urinary disorders (incontinence
and obstructive symptoms), complaints of fecal
excretion symptoms (incontinence and constipation),
sexual satisfaction, and the presence or absence
of dyspareunia were drawn and recorded in a
pre-designed checklist.
In addition, the overall score on quality of
life was calculated and recorded for both groups
using a standard questionnaire on patient quality
of life (SF-36). A study to translate and validate
this international standard scale demonstrated
that its Persian duplicate has adequate validity
and reliability for investigating health-related
quality of life (15).
To observe research ethics, the subjects provided
informed consent to participate in the study,
and the study protocol was approved (approval
no.: IRCT201201188772N1) in the Iranian Registry
of Clinical Trials. Data analysis was conducted
in SPSS (V. 16.0, III Chicago Inc.) by analytical
statistics t-test, chi-square test, and Fisher’s
exact test after qualitative data were encoded
and descriptive statistics were drawn.
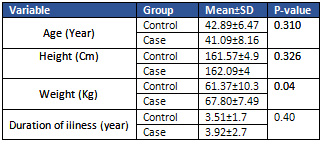
According
to
the
data
analysis,
there
was
no
significant
difference
in
age,
height,
and
the
disease
duration
between
the
two
groups
(p<0.05)
(Table
1).
Table
1:
Comparison
of
mean
age,
weight,
and
duration
of
disease
between
case
and
control
groups
In
the
case
group,
31
out
of
35
(88.6%)
patients
had
history
of
vaginal
delivery
and
the
rest
had
history
of
caesearian
section;
and
in
the
control
group,
27
out
of
35
(77.1%)
patients
had
history
of
vaginal
delivery
and
the
rest
had
history
of
caesearian
section,
without
any
significant
difference
between
the
two
groups
(p=0.11).
Regarding
parity,
in
the
case
group,
10
(28.6%)
subjects
had
one
child,
nine
(25.7%)
had
two
children,
and
two
(7.45%)
had
three
or
more
children;
and
in
the
control
group,
10
(28.6%)
subjects
had
one
child,
20
(57.1%)
had
two
children,
and
five
(14.3%)
had
three
or
more
children,
without
any
statistically
significant
difference
between
the
two
groups
(p=0.07).
The
mean
score
on
the
quality
of
life
after
the
intervention
was
57.59±5.3
in
the
control
group
and
66±5.9
in
the
case
group
(p<0.001).
There
was
no
significant
difference
in
the
rates
of
pressure
in
pelvic
organ,
urinary
incontinence,
and
bowel
movement
disorder
between
the
two
groups
(p>0.05),
but
sexual
satisfaction
was
significantly
higher
and
dyspareunia
was
significantly
lower
in
the
case
group
than
the
control
group
(p<0.05).
Click
here
for
Table
2:
Comparison
of
pressure
in
pelvic
organ,
urinary
incontinence,
and
bowel
movement
disorder
between
the
case
and
control
groups
The
present
study
was
conducted
with
the
aim
of
investigating
the
effect
of
pre-colporrhaphic
physiotherapy
on
treatment
outcomes
in
the
women
with
POP
candidate
for
colporrhaphy.
Results
demonstrated
that
the
mean
score
on
quality
of
life
was
significantly
higher
in
the
case
group
than
the
control
group.
Consistently,
Jarvis
et
al.
reported
that
undergoing
physiotherapy
before
surgery
for
prolapse
and
urinary
incontinence
could
contribute
to
improving
quality
of
life
and
decreasing
these
problems
in
women
(12).
In
two
other
studies,
pelvic
floor
physical
therapy
before
and
after
vaginal
repair
surgery,
caused
improvement
of
the
quality
of
life
in
case
group
(16,
17).
Surgeries
conducted
for
treating
POP
can
improve
the
quality
of
life
among
women
patients
because
they
contribute
to
decreasing
the
symptoms
or
improving
the
disease
complications.
Therefore,
undergoing
physiotherapy
and
doing
exercise,
particularly
pelvic
floor
muscle
exercises,
exerts
synergistic
effect
in
improving
the
quality
of
life
of
patients
through
reduction
of
physiological
and
anatomical
disorders
(5).
In
our
study,
although
the
number
of
cases
presenting
with
the
symptoms
of
severe
pressure
in
pelvic
organ,
urinary
incontinence,
and
bowel
movement
disorders
decreased
in
the
control
group,
the
difference
between
the
two
groups
was
not
statistically
significant.
In
contrast,
Frawley
et
al.
reported
that
physiotherapy
had
no
contribution
to
improving
prolapse
symptoms
and
urinary
incontinence
in
women
(13).
However,
other
studies
have
indicated
that
undergoing
physiotherapy
and
doing
pelvic
muscle
exercises
prior
and
after
the
surgeries
for
POP
can
be
effective
in
decreasing
urinary
incontinence
(12,
18-20),
improving
bowel
function
(20,
21),
and
relieving
feeling
of
pressure
and
pain
(22).
To
explain
this,
we
can
argue
that
the
surgery
itself
can
help
to
improve
the
symptoms,
which
can
relatively
neutralize
the
differences
between
the
two
groups.
Besides
that,
women’s
physiological
conditions
can
affect
the
results.
In
the
present
study,
the
rate
of
sexual
satisfaction
was
significantly
higher
and
dyspareunia
was
significantly
lower
in
the
case
group
than
the
control
group.
In
a
study
to
compare
the
effects
of
physiotherapy
accompanied
by
surgery
on
the
sexual
satisfaction
in
patients
with
pelvic
floor
disorders,
patients
were
assigned
to
two
groups
of
routine
treatment
and
physiotherapy.
After
an
8-week
intervention,
consistent
with
the
present
study,
the
symptoms
of
dyspareunia
and
orgasm
in
the
case
group
improved.
Therefore,
physiotherapy
can
be
considered
an
effective
therapy
for
pelvic
disorders
(23).
Notably,
colporrhaphy
itself
is
an
effective
treatment
for
improving
sexual
desire,
orgasm,
and
sexual
satisfaction
for
the
women
with
POP
(24).
Hagen
et
al’s
study
on
pelvic
floor
muscle
exercises
in
the
women
with
pelvic
fascia
prolapse,
showed
that
doing
these
exercises
for
6
months
could
improve
patients’
sexual
problems
(22).
A
study
reported
that
the
patients
who
underwent
pelvic
muscle
rehabilitation,
exhibited
improvement
in
certain
indices
such
as
orgasm
and
sexual
desire,
but
no
change
in
arousal
(25).
This
study
indicated
that
presurgical
physiotherapy
could
be
used
as
an
appropriate
approach
to
improve
the
quality
of
life
and
sexual
function
for
patients
with
POP
who
are
candidates
for
colporrhaphy.
It
is
recommended
to
investigate
individual
and
specific
physiotherapy
and
match
the
two
groups
of
the
study
by
physical
conditions
in
future
studies
as
well
as
to
conduct
longitudinal
studies.
1.
Jelovsek
JE,
Maher
C,
Barber
MD.
Pelvic
organ
prolapse.
Lancet.
2007;369(9566):1027-38.
2.
Chow
D,
Rodriguez
LV.
Epidemiology
and
prevalence
of
pelvic
organ
prolapse.
Curr
Opin
Urol.
2013;23(4):293-8.
3.
Choi
KH,
Hong
JY.
Management
of
Pelvic
Organ
Prolapse.
Korean
Journal
of
Urology.
2014;55(11):693-702.
4.
Fritel
X,
Varnoux
N,
Zins
M,
Breart
G,
Ringa
V.
Symptomatic
pelvic
organ
prolapse
at
midlife,
quality
of
life,
and
risk
factors.
Obstet
Gynecol.
2009;113(3):609-16.
5.
Doaee
M,
Moradi-Lakeh
M,
Nourmohammadi
A,
Razavi-Ratki
SK,
Nojomi
M.
Management
of
pelvic
organ
prolapse
and
quality
of
life:
a
systematic
review
and
meta-analysis.
Int
Urogynecol
J.
2014;25(2):153-63.
6.
Segal
S,
Arya
LA,
Smith
AL.
Functional
Outcomes
for
Incontinence
and
Prolapse
Surgery.
Current
bladder
dysfunction
reports.
2012;7(3):179-86.
7.
Ellington
DR,
Richter
HE.
Indications,
Contraindications,
and
Complications
of
Mesh
in
Surgical
Treatment
of
Pelvic
Organ
Prolapse.
Clinical
obstetrics
and
gynecology.
2013;56(2):276-88.
8.
Barber
MD,
Maher
C.
Epidemiology
and
outcome
assessment
of
pelvic
organ
prolapse.
Int
Urogynecol
J.
2013;24(11):1783-90.
9.
Tok
EC,
Yasa
O,
Ertunc
D,
Savas
A,
Durukan
H,
Kanik
A.
The
effect
of
pelvic
organ
prolapse
on
sexual
function
in
a
general
cohort
of
women.
J
Sex
Med.
2010;7(12):3957-62.
10.
Buchsbaum
GM.
Urinary
incontinence
and
pelvic
organ
prolapse.
Minerva
Urol
Nefrol.
2006;58(4):311-9.
11.
Giarenis
I,
Robinson
D.
Prevention
and
management
of
pelvic
organ
prolapse.
F1000Prime
Reports.
2014;6:77.
12.
Jarvis
SK,
Hallam
TK,
Lujic
S,
Abbott
JA,
Vancaillie
TG.
Peri-operative
physiotherapy
improves
outcomes
for
women
undergoing
incontinence
and
or
prolapse
surgery:
results
of
a
randomised
controlled
trial.
Aust
N
Z
J
Obstet
Gynaecol.
2005;45(4):300-3.
13.
Frawley
HC,
Phillips
BA,
Bo
K,
Galea
MP.
Physiotherapy
as
an
adjunct
to
prolapse
surgery:
an
assessor-blinded
randomized
controlled
trial.
Neurourol
Urodyn.
2010;29(5):719-25.
14.
Bø
K,
Hagen
RH,
Kvarstein
B,
Jørgensen
J,
Larsen
S,
Burgio
KL.
Pelvic
floor
muscle
exercise
for
the
treatment
of
female
stress
urinary
incontinence:
III.
Effects
of
two
different
degrees
of
pelvic
floor
muscle
exercises.
Neurourology
and
Urodynamics.
1990;9(5):489-502.
15.
Montazeri
A,
Gashtasebi
A,
Vahdaninia
M.
Translate,
determine
of
reliability
and
validity
of
Persian
questionnaire
of
SF36.
Payesh.
2005;5(1):49.
16.
Pauls
RN,
Crisp
CC,
Novicki
K,
Fellner
AN,
Kleeman
SD.
Impact
of
physical
therapy
on
quality
of
life
and
function
after
vaginal
reconstructive
surgery.
Female
Pelvic
Med
Reconstr
Surg.
2013;19(5):271-7.
17.
Pauls
RN,
Crisp
CC,
Novicki
K,
Fellner
AN,
Kleeman
SD.
Pelvic
floor
physical
therapy:
impact
on
quality
of
life
6
months
after
vaginal
reconstructive
surgery.
Female
Pelvic
Med
Reconstr
Surg.
2014;20(6):334-41.
18.
Rajkowska-Labon
E,
Bakua
S,
Kucharzewski
M,
liwiski
Z.
Efficacy
of
Physiotherapy
for
Urinary
Incontinence
following
Prostate
Cancer
Surgery.
BioMed
Research
International.
2014;2014:785263.
19.
Ghaderi
F,
Oskouei
AE.
Physiotherapy
for
Women
with
Stress
Urinary
Incontinence:
A
Review
Article.
Journal
of
Physical
Therapy
Science.
2014;26(9):1493-9.
20.
Hagen
S,
Stark
D,
Dougall
I.
A
survey
of
prolapse
practice
in
UK
women’s
health
physiotherapists:
what
has
changed
in
the
last
decade?
International
Urogynecology
Journal.
2016;27:579-85.
21.
Brækken
IH,
Majida
M,
Engh
ME,
Bø
K.
Can
pelvic
floor
muscle
training
reverse
pelvic
organ
prolapse
and
reduce
prolapse
symptoms?
An
assessor-blinded,
randomized,
controlled
trial.
American
Journal
of
Obstetrics
and
Gynecology.
2010;203(2):170.e1-.e7.
22.
Hagen
S,
Stark
D,
Glazener
C,
Dickson
S,
Barry
S,
Elders
A,
et
al.
Individualised
pelvic
floor
muscle
training
in
women
with
pelvic
organ
prolapse
(POPPY):
a
multicentre
randomised
controlled
trial.
The
Lancet.
2014;383(9919):796-806.
23.
Eftekhar
T,
Sohrabi
M,
Haghollahi
F,
Shariat
M,
Miri
E.
Comparison
effect
of
physiotherapy
with
surgery
on
sexual
function
in
patients
with
pelvic
floor
disorder:
A
randomized
clinical
trial.
Iranian
Journal
of
Reproductive
Medicine.
2014;12(1):7-14.
24.
Shahghaibi
S,
Faizi
S,
Gharibi
F.
Effect
of
colporrhaphy
on
the
Sexual
Dysfunction
of
women
with
pelvic
organ
prolapsed.
Pakistan
Journal
of
Medical
Sciences.
2013;29(1):157-60.
25.
Beji
NK,
Yalcin
O,
Erkan
HA.
The
effect
of
pelvic
floor
training
on
sexual
function
of
treated
patients.
International
Urogynecology
Journal.
2003;14(4):234-8.
|
|
.................................................................................................................

|
| |
|

