|
|
 |
Review Paper
........................................................
Education and Training
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| November 2014
- Volume 12 Issue 9 |
|
Prevalence
of Eye and Vision Abnormalities among a Sample
of Children up to five years old who visit Primary
Health Care Centers in Baghdad Alresafa
Zainab Mudhfer
Nasser (1)
Sanaa Jafar Hamodi Alkaisi (2)
Najah K.M. AL-Quriashi (3)
(1) M. B. Ch. B Specialist Family Physician
in the Arab Board of Family Medicine, Baghdad,
Iraq.
(2) M.B.Ch.B, F.I.B.M.S.\F.M Associated Prof.
in Family and Community Medicine ,Senior Specialist
Family Physician, Supervisor in the Residency
Program of Arab Board of Family Medicine, Member
in the Executive Committee of Iraqi Family Physicians
Society (IFPS) . Baghdad, Iraq.
(3) M.B.Ch.B., FICS.(Oph.),H.Dip.Laser(Oph.).
Assistant Professor and Senior Specialist Ophthalmologist
in Aljrahaat Teaching Hospital for Specialized
Surgeries / Medical city, Supervisor in the
Postgraduate Board Residency Program of Ophthalmology.
Baghdad, Iraq.
Correspondence:
Dr.Sanaa Jafar Hamodi Alkaisi, M.B.Ch.B, F.I.B.M.S.\F.M
Associate Prof and Senior Specialist Family
Physician, Supervisor in the Residency Program
of Arab Board of Family Medicine, member in
the Executive Committee of Iraqi Family Physicians
Society (IFPS) . Baghdad, Iraq.
Email: drsanaaalkaisi@yahoo.com
|
Abstract
Background : Vision
disorders are the fourth most common disability
of children and the leading cause of handicapping
conditions in childhood. Eye examination
and vision assessment are vital for the
detection of conditions that result in
blindness, signify serious systemic diseases
which may lead to problems with school
performance, or at worst, threaten the
child's life.
Objectives :
1.To
identify the prevalence of vision and
eye abnormalities in children up to five
years old attending two of primary health
care centers in Baghdad Al resafa.
2. To identify some risk factors associated
with vision and eye abnormalities in this
age group.
Subjects and methods: A
descriptive cross-sectional study was
conducted from November 2011 to March
2012 in two primary health care centers
in Baghdad Al resafa. The sampling was
a non-probability convenient sample of
(407) children, and all the eligible,
willing participants were subjected to
a self -structured close ended questionnaire
and were subjected to the following examinations
by the researcher alone (inspection of
all children's eyes and eyelids for any
abnormalities, red reflex examination,
corneal light reflex test, near fixation,
ocular motility test, cover test, visual
acuity test). Statistical Package for
Social Sciences version 18 was used for
data input and analysis.
Result: The
prevalence of eye and vision abnormalities
is 6.14% (95%CI 4.09% - 9.05%).The prevalence
of strabismus 4.4 %, abnormal visual acuity1.5%,
nystagmus 0.5%, congenital glaucoma 0.25%.
In this study sample the majority of children
with ocular abnormalities were from the
second and fifth years of life (p=0.008).
The sex was not significantly associated
with ocular abnormalities (p=0.512). Prematurity
was not significantly associated with
eye problems (p>0.05). Low birth weight
was significantly associated with eye
problems (p=0.003). Family history of
congenital glaucoma, eye deviation, wearing
glasses during childhood, all were significantly
associated with eye problems (p=0.001),
but family history of nystagmus and cataract
was not significant (p>0.05). Positive
history of prenatal infection was not
significantly associated with eye problems
(p=0.273). Needed oxygen therapy on birth
was significant (p=0.002). History of
seizure, cerebral palsy, and syndromes
all were not significant (p>0.05).
Conclusion: Strabismus
and abnormal visual acuity are the most
common abnormalities detected in this
study. The detected eye and vision abnormalities
were most commonly distributed in children
at the fifth and second year of life.
Key words: Prevalence,
eye and vision screening
|
Childhood blindness is a priority eye problem
in VISION 2020-The Right to Sight initiative.
[1]
Vision disorders are the fourth most common disability
of children and the leading cause of handicapping
conditions in childhood. [2]
Eye examination and vision assessment are vital
for the detection of conditions that result in
blindness, signify serious systemic diseases that
may lead to problems with school performance,
or at worst, threaten the child's life. [3,4]
Vision problems occur in 5% to 10% of all pre-schoolers
and include refractive error, strabismus, and
amblyopia. [5]
United States Preventive Services Task Force recommends
vision screening for all children at least once
between the ages of 3 and 5 years, to detect the
presence of amblyopia or its risk factors and
concludes that the current evidence is insufficient
to assess the balance of benefits and harms of
vision screening for children < three years
of age.[6]
Before adopting this screening in developing countries,
workload of such screening should be critically
reviewed to ensure its efficiency and sustainability.
[7]
In Iraq a new screening program for early detection
of eye and vision disorders in children from birth
-five years old was started in 2010.*
Aims of the study:
1.To identify the prevalence of vision and eye
abnormalities in children up to five years old
attending two of primary health care centers in
Baghdad Alresafa.
2. To identify some risk factors associated with
vision and eye abnormalities in this age group.
* Dr. Muna AttaAllah Khalefa Ali (head
of non communicable diseases unit at Iraqi Ministry
of Health).
1-Study Design :
A descriptive cross-sectional
study to identify the
prevalence of vision abnormalities
in children up to five
years old.
2-Time of the Study
This study was conducted
from the first of November
2011 to the first of March
2012
3-Place of the Study
This study was conducted
in two primary health
care centers in Baghdad
AL-Resafa; the selected
centers are:
1- Sylakh specialized
family Medicine primary
health care center.
2- AL-Mustansyria
specialized family Medicine
primary health care center.
4-Sampling Design
The sampling design was
a non-probability convenient
sample.
5-Sample size
The sample size was calculated
as (407) on a prevalence
of -5%-10% (as reported
in the USA) [3].
Sample size determination
used the formula:
N=P*Q*Z2/R2 N=0.08*0.92*(1.96)2/(0.05)2=113
N=Sample size, P=prevalence,
Q=1-P, Z=1.96, R=0.05.
6-Criteria of enrolment:
6.1 Inclusion criteria
The study population who
attended the selected
PHC centers for any complaint
was selected depending
on the following criteria:-
1) Age under five
years.
2) Children from
both sexes were included.
6.2 Exclusion criteria
1) Age above five
years old.
2) Subjects who
did not respond to screening
tests
Content of the questionnaire
After selection of the
eligible participants
(the parents), then clarification
of the purpose behind
the study, assuring high
confidentiality, and having
verbal consents were done.
And all the eligible willing
participants were subjected
to a self -structured
closed ended questionnaire
consisting of :
• Age at the time
of examination
• Gender
• Is there a family
history of vision problems
(e.g., cataracts, nystagmus,
congenital glaucoma, eye
crossing and/or needing
glasses In Young age?
• Was your child
exposed to any prenatal
infections (e.g. rubella,
toxoplasmosis, cytomegalovirus,
hepatitis)?
• Child weight at
birth?
• Gestational age
at birth?
• Has your child
had meningitis or encephalitis?
• Has your child
experienced some form
of head trauma?
• Does your child
have a seizure disorder?
• Does your child
have any difficulties
with his or her hearing,
Cerebral palsy, diagnosed
with a syndrome e.g. Down
syndrome?
All children were subjected
to the following examinations
by the researcher alone
using the same equipment
for all: [8]
1. Inspection:
Inspection of all
children's eyes and
eyelids for any abnormalities
like eye deviation,
limited eye movement,
involuntary jerky movement,
red eye, watery, cloudiness
of eye, drooping eyelid
or any other abnormality.
2. Red reflex examination:
The test was done for
all children and was
performed in a darkened
room (to maximize pupil
dilation). The direct
ophthalmoscope is focused
on each pupil individually
approximately 12- 18
inches away from the
eye, and then both eyes
are viewed simultaneously.
The red reflex seen
in each eye individually
should be bright reddish-yellow
(or light gray in darkly
pigmented, brown-eyed
patients) and identical
in both eyes. Dark spots
in the red reflex, blunted
dull red reflex, lack
of a red reflex, or
presence of a white
reflex are all indications
for referral. After
assessing each eye separately,
the eyes are viewed
together with the child
focusing on the ophthalmoscope
light (Bruckner test)
as before, any asymmetry
in red reflex colour,
brightness, or size
is an indication for
referral, because asymmetry
may indicate an amblyogenic
condition.
3. Corneal Light
Reflex Test:
All children older than
three months should
be examined holding
a penlight 12-13 inches
away from the child's
face directly in front
of the eyes. The child
needs to fixate either
on the penlight or an
object that may be held
near the light. The
examiner should observe
the reflection of the
penlight in the pupils
of both eyes. The reflection
should be centered or
equally centered slightly
toward the nose (nasal).
If the reflection is
symmetrical and centered
in both eyes it is normal.
If the reflection of
the penlight does not
appear to be in a centered
position in the pupil
of each eye it is considered
abnormal. Sensitivity
to light, rapid eye
movement, and poor fixation
observed during this
test are also reasons
for referral for further
evaluation.
4. Near Fixation:
All children older than
three months should
be examined. A 1-inch
object is to be placed
from (8-18) inches away
from the child's face
and observe whether
the child looks at the
object. If the child
does not look at the
object, it can be picked
up and shown to the
child. If the child
fixates on the object
(looks with sustained
gaze for 2-3 seconds)
it's a normal finding
but if the child cannot
fixate on the object
or maintain fixation
it's considered an abnormal
finding.
5. Ocular Motility
Test:
Smooth tracking skills
should be evident after
3 months of age.
Horizontal Tracking:
Position the object
or light about 12 inches
from the child's eyes.
Move the object to get
the child's attention
and let him or her look
at it for 2-3 seconds.
Slowly move the object
in an arc of 180 degrees
from one side to the
other and back to the
other side.
Vertical Tracking:
Position the object
about 12 inches in front
of the child's nose.
Move the object to get
the child's attention
and let him or her look
at it for 2-3 seconds.
Slowly move the object
up to several inches
above the child's head
and then down to several
inches below his or
her chin. If the tracking
is described as jerky
or segmented it is abnormal.
If both eyes maintain
their gaze on the oncoming
object at least 4-6
inches from the nose
it is normal.
6. Cover Test:
Start by 6 months age.
The target object (small
toy) may need to be
manipulated or changed
to maintain a young
child's attention. Position
the child sitting in
caregiver's lap or independently
in a chair. The room
should be quiet to reduce
unnecessary distraction.
The examiner sits across
from the child and aligns
his or her eyes with
the child's eyes. Hold
the target object about
12 inches away directly
in front of the child.
Get the child to fixate
on the object for 2-3seconds.
This can be checked
by moving the object
back and forth and watching
the child's eyes follow.
The child's right eye
should be covered with
the occluder, watching
the left eye for any
movement, the cover
should be left for 2-3
seconds then quickly
move the occluder across
the bridge of the nose
to cover the left eye,
watching the right eye
for any movement, waiting
2-3 seconds after the
cover is moved to permit
fixation of the now
uncovered eye, moving
the cover from the left
eye back to the right
eye, across the bridge
of the nose, watching
the left eye for any
movement then we allow
2-3 seconds for fixation.
Repeat procedure several
times to be assured
of observations. If
there is no redress
movement in either eye;
the child will pass
this screening indicator.
If there is redress
movement in either eye,
the child will fail
this indicator and should
be referred for further
evaluation.
7. Visual Acuity
(V.A) Test:
All children from 36
months old were examined,
using Snellen picture
chart. The examiner
shows the child the
pictures on the chart
up close and asks the
child to give a name
for each picture. The
child looks at the chart
which is placed 20 feet
(6 meters) from the
child. The child or
his or her parent occluding
one eye and the child
should be able to identify
at least 3 pictures
from 5 at each line
to pass that line. If
the child has a V.A
of 20 /40or 6 /12 his
or her V.A is considered
normal at that eye,
one eye should be evaluated
at a time. [8]
Data analysis:-
SPSS v.18 (Statistical
Package for Social Sciences
version 18) was used
for data input and analysis.
Continuous variables
were presented as mean
with its standard deviation
(SD) and discrete variables
presented as numbers
and percentages. Chi
square test for goodness
of fit was used to test
the significance of
observed distribution.
Those who did not undergo
a specific examination
or test were not included
in related analysis.
Chi square test for
independence and Fisher
exact test were used
as appropriate to test
the significance of
association between
observed findings. P
value used for all tests
was asymptotic and two
sided. Findings with
a P value less than
0.05 were considered
significant.
The total number of
children who were involved
in this study is 407;
the minimum age was
2 weeks and the maximum
age 59 months; the mean
of ages was 16.6 months;
standard deviation is
15.1.
The personal characteristics
for the study sample
according to presence
or absence of eye problems:
There is a significant
association between
age and having eye problems
with the majority of
eye problem cases aged
more than one year (p<0.001),
(Table 1).
Table 1: Personal characteristics
for the study sample
according to presence
or absence of eye problem
| |
positive
eye
problem N=25
|
100%
|
negative
eye problem N=382
|
100%
|
P
value
|
| Year
of Life |
|
|
|
|
|
| First |
3
|
12.0
|
180
|
47.1
|
|
| Second |
10
|
40.0
|
124
|
32.5
|
|
| Third |
1
|
4.0
|
35
|
9.2
|
<0.001
|
| Fourth |
0
|
0.0
|
21
|
5.5
|
|
| Fifth |
11
|
44.0
|
22
|
5.8
|
|
| Sex |
|
|
|
|
|
| Male
|
12
|
48.0
|
143
|
37.4
|
0.512
|
| Female |
13
|
52.0
|
239
|
62.6
|
|
| GA<
37 Week |
6
|
24.0
|
54
|
14.1
|
0.178
|
Birth
Weight
< 2.5 kg |
5
|
20.0
|
12
|
3.1
|
<0.001
|
There was no significant
association between
sex and having eye problem
(P=0.512). Prematurity
was not significantly
associated with eye
problems in the study
sample ( p=0.178). Low
birth weight was significantly
associated with eye
problems in the study
sample (p<0.001),
(Table 1 ).
History findings of
the study sample according
to presence or absence
of eye problems was
as follows: The number
of children with eye
problems was 25 and
the number of children
with no eye problems
was 382. Family history
of glaucoma, eye deviation,
wearing glasses during
childhood, all were
significantly associated
with eye problems in
the study sample (p<0.05)
for each, but family
history of nystagmus
was not significant
(p=0.06). There was
no family history of
cataract. Positive history
of prenatal infection
was not significantly
associated with eye
problems in the study
sample (p=0.57). Needed
oxygen therapy on birth
was significant (p=0.002).
History of seizure,
cerebral palsy, and
syndromes all were not
significant (p>0.05).
There were no cases
of hearing difficulty,
history of meningitis,
encephalitis or head
trauma, (Table 2 ).
Table 2: History
findings for the study
sample according to
presence or absence
of eye problems
| |
N
=25
|
100%
|
N=382
|
100%
|
P
value
|
| Family
history |
|
|
|
|
|
| Positive
for eye problems |
9
|
36.0
|
11
|
2.9
|
<0.001
|
| of
Cataract |
0
|
0.0
|
0
|
0.0
|
-
|
| of
Nystagmus |
1
|
4.0
|
0
|
0.0
|
0.061
|
| of
Glaucoma |
3
|
12.0
|
0
|
0.9
|
<0.001
|
| of
eye deviation |
2
|
4.0
|
3
|
0.8%
|
0.032
|
| Wearing
Glasses during childhood |
3
|
12.0
|
10
|
2.6
|
0.039
|
| Positive
History of Prenatal
Infection |
1
|
4.0
|
4
|
0.1
|
0.273
|
| History
of Needed Oxygen
Therapy on Birth |
4
|
16.0
|
2
|
0.5
|
0.002
|
| History
of Meningitis or
Encephalitis |
0
|
0.0
|
0
|
0.0
|
-
|
| History
of Head Trauma |
0
|
0.0
|
0
|
0.0
|
-
|
| History
of Seizure |
1
|
4.0
|
0
|
0.0
|
0.061
|
| History
of Hearing Difficulty |
0
|
0.0
|
0
|
0.0
|
-
|
| History
of Cerebral Palsy |
1
|
4.0
|
0
|
0.0
|
0.061
|
| History
of Syndromes |
1
|
0.0
|
1
|
0.3
|
0.119
|
Inspection finding
for study sample. The
total number of inspection
abnormalities was 24
(5.9%), 3 (0.9%) children
had watery eye, 1 child
(0.2%) had cloudy eye,
18 (4.4%) had eye deviation,
2 (0.5%) children had
nystagmus; no child
had red eye, irritated
eye or drooping of eyelids,
(Table 3).
Table 3: Inspection
findings for study sample
| |
N
= 407
|
100.0%
|
| Red
Eye |
0
|
0.0
|
| Irritated
Eye |
0
|
0.0
|
| Watery
Eye |
3
|
0.9
|
| Cloudy
Eye |
1
|
0.2
|
| Eye
Deviation |
18
|
4.4
|
| Nystagmus |
2
|
0.5
|
| Drooping
of Eyelids |
0
|
0.0
|
| Total
No. of abnormalities |
24
|
5.9
|
Examination findings
of study sample was
24 (5.8) children having
abnormal finding by
inspection. 8 (2%) children
had abnormal red reflex,
17 (4.1%) had abnormal
corneal reflex, 4(1%)
children had abnormal
fixation test. 5 (1.2
%) children had abnormal
fixation and flow (horizontal).
4 children (1%) had
abnormal fixation and
flow (vertical). 17
(4.1%) had abnormal
cover test. 6 (1.4%)
had abnormal visual
acuity, (Table 4).
Table 4: Examination
findings for study sample
| |
N
= 407
|
100.0%
|
| Inspection |
|
|
| Normal |
383
|
94.1
|
| Abnormal |
24
|
5.8
|
| Red
Reflex |
|
|
| Normal |
399
|
98.0
|
| Abnormal
Red Reflex |
8
|
2.0
|
| Corneal
Reflex |
|
|
| Symmetrical |
256
|
62.9
|
| Not
Symmetrical |
17
|
4.1
|
| Not
done * |
134
|
32.1
|
| Fixation
test |
|
|
| Normal |
346
|
85.0
|
| Not
normal |
4
|
1.0
|
| Not
done * |
57
|
14.0
|
| Fixation
and Flow Horizontal
) |
|
|
| Smooth |
345
|
84.8
|
| Not
Smooth/segmented |
5
|
1.2
|
| Not
done * |
57
|
14.0
|
| Fixation
and Flow (Vertical) |
|
|
| Smooth |
346
|
85.0
|
| Not
Smooth/segmented |
4
|
1.0
|
| Not
done * |
57
|
14.0
|
| Cover
Test |
|
|
| Normal |
256
|
62.9
|
| Abnormal
Cover Test |
17
|
4.1
|
| Not
done * |
134
|
3212
|
| Visual
Acuity |
|
|
| Normal |
46
|
11.3
|
| Abnormal
Visual Acuity |
6
|
1.4
|
| Not
done * |
355
|
87.2
|
* children not included
in the test because of
their age
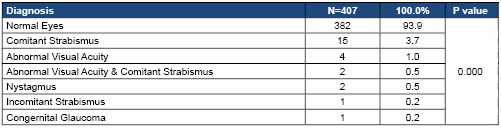
The distribution of
study sample according
to eye status was: 382
(39.9%) had normal eyes.15
(3.7%) had comitant
strabismus, 4(1%) had
abnormal visual acuity,
2 (0.5%) abnormal visual
acuity and comitant
strabismus. 2 (0.5%)
had nystagmus and 1
(0.2%) have incomitant
strabismus. 1 (0.2%)
had congenital glaucoma,
(Table 5).
Table 5: Distribution
of study sample according
to eye status.
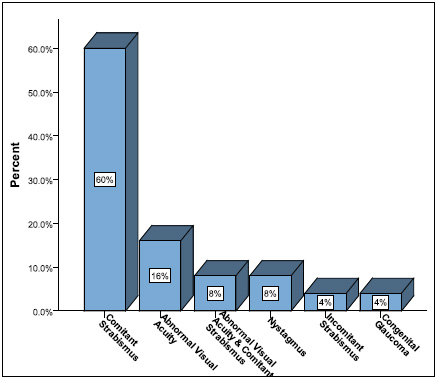
The distribution of
eye problems in children
with eye abnormalities,
were comitant strabismus
(60%), abnormal (VA.)
(16%), comitant strabismus+
abnormal (VA) is (8%),
nystagmus (8%), incomitant
strabismus (4%) and
congenital glaucoma
(4%), (Figure 1).
Figure 1: The distribution
of eye problems in children
with eye abnormalities
The prevalence of
eye and vision abnormalities
in the study sample
were:
The prevalence of all
eye abnormalities was
6.14% (95%CI 4.09% -
9.0.5%), the prevalence
of strabismus was 4.42
%, abnormal visual acuity
1.5%, nystagmus 0.5%
and congenital glaucoma
0.25% (Table 6).
Table 6: Shows the
prevalence of eye and
vision abnormalities
in the study sample
| Diagnosis |
Prevalence
|
95%CI
|
| Strabismus |
4.42
%
|
2.32-6.40
|
| Abnormal
Visual acuity |
1.50%
|
0.62-3.38
|
| Nystagmus |
0.50
%
|
0.09-1.97
|
| Congenital
gluacoma |
0.25
%
|
0.01-1.59
|
| Total |
6.14%
|
4.09
- 9.0.5
|
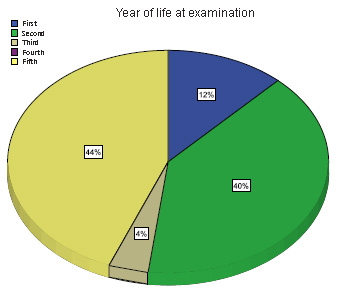
The distribution of
children with eye problems
according to the age
(year of life) at examination
shows that maximum distribution
is in the fifth (44%)
and second (40%) year
of life, no children
with eye problems were
found in the study sample
in the fourth year of
life, (Figure 2).
Figure 2: Distribution
of children with eye
problem according to
the age (year of life)
at examination
In
this
study,
the
prevalence
of
eye
and
vision
abnormalities
among
children
up
to
five
years
old
is
6.14%
(95%
CI
is
4.09%
-
9.05%)
and
this
goes
with
prevalence
of
American
Academy
of
Pediatrics
where
prevalence
of
vision
abnormalities
is
5%
to
10%.
[5]
The
prevalence
of
strabismus
is
4.4%
which
is
close
to
Rajiv
Khandekar
et
al's
study
in
Oman
and
Bardisi
et
al
in
Saudi
Arabia
where
the
prevalence
of
strabismus
was
2.9%
and
6%
respectively.
[7,
9]
This
is
also
similar
to
other
studies
in
the
USA
where
the
prevalence
was
4%.[10,
11]
The
prevalence
of
abnormal
visual
acuity
is
1.5%,
which
is
close
to
the
Al-Rowaily
study
in
Saudi
Arabia
which
was
4.5%.
[12]
The
prevalence
of
nystagmus
is
0.5%.
This
is
similar
to
Shirzadeh
et
al's
study
in
Iran
0.5
%
[13]
and
close
to
Rajiv
Khandekar
et
al's
study
in
Oman
which
was
1.2%.
[7]
The
prevalence
of
congenital
glaucoma
is
0.2%,
while
in
Zeidan
et
al's
study
in
Sudan
it
was
2.5
%,
[14]
and
according
to
the
American
Academy
of
Ophthalmology
it
was
0.01%
in
the
USA.
[15]
This
may
be
due
to
different
samples
size
among
these
studies.
The
distribution
of
children
with
ocular
abnormalities
in
regard
to
year
of
life
was
significant
in
that
the
majority
were
from
the
second
and
fifth
years
of
life
while
in
Rajiv
Khandekar
et
al's
study
the
distribution
of
children
with
ocular
abnormalities
was
significant
in
the
second
and
fourth
years
of
age.
[7]
This
may
be
due
to
the
larger
number
of
children
attending
primary
health
care
centers
during
the
fifth
year
of
life
according
to
the
immunization
program,
and
older
children
respond
better
than
those
who
are
younger
age
for
assessment
of
V.A.
by
Snellen
chart.
There
is
no
significant
association
between
sex
and
having
eye
problem
and
this
goes
with
Al-the
Rowaily
study
in
Saudi
Arabia.
[12]
This
study
shows
that
low
birth
weight
was
significantly
associated
with
eye
problems
and
this
goes
with
Rajiv
Khandekar
et
al's
study
in
Oman
and
Saw
et
al's
study
in
the
USA.
[7,16]
Prematurity
was
not
significantly
associated
with
eye
problems
and
this
goes
with
Rajiv
Khandekar
et
al's
study,
[7]
while
in
the
Dowdeswell
et
al
study
in
USA,
prematurity
was
associated
with
eye
and
vision
defect.
This
discrepancy
occurs
because
most
premature
children
in
this
study
were
born
after
the
32nd
week
of
gestation
while
in
the
Dowdeswell
et
al
study,
all
children
were
born
before
the
32nd
week
of
gestation.
[17]
Needed
oxygen
therapy
is
significantly
associated
with
eye
problems
in
this
study
and
this
goes
with
the
Saw
et
al
study
and
other
studies
in
the
USA.
[13,
8,
18]
Family
history
was
significantly
associated
with
eye
problems
in
this
study.
This
goes
with
publications
of
the
American
Academy
of
Ophthalmology
and
different
studies
in
the
USA.
[8,16,
18
,19]
Positive
history
of
prenatal
infection
was
not
significantly
associated
with
eye
problems
in
this
study.
This
is
because
the
majority
of
eye
problems
which
were
found
like
strabismus
and
abnormal
visual
acuity,
are
not
associated
with
prenatal
infection.
History
of
seizure,
cerebral
palsy,
and
syndromes
are
not
significantly
associated
with
eye
and
vision
problems
in
this
study,
while
in
Peter
Black
et
al's
study
in
England
and
Haugen
et
al's
study
in
Norway
there
was
significant
association.
[20,
21]
This
may
be
due
to
smaller
sample
size
in
this
study.
Vision
and
eye
screening
conducted
in
a
small
sample
of
children
up
to
five
years
old
in
this
study
enabled
us
to
detect
children
with
eye
problems
for
the
first
time
in
spite
of
having
well
established
and
accessible
eye
care
services
of
primary
and
secondary
levels
within
the
reach
of
this
community.
Strabismus
and
abnormal
visual
acuity
are
the
most
common
abnormalities
detected
in
this
study.
The
detected
eye
and
vision
abnormalities
are
most
commonly
distributed
in
children
at
the
fifth
and
second
year
of
life.
1-
Vision
screening
is
recommended,
but
validity
of
such
screening
should
be
established
before
recommending
eye
screening
on
a
larger
scale.
2-
Amblyopia
is
an
avoidable
vision
defect.
In
this
study,
risk
factors
for
amblyopia
like
abnormal
visual
acuity
and
strabismus
were
identified
and
further
studies
to
identify
the
prevalence
and
the
effect
of
early
detection
and
management
of
this
abnormality
is
recommended.
3-
Efforts
should
be
encouraged
to
increase
awareness
about
the
importance
of
early
vision
assessment
and
eye
examination
firstly
among
doctors,
especially
family
physicians,
general
practitioners
and
pediatricians
who
are
in
close
contact
with
children
during
this
critical
period
of
visual
development;
secondly
among
medical
staff
and
finally
among
parents
via
lectures,
meetings
and
media.
1.
Gilbert
C,
Foster
A.
Childhood
blindness
in
the
context
of
VISION
2020-The
right
to
sight.
Bull
World
Health
Organ.
2001;79:227-32.[PubMed]
2.
Ciner
EB,
Schmidt
PP,
Orel-Bixler
D,
et
al.
Vision
screening
of
preschool
children:
Evaluating
the
past,
looking
toward
the
future.
Optom.
Vis.
Sci.
1998;75:571-584
3.
American
Academy
of
Pediatrics,
Section
on
Ophthalmology.
Proposed
vision
screening
guidelines.
AAP
News.
1995;
11:25.
4.
American
Academy
of
Pediatrics,
Committee
on
Practice
and
Ambulatory
Medicine.
Recommendations
for
preventive
pediatric
health
care
Pediatrics.
1995;
96:373-3745.
5.
Donald
H.
Tingley.
Vision
Screening
Essentials.
Screening
Today
for
Eye
Disorders
in
the
Pediatric
Patient.
Pediatrics
in
Review.
February
2007;Vol.28
No.2
:54
6.
Chou
R,
Dana
T,
Bougatsos
C.
Screening
for
visual
impairment
in
children
ages
1-5
years:
update
for
the
USPSTF.
Pediatrics
2011;127(2):e442-e479.
7.
Rajiv
Khandekar,
Saleh
Al
Harby,
and
Ali
Jaffer
Mohammed.
Eye
and
vision
defects
in
under-five-year-old
children
in
Oman.
A
public
health:
intervention
study.
Oman
J
Ophthalmology.
2010
Jan-Apr;
3(1):
13-17
8.
Tanni
L.
Anthony,
J.C.
Greeley,
Susan
Larson,
et
al.
Visual
Screening
Guidelines:
Children
Birth
through
Five
Years.
COLORADO
DEPARTMENT
OF
EDUCATION.2005:5-6.
9.
Bardisi
WM,
Bin
Sadiq
BM.
Vision
screening
of
preschool
children
in
Jeddah,
Saudi
Arabia.
Saudi
Med
J.
2002
Apr;
23(4):445-9.
10.
Donnelly
UM,
Stewart
NM,
Hollinger
M.
Prevalence
and
outcomes
of
childhood
visual
disorders.
Ophthalmic
Epidemiol
2005;12:243-50
11.
National
Advisory
Eye
Council.
Vision
Research:
A
National
Plan.
Report
of
the
Strabismus
Amblyopia,
and
Visual
Processing
Panel,
Vol
2,
Part
5.
Bethesda:
US
DHHS,
NIH
Publ
No.
83.2001,2475
12.
Mohammad
A.
Al-Rowaily.
Prevalence
of
refractive
errors
among
pre-school
children
at
King
Abdulaziz
Medical
City,
Riyadh,
Saudi
Arabia.
Saudi
Journal
of
Ophthalmology.,
April
2010;
24,
Issue
2
,
Pages
45-48.
13.
Shirzadeh
E.,
Bolourian
A.A.,
Mohamadi
Nikpoor
M.,
Bemani
Naeini
M.
A
Survey
of
Impaired
Vision
and
the
Common
Etiology
in
the
Rural
Population
of
Sabzevar,
Iran.
Journal
of
Medical
Sciences
Research;
2007:
19-22
14.
Zeidan
Z,
Hashim
K,
Muhit
MA,
Gilbert
C.
Prevalence
and
causes
of
childhood
blindness
in
camps
for
displaced
persons
in
Khartoum:
results
of
a
household
survey.
East
Mediterr
Health
J.
2007;
13(3):
580-5.
15.
American
Academy
of
Ophthalmology
Basic
and
Clinical
Science
Course
Subcommittee.
Basic
and
Clinical
Science
Course.
Glaucoma:
Section
10,
2007-2008.
San
Francisco,
CA:
American
Academy
of
Ophthalmology;
2007:
Chapter
6
16.
Seang-Mei
Saw,
Joanne
Katz,
Oliver
D.
Schein
,et
al.
Epidemiol
Rev
Vol.
18,
No.
2,
1996:177-180.
17.Dowdeswell
HJ,
Slater
AM,
Broomhall
J,
Tripp
J.
Visual
deficits
in
children
born
at
less
than
32
weeks'
gestation
with
and
without
major
ocular
pathology
and
cerebral
damage.
Br
J
Ophthalmol.
1995
May;79(5):447-52.
18.
Linda
M.
Christmann,
Patrick
J.
Drost,
Sid
Mandelbaum.
American
Academy
of
Ophthalmology
Pediatric,
Ophthalmology/Strabismus
Panel.
Preferred
Practice
Pattern®
Guidelines.
Pediatric
Eye
Evaluations.
San
Francisco,
CA:
American
Academy
of
Ophthalmology;
2007.
Available
at:
http://www.aao.org/ppp.
19.
Lisa
A.
Jones-Jordan,
Loraine
T.
Sinnott,
Ruth
E.
Manny,
et
al.
Investigative
Ophthalmology
&
Visual
Science,
January
2010,
Vol.
51,
No.
1:115-121.
20.
PETER
BLACK.
Visual
disorders
associated
with
cerebral
palsy.
British
Journal
of
Ophthalmology,
1982;
66:
46-52
21.Haugen
OH,
Høvding
G.
Refractive
development
in
children
with
Down's
syndrome:
a
population
based,
longitudinal
study.
Br
J
Ophthalmol.
2001
June;
85(6):
714-719.
|
|
.................................................................................................................

|
| |
|

