|
|
 |
Review Paper
........................................................
Education and Training
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| November 2014
- Volume 12 Issue 9 |
|
Management
of primary postpartum Hemorrhage inside Erbil
city: Iraq
Awring
Maroof Raof
Correspondence:
Awring Maroof Raof, MSc. PhD community Medicine,
Department of Community Medicine, College of
Medicine,
Erbil, Iraq
Email: awringmaroof62@yahoo.com
|
Abstract
Background: The proportions
of maternal deaths due to postpartum hemorrhage
vary considerably between developed and
developing countries; deaths from postpartum
hemorrhage are preventable. This study
was carried out to determine the effect
of place of birth on the risk of primary
postpartum hemorrhage and the effect of
mode of management of the third stage
of labor on severe primary postpartum
hemorrhage.
Methods: This is a retrospective study.
Data for this study was collected from
the Directorate of Health in Erbil city
and record review from Maternity Teaching
Hospital, Primary Health Care Labour room
and Private Hospital. The population comprised
all low risk women giving birth from 2012till
2014. The data entry and data analysis
was done by using Statistical Package
for Social Sciences (SPSS, version 21.0).
P value ? 0.05 was regarded statistically
significant.
Results: From the data of Directorate
of Health in Erbil city and record review
a total of 73,954 births in Maternity
Teaching Hospital, primary health care
center and Private Hospital and home,
32,420 (43.8%) women were at low-risk.
About 1.3 percent (428/32,420) of those
low-risk women experienced a blood loss
greater than 1,000 mL. In this low-risk
cohort of women, those women receiving
active management of third stage of labor
had twice the risk of blood loss greater
than 1,000 mL compared with those undergoing
physiological management of third stage
of labor (RR: 2.12, 95% CI: 1.32-3.21).
Conclusion: The result of this study
showed that severe primary postpartum
hemorrhage was experienced by 1.32 percent
of low-risk women inside Erbil city. Place
of birth was not associated with increasing
the risk of severe postpartum hemorrhage
but active management of third stage of
labour increased the risk by twofold.
This study is welcoming and provides well-reasoned
scientific arguments in promoting third
stage labour care for women in developing
countries. Further studies tackling this
condition are necessary.
Key words: Postpartum hemorrhage,
risk factors, management options, cesarean
|
Postpartum haemorrhage (PPH) is the leading cause
of maternal mortality worldwide with a prevalence
rate of 6%; Africa has the highest prevalence
rate of about 10.5% (1). In Africa and Asia, PPH
accounts for more than 30% of all maternal deaths
(2).
The proportions of maternal deaths due to PPH
vary considerably between developed and developing
countries, so deaths from PPH are preventable
(2). Interventions to prevent PPH in developing
countries are therefore very important in the
global effort to achieve by 2015 the Millennium
Development Goal of reducing maternal mortality
ratio by three-quarters (from 1990 levels) (3).
The third stage of labour is defined as that time
extending from the birth of the baby until the
birth of the placenta (4).
The most common cause of PPH is uterine atony.
An evidence-based intervention for the prevention
of uterine atony is active management of the third
stage of labour, which has been adopted lately
in developing countries (5, 6). Research in this
field in developing countries is rare. Therefore,
both accurate knowledge about active management
of the third stage of labour (7) and its correct
use remain low in developing countries (8, 9).
In developing countries, health systems face difficulties
that delay the delivery of emergency obstetric
care, which is very important for saving the lives
of women who develop PPH. The high prevalence
of anemia in women in developing countries, complicates
PPH. Prevention of PPH through greater use of
active management of the third stage of labour
will reduce maternal mortality (10). Approximately
65% of deliveries in our region are supervised
by a skilled health-care provider. Developing
countries needs evidence-based interventions to
reduce PPH rates in deliveries not attended by
skilled providers (11).
Primary postpartum hemorrhage is often defined
as a blood loss of over 500 mL during or within
the first 24 hours of birth (12). The average
blood loss delivery has been estimated at 500ml
and this amount of blood loss is not tolerated
by women in developing countries. They enter labour
in poor health and they are usually hemo dynamically
compromised(13).The primary method which is available
for practitioners in clinical situations is visual
estimation of the blood loss. It provides the
bases for clinical management. This study depends
on this method which usually results in underestimation
of blood loss. The estimate of blood loss in the
current study is assumed to be consistent in different
birth settings with different management of third
stage being used (14).
Two approaches to the management of the third
stage of labor are used: active, which means using
a uterotonic drug, or physiological, not using
a uterotonic drug (15).
To our knowledge this is the first study concerning
postpartum hemorrhage and its management inside
Erbil city. This study was carried out to determine
the effect of place of birth on the risk of primary
postpartum hemorrhage and the effect of mode of
management of the third stage of labor on severe
primary postpartum hemorrhage.
This is a cross sectional,
retrospective study. Data
for this study were collected
from Directorate of Health
in Erbil city and record
review from Maternity
Teaching Hospital, Primary
Health Care Labour room
and Private Hospital.
The Maternity Teaching
Hospital is the only public
Hospital in Erbil city.
It provides delivery care
services, medical termination
of pregnancy, Caesarean
section and blood transfusion.
It is largely equipped
to cope with emergencies,
and services are available
24 hours a day. The hospital
serves the whole population
of Erbil governorate.
The population comprised
all low risk women giving
birth from 1st Jan 2012
till 1st Jan 2014. Information
collected was about demographic,
medical history, type
of birth, and place of
birth. Exclusion criteria
were: women with previous
cesarean section, elective
cesarean section stillbirth,
previous postpartum hemorrhage(>1,000
mL), pregnancy-induced
hypertension, gestational
diabetes, essential hypertension,
diabetes, thyroid disease,
heart disease, asthma,
hematological disorder,
neurological disorder,
renal/urinary tract disorder,
multiple birth, fetal
death, women who presented
in labor before 36 completed
weeks' gestation or after
42 completed weeks' gestation,
induced labor, shoulder
presentation or breech,
and transverse lie. Place
of birth was defined as
home, primary unit, secondary
hospital, or private hospital.
In active management of
labour the uterotonic
drug of choice is given
as soon as possible after
birth of the baby's anterior
shoulder; then the cord
is clamped and cut after
birth of the baby; the
placenta is born after
separation by maternal
effort or controlled cord
traction, while in the
physiological management
of third stage of labour
no prophylactic uterotonic
drug is given, without
controlled cord traction.
Clamping and cutting of
the cord is delayed for
several minutes or until
the placenta is expelled.
If the cord is clamped
and cut before expulsion
of the placenta, the placental
end is to be drained.
Keeping the women warm
and put the baby to the
breast. When signs of
placental separation occur,
the mother's position
may be changed to deliver
the placenta by gravity
force then using traction
force gently to guide
the placenta.
According to the records,
women were categorized
into four groups: active
management, active management
with treatment, physiological,
and physiological with
treatment. In the current
study active management
and active management
with treatment were put
together under the group
"active management"
and physiological, and
physiological management
with treatment were considered
together under the second
group named "physiological
third stage." Treatment
refers to the administration
of uterotonic drug (16).
The study was approved
by the scientific committee
of the department of Community
Medicine and the ethical
committee of College of
Medicine at Hawler Medical
University.
Data analysis:
The data entry and data
analysis was done by using
Statistical Package for
Social Sciences (SPSS,
version 20.0). P value
? 0.05 was regarded statistically
significant. Statistical
tests included Chi-square
test to compare between
the proportions of different
"characteristics"
among the groups. Analysis
was done with multinomial
logistic regression after
controlling for maternal
age(< 35 or > 35years),
parity (nullipara or multipara),
ethnic group (Kurdish,
Arab, Turkman, Aserian,
others), augmentation
of labor done or not,
length of labor, mode
of birth (vaginal, assisted
vaginal, emergency cesarean
section), episiotomy done
or not, and newborn birth
weight (less or greater
than 4,000 g).
From the data of Directorate
of Health in Erbil city
and record review of
a total of 73,954 births
in Maternity Teaching
Hospital, primary health
care center and Private
Hospital and home, 32,420
(43.8%) women were at
low-risk. Of this group,
11.3 percent gave birth
at home, 17.7 percent
in a primary unit, 45.5
percent in a secondary-level
hospital, and 25.4 percent
gave birth in a private
hospital.
Table 1 illustrates
the mean age, parity,
and length of labor,
vaginal births, and
management of third
stage of labor by place
of birth. The study
shows that each group
was different significantly
in respect to these
characteristics. Those
women who gave birth
at home or in primary
units have a higher
mean age and parity
and shorter mean length
of labor. The home and
primary unit women showed
a greater percentage
of unassisted vaginal
delivery with lower
percentage of active
management of third
stage of labor than
the secondary and private
hospital groups.
Table 1: Distribution
of the studied sample
according to mean age,
mean parity, mean length
of labour, vaginal birth,
Cesarean section, active
management of third
stage of labour by place
of birth
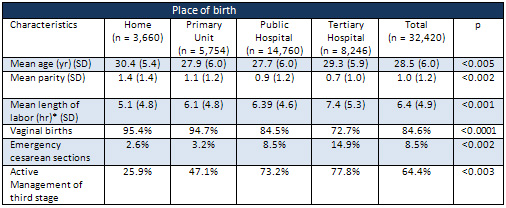
Table 2 shows women
who lost blood greater
than 1,000 mL and mode
of third stage management
for each place of birth.
About 1.3 percent (428/32,420)
of those low-risk women
experienced a blood
loss greater than 1,000
mL. Women who gave birth
at home and in primary
health care center had
the lowest proportion(25.9%
and 47.1%) among those
who received active
management of the third
stage of labor, and
the lowest proportion
of blood loss greater
than 1,000 mL (1.03%
and 1.11%),while the
secondary and private
hospital groups had
the highest proportion
(73.2% and 77.8%) of
women receiving active
management of the third
stage of labor and the
highest proportion(1.30%
and 1.62%) of women
with a blood loss greater
than 1,000 mL.
A larger number of women
(1.11%) with blood loss
more than 1,000 ml were
in the active management
groups for all birth
places.
Table 2: Distribution
of severe postpartum
hemorrhage cases by
third stage management
and birth place*
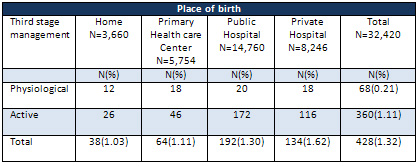
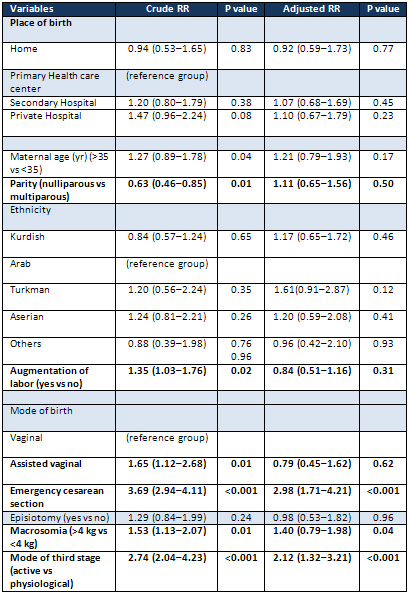
Table 3 shows the relative
risk of blood loss greater
than 1,000 mL by place
of birth. It was 0.92(95%
CI: 0.59-1.73) for the
home birth group, 1.07(95%CI:
0.68-1.69) for the secondary
hospital group, and
1.10 (95% CI: 0.67-1.79)
for the private hospital
group, although the
differences were not
statistically significant.
There was no statistically
significant difference
between the four groups
in respect to place
of birth and risk of
severe postpartum hemorrhage
(loss greater than 1,000
mL).
In this low-risk cohort
of women, those women
receiving active management
of third stage of labor
had twice the risk of
blood loss greater than
1,000 mL compared with
those undergoing physiological
management of third
stage of labor (RR:
2.12, 95% CI: 1.32-3.21).
In addition, women experiencing
an emergency cesarean
section had an almost
two fold risk of blood
loss greater than 1,000
mL than women who had
normal vaginal birth.
Table 3: Distribution
of studied sample according
to variables and risk
of severe hemorrhage
In the current study
1.32% of women experienced
severe postpartum hemorrhage,
which is lower than
that reported in other
low-risk populations.
According to WHO PPH
affects approximately
2% of all women who
give birth.
WHO defines postpartum
hemorrhage (PPH) as
a blood loss of 500
ml or more within 24
hours after birth, while
severe PPH is defined
as a blood loss of 1000
ml or more within the
same time frame. The
reporting of postpartum
hemorrhage in our region
uses the WHO definition
which did not distinguish
between high and low
risk women (17).
Women who make the choice
to give birth at home
or in a birth centre
do so because they want
to give birth naturally,
in their own way at
their own time; this
includes the way they
want to experience the
third stage of labour.
The study which was
conducted among low
risk American women
(18) reported that 2.6
percent of the women
had a blood loss which
was greater than 1,000
mL. A randomized controlled
trial in the UK(19)
showed that 2 percent
(90/3,436) of the women
had a blood loss which
was greater than 1,000
mL. The Australia Study,
(20) demonstrated that
2.3 percent of the women
who gave birth vaginally
had a blood loss of
1,000 mL or more but
which was less than
1,500 mL and that 1.6
percent had a blood
loss of 1,500 mL or
more. A study in India
showed that, 40.3% of
the women had a blood
loss which was between
500-700 ml, 27.4% had
a blood loss which was
between 700-1000 ml
and 32.2% had a blood
loss of more than 1000ml
(21).
A recent Swedish randomized
controlled trial (22)
on low-risk women which
compared the physiological
third stage with the
active management, reported
a high rate of severe
postpartum hemorrhages
13.5 percent overall.
The high rate of PPH
in the previous studies
is due to high risk
cohort. The explanation
for the low rate of
PPH in the current study:
is due to low risk women,
under-reporting, or
due to different skills
of midwives in the different
study settings and finally
could be due to the
use of visual method
for assessment of hemorrhage
which is a subjective
one and results in underestimation
of the amount lost especially
in a busy labour room.
In the current study
the lowest proportion
of women who received
active management was
among home and primary
health center groups
(25% and 47% respectively).
The explanation for
that could be due to
the fact that birth
is a normal process
and no need for interference
that is why those women
seek care from the primary
health care center and
some even prefer delivery
at home (23), while
the hospital group had
higher rate of active
management even without
risk of postpartum hemorrhage.
In the current study,
those having active
management of the third
stage of labor had two
times the risk of severe
postpartum hemorrhage
than those having a
physiological third
stage of labor. This
finding was in contrast
with the findings from
randomized controlled
trials that were conducted
in the UK (24, 25).
One of the limitations
of this study is a retrospective
study so it's subjected
to selection bias. The
higher rate of severe
postpartum hemorrhage
in the active management
group found in our study
could be explained by
under-reporting of postpartum
hemorrhage in the physiological
third stage group. It
could also reflect the
fact that the third
stage of labor was already
complete when it was
managed. Caregivers
may not be as skilled
as they should be in
monitoring blood loss
and uterine contractility
when physiological management
was used. It is clear,
however, that in developing
countries there is no
good evidence which
informs decision making
for women at low risk
of hemorrhage, in low-resource
settings and with caregivers
who are not confident
in active and physiological
management of third
stage of labor (26).
The results of this
study suggest that women
at low risk of hemorrhage
with caregivers who
are confident in the
physiological management
of third stage of labor
may have less risk of
severe postpartum hemorrhage
than their counterparts
experiencing active
management of the third
stage of labor. Another
limitation of this study
is that the deliveries
are not representative
of all facility-based
deliveries in Erbil
governorate so the result
can't be generalized.
Further prospective
research is needed to
substantiate these results
and provide stronger
evidence to inform decision
making.
The result of this study
showed that severe primary
postpartum hemorrhage
was experienced by 1.32
percent of low-risk women
inside Erbil city. Place
of birth was not associated
with increasing the risk
of severe postpartum hemorrhage
but active management
of third stage of labour
increased the risk by
twofold.
The finding of this study
is in contrast to other
studies from randomized
controlled trials on this
clinical issue. Blood
loss in labor or the postpartum
period exposes women to
additional risks and also
increases financial burden
on the health service.
It is important to support
women and encourage physiological
birth if it's appropriate.
It should also be emphasized
that the reduction of
blood loss has a much
greater impact on women's
health in our region.
A randomized controlled
trial in this field is
recommended. We acknowledge
that this study is welcoming
and provides well-reasoned
scientific arguments in
promoting third stage
labour care for women
in developing countries.
1-Carroli
G,
Cuesta
C,
Abalos
E,
Gulmezoglu
AM.
Epidemiology
of
postpartum
haemorrhage:
a
systematic
review.
Best
Pract
Res
Clin
Obstet
Gynaecol
2008;22:999-1012.
2-Khan
KS,
Wojdyla
D,
Say
L,
Gulmezoglu
AM,
Van
Look
PFA.
WHO
analysis
of
causes
of
maternal
death:
a
systematic
review.
The
Lancet
2006;367:1066-1074.
3-United
Nations.
Millennium
Development
Goals.
New
York:
United
Nations;
2000.
Available
at:
http://www.un.org/millenniumgoals.
4-
Cunningham
F,
Leveno
K,
Bloom
S,
Hauth
J,
Gilstrap
L,
Wenstrom
K,
editors.
Williams
obstetrics.
22nd
ed.
New
York:
McGraw-Hill;2005.
5-Lalonde
A,
Daviss
BA,
Acosta
A,
Herschderfer
K.
Postpartum
haemorrhage
today:
ICM/FIGO
initiative
2004-2006.
Int
J
Gynaecol
Obstet
2006;94:243-253.
6-International
Confederation
of
Midwives;
International
Federation
of
Obstetrics
and
Gynaecology.
Prevention
and
treatment
of
post-partum
haemorrhage.
New
advances
for
low
resource
settings.
.
Int
J
Gynaecol
Obstet
2007;97:160
-163.
7-Oladapo
OT,
Akinola
OI,
Fawole
AO,
Adeyemi
AS,
Adegbola
O,
Loto
OM,
Fabamwo
AO,
Alao
MO,
Sotunsa
JO.
Active
management
of
third
stage
of
labour:
evidence
versus
practice.
Acta
Obstetricia
et
Gynecologica
2009;88:1252-1260.
8-
Stanton
C,
Armbruster
D,
Knight
R,
Ariawan
I,
Gbangbade
S,
Getachew
A,
Portillo
JA,
Jarquin
D,
Marin
F,
Mfinanga
S,
Vallecillo
J,
Johnson
H,
Sintasath
D.
Use
of
active
management
of
the
third
stage
of
labour
in
seven
developing
countries.
Bull
World
Health
Org
2009;87:207-215
.
9-
Festin
MR,
Lumbiganon
P,
Tolosa
JE,
Finney
KA,
Ba-Thike
K,
Chipato
T,
Gaitán
H,
Xu
L,
Limpongsanurak
S,
Mittal
S,
Peedicayil
A,
Pramono
N,
Purwar
M,
Shenoy
S,
Daly
S.
International
survey
on
variations
in
practice
of
the
management
of
third
stage
of
labour.
Bull
World
Health
Org
2003;
81:
286
-
291.
10-Karoshi
M,
Keith
L.
Challenges
in
managing
postpartum
hemorrhage
in
resource-poor
countries.
Clinic
Obstet
Gynecol
2009;52:285-298.
11-WHO.
Proportion
of
births
attended
by
a
skilled
health
worker
2008
updates.
Geneva:
World
Health
Organization;
2008.
12-World
Health
Organization.
WHO
Guidelines
for
Management
of
Postpartum
Haemorrhage
and
Retained
placenta
Geneva:WHO,2009.
13-
Coker
A,
Oliver
R.
Definitions
and
classifications.
In:
B-Lynch
C,
Keith
L,
Lalonde
AB,
Karoshi
M,
eds.
A
Textbook
of
Postpartum
Hemorrhage:
A
Comprehensive
Guide
to
Evaluation,
Management
and
Surgical
Intervention.
New
Delhi:
Jaypee
Brothers
Medical
Publishers,
2006:11-16.
14-Bose
P,
Regan
F,
Paterson-Brown
S.
Improving
the
accuracy
of
estimated
blood
loss
at
obstetric
hemorrhage
using
clinical
reconstruction.
Gen
obstet
2006,
113(8):919-924.http://onlinelibrary.wiley.com/doi/10.1111/j.1471-0528.2006.01018.x/full
15.Prendiville
WJP,
Elbourne
D,
McDonald
SJ.
Active
versus
expectant
management
in
the
third
stage
of
labour
[Cochrane
review].
Chichester:
The
Cochrane
Library;
2000.
http://apps.who.int/rhl/reviews/langs/CD000007.
16-World
Health
Organisation.
The
prevention
and
management
of
postpartum
haemorrhage.
WHO
report
of
technical
working
group
1990;
Report
No
WHO/MHC/90.7.
17-WHO
.WHO
recommendation
for
prevention
and
treatment
of
postpartum
hemorrhage.Geneva:2012.
18-Fahy
K.
Third
stage
of
labor
care
for
women
at
low
risk
of
postpartum
hemorrhage.
J
Midwifery
Women's
Health
2009;54
(5):380-386.
19-
Rogers
J,
Wood
J,
McCandlish
R,
Ayers
S,
Truesdale
A,
Elbourne
D.
Active
versus
expectant
management
of
the
third
stage
of
labour:
The
Hinchingbrooke
randomised
controlled
trial.
Lancet
1998;351(9104):693-699.
20-Thompson
J,
Baghurst
P,
Ellwood
D.
Benchmarking
Maternity
Care
2008-2009.
Canberra,
Australia:
Women's
Hospitals
Australasia,
2010.
21-Umashankar
KM,
Dharmavijaya
MN,
Sudha
R,
Sujatha
N
Datti,
Kavitha
G,
Laxmi.
Effect
of
a
Primary
Postpartum
Haemorrhage
on
the
"Near-Miss"
and
Mortality
at
a
Tertiary
Care
Hospital
in
Rural
Bangalore,
India.
Journal
of
Clinical
and
Diagnostic
Research.
2013,
7(6):
1114-1119
22-
Jangsten
E,
Mattsson
LÅ,
Lyckestam
I,
Hellström
AL,
Berg
M.
A.
comparison
of
active
management
and
expectant
management
of
the
third
stage
of
labour:
A
Swedish
randomised
controlled
trial.
Br
J
Obstet
Gynaecol.
2011;118(3):362-36.
23--
Davis
D,
Baddock
S,
Pairman
S,
Hunter
M,
Benn
C,
Wilson
D,
Dixon
L,
Herbison
P.Planned
place
of
birth
in
New
Zealand:
Does
it
affect
mode
of
birth
and
intervention
rates
among
low-risk
women?
Birth
2011;38(2):111-119.
24.
Begley
CM.
A
comparison
of
active
and
physiological
management
of
the
third
stage
of
labour.
Midwifery
1990;6:3-17
25.
Rogers
J,
Wood
J,
McCandlish
R,
Ayers
S,
Truesdale
A,
Elbourne
D.
Active
versus
expectant
management
of
the
third
stage
of
labour:
the
Hitchingbrooke
randomised
controlled
trial.
Lancet
1998;351:693-9
26-
International
Federation
of
Obstetrics
and
Gynecology,
Safe
motherhood
and
newborns
health.
Prevention
and
treatment
of
postpartum
hemorrhage
in
low
resource
setting.
Int
J
Gynaecol
Obstet
2012;117:108-118.
|
|
.................................................................................................................

|
| |
|

