|
|
 |
Review Paper
........................................................
Education and Training
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| November 2014
- Volume 12 Issue 9 |
|
Review:
Ebola haemorrhagic fever
Lesley
Pocock (1)
Mohsen Rezaeian
(2)
(1) Publisher, Middle East Journal of Family
Medicine,
Queensland, Australia
(2) PhD, Epidemiologist, Social Medicine Department
Occupational Environmental Research Center
Rafsanjan Medical School
Rafsanjan University of Medical Sciences
Rafsanjan-Iran
Correspondence:
Lesley Pocock
Publisher,
Middle East Journal of Family medicine,
Queensland, Australia
Email: lesleypocock@mediworld.com.au
|
Abstract
This
is a review paper, on the spread of Ebola
haemorrhagic fever (Ebola) on the African
continent and beyond, and provides guidelines
for its prevention, diagnosis and treatment,
for family doctors.
Key words: Ebola,
prevention, diagnosis, treatment
|
Ebola haemorrhagic fever (Ebola) was first
documented in Zaire (Democratic Republic of
the Congo) in 1976. The reported number of human
cases at the time was 318. Of those, 88% died.
The disease was spread by close personal contact
and by use of contaminated needles and syringes
in hospitals/clinics.
In the same year there were 284 cases in South
Sudan, where the disease was recorded as Sudan
fever. The disease was spread mainly through
close personal contact within hospitals. Many
medical care personnel were infected.
With few cases in the ensuing years it emerged
again in 1979, in South Sudan with 34 cases.
65% of the infected died.
1994 saw a major re-emergence in Gabon (52 cases,
31 deaths) and in 1995 there were 315 cases
in the Democratic Republic of the Congo (formerly
Zaire).
There was 1 death in Russia in 1996, the first
case out of Africa, and a further death in Russia
in 2004. 6 asymptomatic cases were found in
the Philippines in 2008.
2000-2001 saw a major outbreak in Uganda with
425 cases with a 53% death rate. Major outbreaks
also occurred in Gabon and the Republic of Congo
in the same year.
Varying levels of outbreaks have occurred since
that time.
2014 has seen major outbreaks in Guinea, Liberia,
and Sierra Leone, with local transmission of
Ebola in Spain, (2 cases) and the USA (2 cases).
Senegal has had cases of travel-associated transmission.
Currently there are 10,000 expected new cases
of Ebola in West Africa, every week. Unfortunately
the major outbreaks are in developing nations
with limited resources, with minimal foreign
aid or assistance to these countries being generated,
Ebola now threatens the global population. (1,4)
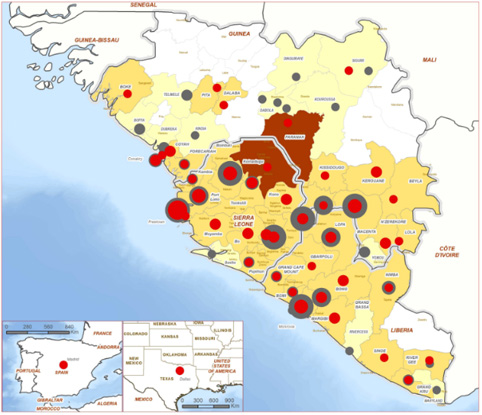
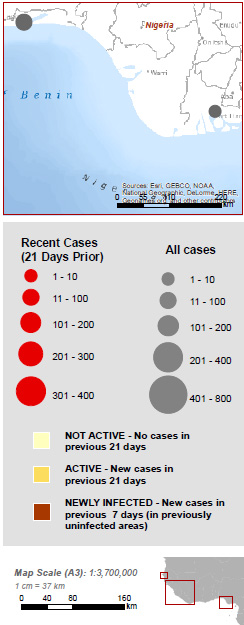
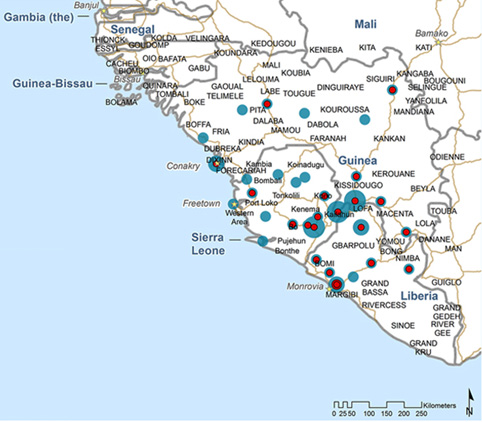
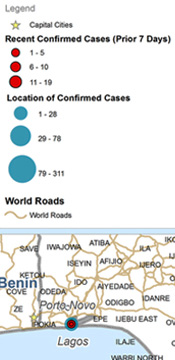
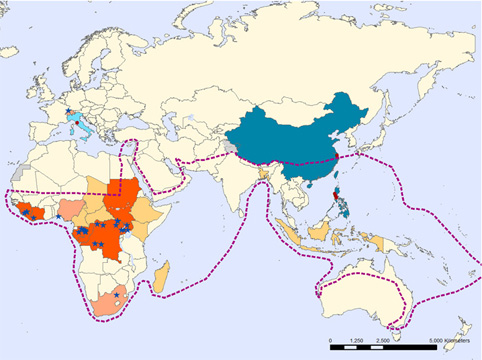
Ebola Outbreak Response Maps
WHO 2014
(Reproduced with permission from:
http://www.who.int/csr/disease/ebola/maps/en/
)
Map 1: Regional confirmed and probable cases
- 20 October 2014
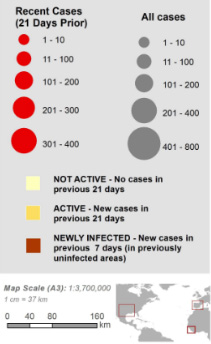
Map 2: Regional confirmed and probable cases
- 3 October 2014
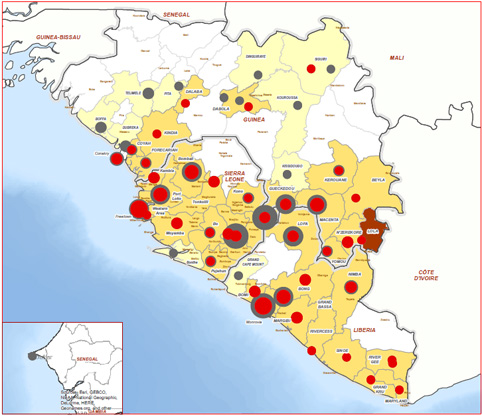
Map 3- Confirmed cases of Ebola – 7
August 2014
Map 4- Geographic distribution of Ebola
virus disease outbreaks in humans and animals
- 2014
Map 5 - Laboratories for Ebola virus diagnostic
- 10 April 2014

Ebola virus is one of
a group of zoonotic viruses
that can cause severe
disease in humans. Other
viruses that cause viral
haemorrhagic fever include
Lassa virus, Crimean-Congo
haemorrhagic fever virus,
Marburg virus, and emerging
viruses such as Lujo virus.
In previous outbreaks
2,387 cases have been
reported, with a case
fatality risk of 66.7%.(2)
Of the five species of
Ebola virus, three (Zaire,
Sudan and Bundibugyo)
have been associated with
significant human to human
transmission, with the
other two (Tai Forest
and Reston) associated
with limited or no human
disease.
The current outbreak has
been caused by a new emergence
of the Zaire species.(2)
Data from previous outbreaks
suggest Ebola is moderately
transmissible in the absence
of infection control,
even in resource limited
settings. Studies have
estimated the basic reproductive
ratio (R0) at 1.3 to 2.7
in different outbreaks
(2.3) meaning that in
a completely susceptible
population with no interventions
to reduce spread, each
infected case resulted
in secondary transmission
to an average of fewer
than three people.
Symptoms of Ebola include
• Fever
• Severe headache
• Muscle pain
• Weakness
• Diarrhoea
• Vomiting
• Abdominal (stomach)
pain
• Unexplained hemorrhage
(bleeding or bruising)
Symptoms may appear
from 2 to 21 days after
exposure to Ebola, but
the average is 8 to
10 days.
Recovery from Ebola
depends on good supportive
clinical care and the
patient's immune response.
People who recover from
Ebola infection develop
antibodies that last
for at least 10 years.
(1, 4)
Because
the
natural
reservoir
host
of
Ebola
viruses
has
not
yet
been
identified,
the
way
in
which
the
virus
first
appears
in
a
human
at
the
start
of
an
outbreak
is
unknown.
Scientists
believe
that
the
first
patient
becomes
infected
through
contact
with
an
infected
animal,
such
as
a
fruit
bat
or
primate.
Person-to-person
transmission
follows
and
can
lead
to
large
numbers
of
affected
people.
Ebola
is
spread
through
direct
contact
(through
broken
skin
or
mucous
membranes
in,
for
example,
the
eyes,
nose,
or
mouth)
with
"
blood
or
body
fluids
(including
but
not
limited
to
urine,
saliva,
sweat,
faeces,
vomit,
breast
milk,
and
semen)
of
a
person
who
is
sick
with
Ebola"
objects
(like
needles
and
syringes)
that
have
been
contaminated
with
the
virus"
infected
fruit
bats
or
primates
.
(1,2,4)
Healthcare
providers
caring
for
Ebola
patients
and
the
family
and
friends
in
close
contact
with
Ebola
patients
are
at
the
highest
risk
of
transmission
because
they
may
come
in
contact
with
infected
blood
or
body
fluids
of
sick
patients.
Diagnosing Ebola in a
person who has been infected
for only a few days is
difficult, because the
early symptoms, such as
fever, are nonspecific
to Ebola infection and
are often seen in patients
with more commonly occurring
diseases, such as malaria
and typhoid fever.
However, if a person has
the early symptoms (http://www.cdc.gov/vhf/ebola/symptoms/index.html)
of Ebola and has had contact
with the blood or body
fluids of a person sick
with Ebola, contact with
objects that have been
contaminated with the
blood or body fluids of
a person sick with Ebola,
or contact with infected
animals, they should be
isolated and public health
professionals notified.
Samples from the patient
can then be collected
and tested to confirm
infection.
The following basic interventions,
when used early, can significantly
improve the chances of
survival:
• Providing intravenous
fluids (IV)and balancing
electrolytes (body salts)
• Maintaining oxygen
status and blood pressure
• Treating other
infections if they occur
Experimental vaccines
and treatments for Ebola
are under development,
but they have not yet
been fully tested for
safety or effectiveness.
•
Practice
careful
hygiene.
•
Do
not
handle
items
that
may
have
come
in
contact
with
an
infected
person's
blood
or
body
fluids
(such
as
clothes,
bedding,
needles,
and
medical
equipment).
•
Avoid
funeral
or
burial
rituals
that
require
handling
the
body
of
someone
who
has
died
from
Ebola.
•
Avoid
contact
with
bats
and
non-human
primates
or
blood,
fluids,
and
raw
meat
prepared
from
these
animals.
•
Avoid
hospitals
in
West
Africa
where
Ebola
patients
are
being
treated.
Healthcare
workers
exposed
to
people
with
Ebola
should
:
•
Wear
protective
clothing,
including
masks,
gloves,
gowns,
and
eye
protection.
•
Practice
proper
infection
control
and
sterilization
measures.
For
more
information,
see
"Infection
Control
for
Viral
Hemorrhagic
Fevers
in
the
African
Health
Care
Setting".
•
Isolate
patients
with
Ebola
from
other
patients.
•
Avoid
direct
contact
with
the
bodies
of
people
who
have
died
from
Ebola.
•
Notify
health
officials
if
direct
contact
has
been
made
with
the
blood
or
body
fluids,
such
as
but
not
limited
to,
feces,
saliva,
urine,
vomit,
and
semen
of
a
person
who
is
sick
with
Ebola.
The
virus
can
enter
the
body
through
broken
skin
or
unprotected
mucous
membranes
in,
for
example,
the
eyes,
nose,
or
mouth
•
Laboratory
workers
are
also
at
risk.
Samples
taken
from
humans
and
animals
for
investigation
of
Ebola
infection
should
be
handled
by
trained
staff
and
processed
in
suitably
equipped
laboratories.
Good
outbreak
control
also
relies
on
applying
a
package
of
interventions,
namely
case
management,
surveillance
and
contact
tracing,
a
good
laboratory
service,
safe
burials
and
social
mobilisation.
Community
engagement
is
key
to
successfully
controlling
outbreaks.
Raising
awareness
of
risk
factors
for
Ebola
infection
and
protective
measures
that
individuals
can
take
is
an
effective
way
to
reduce
human
transmission.
National
risk
reduction
messages
should
focus
on
several
factors:
•
Reducing
the
risk
of
wildlife-to-human
transmission
from
contact
with
infected
fruit
bats
or
monkeys/apes
and
the
consumption
of
their
raw
meat.
Animals
should
be
handled
with
gloves
and
other
appropriate
protective
clothing.
Animal
products
(blood
and
meat)
should
be
thoroughly
cooked
before
consumption.
•
Reducing
the
risk
of
human-to-human
transmission
from
direct
or
close
contact
with
people
with
Ebola
symptoms,
particularly
with
their
bodily
fluids.
Gloves
and
appropriate
personal
protective
equipment
should
be
worn
when
taking
care
of
ill
patients
at
home.
Regular
hand
washing
is
required
after
visiting
patients
in
hospital,
as
well
as
after
taking
care
of
patients
at
home.
•
Outbreak
containment
measures
including
prompt
and
safe
burial
of
the
dead,
identifying
people
who
may
have
been
in
contact
with
someone
infected
with
Ebola,
monitoring
the
health
of
contacts
for
21
days,
the
importance
of
separating
the
healthy
from
the
sick
to
prevent
further
spread,
the
importance
of
good
hygiene
and
maintaining
a
clean
environment.
1.
World
Health
Organization.
http://www.who.int/csr/disease/ebola/maps/en/
2.
Allen
C.
Cheng,
Heath
Kelly.
Are
we
prepared
for
Ebola
and
other
viral
haemorrhagic
fevers?
Australian
and
New
Zealand
Journal
of
Public
Health.
doi:
10.1111/1753-6405.12303
3.
World
Health
Organization.
WHO
Statement
on
the
Meeting
of
the
International
Health
Regulations
Emergency
Committee
Regarding
the
2014
Ebola
Outbreak
in
West
Africa
[Internet].
Geneva
(CHE):
WHO;
2014
[cited
2014
Aug
15].
Available
from:
http://www.who.int/mediacentre/news/statements/2014/ebola-20140808/en/.
4.
CDC.
http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/distribution-map.html
|
|
.................................................................................................................

|
| |
|

