|
|
 |
Review Paper
........................................................
Education and Training
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| November 2014
- Volume 12 Issue 9 |
|
Comparison
of the medical students' self-assessment and simulated
patients evaluation of students' communication
skills in Family Medicine Objective Structured
Clinical Examination (OSCE).
Firdous
Jahan
(1)
Muhammed Moazzam (2)
Mark Norrish
(3)
Shaikh
Mohammed Naeem (4)
(1) Dr Firdous Jahan, Associate Professor,
Department of Family Medicine, Oman Medical
College
(2) Dr Muhammed Moazzam, Department of Family
Medicine, Oman Medical College
(3) Dr Mark Norrish, Academic coordinator, Academic
Partnerships Unit, Coventry University.
(4) Dr Shaikh Mohammed Naeem . Department of
Family Medicine, Oman Medical College
Correspondence:
Dr Firdous Jahan, Associate Professor, Department
of Family Medicine,
Oman Medical College, Oman
Email:
firdous@omc.edu.om
|
Abstract
Objective:
Comparison of the medical students' self-assessment
and the evaluation of students by simulated
patients regarding students' communication
skills in Family Medicine OSCE.
Introduction: Communication
is the act of conveying a message to another
person, and it is an essential skill for
establishing physician-patient relationships
and effective functioning among health
care professionals. Effective communication
can positively influence patient satisfaction
and outcomes. Health professional communication
skills do not necessarily improve over
time but can improve with formal communication
skills training.
Method:
A cross sectional study done at Oman Medical
College. All of the medical students who
signed up for an Objective Structured
Clinical Examination (OSCE) in Family
Medicine were included. As a part of the
OSCE, the student performance was evaluated
by a simulated patient. After the examination,
the students were asked to assess their
communication skills. The Calgary Cambridge
Observation Guide formed the basis for
the outcome measures used in the questionnaires.
A total of 12 items were rated on a Likert
scale from 1-5 (strongly disagree to strongly
agree).
Results: 68
students participated in the examination,
88% (60/68) of whom responded to the questionnaire.
The response rate for the simulated patients
was 100%. Over all comparison showed that
students marginally over estimated in
few areas as compared to simulated patients.
Measures of reliability show that it is
a reliable measure with Cronbach's Alpha
from the 12 items being 0.89. When comparing
between the experience and new simulators
only one item (q12) showed a statistically
significant difference, with t(16)=3.08,
p<0.05, with experienced simulators
giving a higher score 4.55, when compared
with the new simulators 3.86.
Conclusion: Students'
and simulated patients' assessment has
some agreements. Self-assessment is guiding
the future learning, providing reassurance,
and promoting reflection which helps them
to perform appropriately.
Key Words: Self-assessment,
communication skills, Calgary Cambridge
observation guide; Communication skills
training, under graduate medical student
|
Communication skills' training is an essential
component of medical education. Communication
is a process by which meaning is conveyed to create
shared understanding[1]. It is a skill that can
be taught and learnt; students learn this competency
in an effective learning environment. It is an
essential skill for safe, effective, and compassionate
health care to improve better outcomes in health
care system and good communication skills are
more likely to make patients satisfied with the
care they receive[2]. Learners are expected to
be actively involved and coached in communication
by their teachers specially the features of clinical
competence like empathy, compassion, counseling,
and showing support to patients[3-4]. The most
difficult aspect of the doctor-patient relationship
is ability to convey distressing news to the patients
and their relatives. Breaking bad news is an inevitable
part of medical practice[5-7]. The development
of effective communication skills is an important
part of becoming a good doctor; with appropriate
teaching, these skills can be both acquired and
retained[8]. Integrating communication with other
clinical skills- with history taking, physical
examination, and medical problem solving, help
them in real-life practice[9-10].
Interviewing real patients in real practice has
been shown to be valuable for learning communication
skills and understanding patient illnesses. The
UK's General Medical Council (GMC) emphasizes
effective communication as fundamental to good
medical practice[11].
To implement a more comprehensive approach, Calgary-Cambridge
guides is an effective tool used to teach medical
students' communication skills and practice in
a comprehensive clinical method[12]. Educators
can adopt the methods for teaching communication
that are more effective to help learners cultivate
the skills required as well as help learners set
realistic goals, and teachers should know when
and how to provide feedback to the learners in
a way that allows a deepening of skills and a
promotion of self-awareness[13-14]. Standardized
or simulated patients are used for role playing
specific communication skills or solving certain
patient problems. Simulations are good for improving
certain communication skills, and are effective
in teaching and assessing communication skills.
Teaching and Learning communication skills
at Oman Medical College:
Oman Medical College (OMC) is the only private
medical college in Oman, and offers a seven-year
curriculum, leading to the degree of Doctor of
Medicine (MD). In the 4th year (first preclinical
year) they learn Physical Diagnosis and Clinical
Integration (PDCI) clinical skills. History taking
and physical examination is conducted in the skills
lab on simulated patients(16 sessions). At the
end of the course, 2 theory exams and 1 clinical
exam are done on simulated patients(SP). In the
5th Year of PDCI they learn clinical history taking
and examination on real patients in the hospital
(32 sessions). At the end of the course Theory
Exam and Practical exam of clinical skills is
done on real patients in Sohar Hospital. Communication
skills teaching and assessment is an integral
part of clinical teaching in clinical years 6
and 7 at OMC. The Family Medicine department organizes
special communication skills sessions to help
the students communicate with their patients.
They learn knowledge of basic communication concepts,
communication models, types and functions of non-verbal
communication, ability to elicit accurate, comprehensive
and focused medical histories as well as communication
in different difficult and special situations.
Although communication skills are the integral
part of every patient encounter there are few
specialized skills they learn during Family Medicine
rotation like breaking bad news, smoking cessation
counseling, confidentiality, how to handle a difficult
patient, counseling for chronic diseases (Diabetes,
Hypertension, Obesity), Palliative and Geriatric
care.
Self-assessment is used to assess the outcome
of continuous professional development using questionnaires
and checklists focusing on skills, such as performance
skills and general clinical skills. Calgary Cambridge
Observation Guide is used as a basis for the self-efficacy
and objective assessment scores; the evaluation
tools closely match the communication skills taught.
Their communication skills are assessed during
the real consultation in the clinic as well as
mid rotation and end of rotation in Objective
Structured Clinical examination (OSCE). In the
OSCE setting simulated, standardized patients
are used for role playing different scenario.
Simulators training are done by faculty of family
medicine department maintaining a bank for simulators.
At the end of each OSCE there is a feedback session
with simulators regarding students' approach towards
patient and communication skills. OMC maintains
a SP bank managed by faculty of family medicine.
The criteria to choose SP are; minimum education
high school graduate, good English communication,
volunteers and actors, living within the city.
General training program is to give them orientation
about OMC and students, OSCE and its conduct.
Special training sessions are done twice, 4 weeks
before OSCE on a specific scenario carefully written
and reviewed by family medicine faculty. The scenario
is than discussed and role play with the SP.
In final MD OSCE 10 live stations were placed
including: A young female with lymphocytic leukemia
diagnosis as breaking bad news, a male with ureteric
colic and hematuria, a young female with Irritable
Bowel Syndrome, father of one year old child develops
febrile fit, middle aged male with community acquired
pneumonia, a middle aged male hypertensive with
recurrent Transient Ischemic Attack, an elderly
male with diabetes mellitus as follow up, a middle
aged women with menorrhagia (Dysfunctional uterine
bleeding), young boy with acute hepatitis for
abdominal examination and a young male with right
knee injury for examination of knee joints.
All stations had trained SP and all stations had
built in communication skills during consultation.
The overall objective was how the students approach
to the patient identifies the problem and manages
it. Total duration for each station was 7 minutes.
This study aimed at the comparison of students'
self-assessment and simulated patients' assessment
on students' communication skills at the end of
Family Medicine final MD OSCE.
A
cross
sectional
study
done
on
all
of
the
medical
students
who
were
signed
up
for
an
Objective
Structured
Clinical
Examination
(OSCE)
at
the
Oman
Medical
College,
June
2013
were
included
in
this
study.
There
were
2
sessions
for
simulators
training
for
the
exam
and
survey
questionnaire
by
faculty.
Questionnaires
The
Calgary-Cambridge
Observation
Guide
Checklist
formed
the
basis
for
the
outcome
measures
used
in
the
questionnaires
to
the
students
[12],
the
simulated
patients.
Twelve
items
were
chosen,
covering
domains
of
the
checklist
(initiating
the
session,
gathering
information,
building
relationship,
giving
information,
explaining
and
planning,
and
closing
the
session).The
students
were
asked
to
assess
how
confident
they
felt
being
able
to
successfully
manage
each
of
the
12
different
communication
skills
rated
on
a
Likert
scale
in
categories
1-5
(strongly
disagree
to
strongly
agree).
The
simulated
patients
were
asked
to
assess
how
the
students
succeeded
in
managing
the
12
skills
rated
on
a
similar
Likert
scale.
Validation
of
the
questionnaires
was
done.
A
pilot
test
was
performed
to
assess
the
feasibility
of
answering
the
questionnaires
for
the
standardized
patients
and
students
during
a
similar
OSCE
examination
6
months
prior
to
the
study.
Sixty eight students
participated in OSCE
of whom 60 responded
to the questionnaire,
of these -52 were women,
8 men. The response
rate for the simulated
patients was 100%.
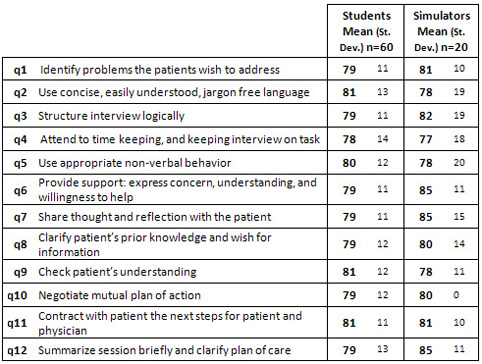
Comparison of student
self-assessment and
simulated patient evaluation
scores,when including
all 12 items evaluated.
Overall comparison showed
that students marginally
over estimated in Q
2,4,5 and 9, while remaining
items showed under estimation
(Figure 1).
Figure 1: Percentage
scores for each Item.
Likert scores for each
item (from 1-5) are
presented here as percentages
Measures of reliability
show that it is a reliable
measure with Cronbach's
Alpha from the 12 items
being 0.89. There is
one item (q10) where
the simulators show
an unusual pattern of
responses.
When comparing between
the experience and new
simulators only one
item (q12) showed a
statistically significant
difference, with t(16)=3.08,
p<0.05, with experienced
simulators giving a
higher score 4.55, when
compared with the new
simulators 3.86.
Good and appropriate
communication skills
are essential for medical
students to become an
efficient member of
a health care team in
future. Self-assessment
is guiding future learning,
providing reassurance,
and promoting reflection
which helps them to
perform appropriately
in examination[15-16].
They can reinforce students'
intrinsic motivation
to learn and inspire
them to set higher standards
for themselves[17].
In our study medical
students in the self-assessment
of communication skills,
do not overestimate
their skills. Students
have shown appropriate
self-assessment in one
of the history taking
stations; the literature
also support student's
self-assessment is good
for history taking attributes
in an OSCE[18]. Some
differences are also
shown, as they have
only marginally overestimated
their communication
skills in questions
2, 4, , 5 and 9. As
reported in literature
that communication skills
assessment measures
broader aspects of attitudes
towards learning communication
skills this may turn
out to be helpful for
monitoring the effect
of different teaching
strategies on students'
attitudes during medical
school.[19]. Another
study has shown that
students scored their
communication skills
lower compared to observers
or simulated patients.
The differences were
driven by only 2 of
12 items[20]. The results
in this study indicate
that self-efficacy based
on the Calgary Cambridge
Observation guide seems
to be a reliable tool
that can be used for
formative assessment
of health professionals
[21].
In Q10 of our study
there is no variance
in the simulators responses;
that is all simulators
chose "agree".
This lack of variance
is likely to indicate
that for this question
the simulators did not
feel confident to 'stray'
away from a default
answer. They may not
have understood the
question or may not
have felt confident
to assess it. Since
numbers are quite small
this is difficult to
ascertain. Question
number 11 seems to have
full agreement.
There is difference
seen when we have done
regression respondents
who agreed and strongly
agreed(Figure 2). Another
interesting finding
was seen in the extreme
end of Likert scale
which is strongly agree(Figure
3). While the students
seem very consistent
in the item ratings,
with the average for
all items being between
10 and 20% for "strongly
agree", the simulators
usage of "strongly
agree" is much
more variable, with
average score ranging
from 0% to nearly 40%.
Figure 2: The percentage
of respondents (students
and simulators) who
"agreed" or
"strongly agreed"
with the items
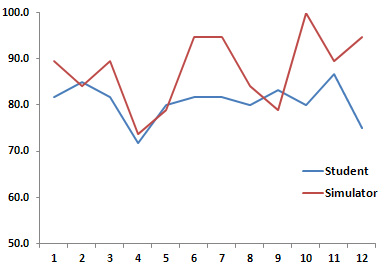
Figure 3: The percentage
of respondents (students
and simulators) who
used the extreme end
of the Likert scale
("strongly agree")

While the students
seem very consistent
in the item ratings,
with the average for
all items being between
10 and 20% for "strongly
agree", the simulators
usage of "strongly
agree" is much
more variable, with
average score ranging
from 0% to nearly 40%.
It appears that on average
the experienced simulators
are more likely to use
the extreme end of the
rating scale(Figure
4). One study has reported
that simulators' training
compared with pre workshop
standardized patient
encounters, post workshop
encounters showed significant
improvement in communication
skills [22].
Figure 4: The percentage
of simulators who used
the extreme end of the
Likert scale ("strongly
agree"), with comparison
between the new simulators
and the experienced
simulators
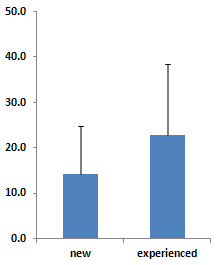
It appears that on
average the experienced
simulators are more
likely to use the extreme
end of the rating scale.
Standardized or simulated
patients or use of well-trained
actors is an alternative
way of role playing
specific communication
skills or solving certain
patient problems. Simulations
can mirror reality quite
closely and are good
for improving certain
communication skills,
such as counseling and
breaking bad news. Standardized
patient simulations
are effective in teaching
and assessing communication
skills[23]. In our study
the experienced simulators
have a higher intra-variance,
and thus they are more
willing to use a wider
range of scores in their
assessments, while the
'new' simulators, might
be a little more cautious
so are therefore using
a more narrow and restricted
range of scores in their
assessments (Figure
5). One study has shown
detailed constructive
feedback to students
from SPs is a feature
of SP contribution to
student learning[24].
Eva has reported that
, self-assessment serves
several potential functions
learning communication
and clinical skills,
becomes a part of the
training of healthcare
professionals and it
appears to be evident
and generally accepted
that communication skills
are core competencies
essential for good patient
care[25-26]. During
the training period
students are exposed
to real as well as simulated
patients. They can practice
this attribute under
supervision. Preliminary
research does indicate
that self-assessment
of clinical skills in
medical schools improves
the ability to self-assess
in clinical practice
[27]. Literature has
proven that introduction
and integration of structured
communication skills
teaching in early years
contributes greatly
in the development of
students' strengths.
The interactive examination
may be a convenient
tool for providing deeper
insight into students'
ability to prioritize,
self-assess and steer
their own learning [28].
Figure 5: This figure
shows the intra-rater
variance for the new
and experienced simulators
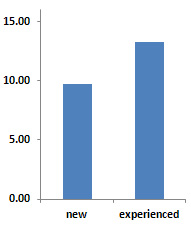
Limitation: Our
study is done on final
year medical students
at exit level exam who
may have some undue
pressure on them.
Medical
students
in
the
self-assessment
of
communication
skills,
do
not
overestimate
their
skills;
students
seem
very
consistent
in
the
item
ratings
.Students
and
simulated
patients'
assessment
has
some
agreements.
Self-assessment
is
guiding
the
future
learning,
providing
reassurance,
and
promoting
reflection
which
helps
them
to
perform
appropriately.
Acknowledgement:
The
author
would
like
to
acknowledge
Dr.
Thomas
A.
Heming,
(Vice
Dean
for
Academic
Affairs
Professor
and
Head,
Department
of
Physiology
and
Biochemistry,
Oman
medical
college)
and
Dr
Saleh
Al
Khusaiby
(Dean
Oman
medical
college)
Click
here
for
Survey
Questionnaire
for
Simulated
Patients
and
Survey
Questionnaire
for
Students
1.
Maguire
P,
Pitceathly
C.
Key
communication
skills
and
how
to
acquire
them.
British
Medical
Journal.
2002;325(7366):697-700.
2.
Aspegren
K,
Lønberg-Madsen
P.
Which
basic
communication
skills
in
medicine
are
learnt
spontaneously
and
which
need
to
be
taught
and
trained?
Med
Teacher.
2005;27(6):539-543.
3.
Sargeant
J,
MacLeod
T,
Murray
A.
An
inter
professional
approach
to
teaching
communication
skills.
Journal
Continuing
Education
in
Health
Professions.
2011
Fall;31(4):265-7.
doi:
10.1002/chp.20139.
4.
Brown
RF,
Bylund
CL.
Communication
skills
training:
describing
a
new
conceptual
model.
Academic
Medicine.
2008;83(1):37-44
5.
Deveugel,
M.,
Derese,
A.,
De
Maesschalck,
S.
Willems,
S,
Van
Driel,
M,De
Maeseneer,
J
.
Teaching
communication
skills
to
medical
students,
a
challenge
in
the
curriculum?
Patient
Education
Counseling.
2005,
58,
265-270.
6.
Back
AL,
Arnold
RM:
Discussing
prognosis:
How
much
do
you
want
to
know?''
talking
to
patients
who
are
prepared
for
explicit
information.
J
Clin
Oncol
2006;24:4209-4213.
7.
Back
AL,
Arnold
RM,
Baile
WF,
Tulsky
JA,
Barley
GE,
Pea
RD,
Fryer-Edwards
KA:
Faculty
development
to
change
the
paradigm
of
communication
skills
teaching
in
oncology.
J
Clin
Oncol
2009;27:1137-1141.
8.
Ammentorp
J,
Sabroe
S,
Kofoed
P-E,
Mainz
J.
The
effect
of
training
in
communication
skills
on
medical
doctors'
and
nurses'
self-efficacy:
a
randomized
controlled
trial.
Patient
Educ
Couns.
2007;66(3):270-277.
9.
Jørgen
Nystrup,
Jan-Helge
Larsen,
and
Ole
Risør.
Developing
Communication
Skills
for
the
General
Practice
Consultation
Process.
Sultan
Qaboos
University
Medical
Journal.
2010
December;
10(3):
318-325.
10.
Kurtz
S,
Silverman
J,
Draper
J:
Teaching
and
learning
communication
skills
in
medicine.
2nd
edition.
Oxon:
Radcliffe
publishing;
2005:58-62.
11.
General
Medical
Council.
Tomorrow's
Doctors:
Recommendations
on
Undergraduate
Medical
Education.
London:
GMC,
1993.
12.
Silverman
J,
Kurtz
S,
Draper
J:
Skills
for
Communicating
with
Patients.
Oxon:
Radcliffe
Medical
Press
Ltd;
1998.(Questionnaire)
13.
Abdulaziz
Al
Odhayani.
Teaching
communication
skills.
Canadian
Family
Physician.
2011
October;
57(10):
1216-1218.
14.
Suter
E,
Arndt
J,
Arthur
N,
Parboosingh
J,
Taylor
E,
Deutschlander
S.
Role
understanding
and
effective
communication
as
core
competencies
for
collaborative
practice.
Journal
of
Inter
professional
Care.
Jan
2009;23(1):41-51.
15.
Fryer-Edwards
K,
Arnold
RM,
Baile
W,
Tulsky
JA,
Petracca
F,
Back
AL:
Reflective
teaching
practices:
An
approach
to
teaching
communication
skills
in
the
small
group
setting.
Acad
Med
2006;81:638-644.
16.
Vicki
A.
Jackson,
M.D.,
M.P.H.
Anthony
L.
Back,
M.D.
Teaching
Communication
Skills
Using
Role-Play:
An
Experience-Based
Guide
for
Educators.
JOURNAL
OF
PALLIATIVE
MEDICINE.
Volume
14,
Number
6,
2011
17.
Mavis
B.
Self-efficacy
and
OSCE
performance
among
second
year
medical
students.
Adv
Health
Sci
Educ.
2001;6(2):93-102.
18.
Firdous
J,
Naeem
S,
Mark
N,
Najam
S,
Rizwan
Q.
Comparison
of
student's
self-assessment
to
examiners
assessment
in
a
formative
Observed
Structural
Clinical
Examination
(OSCE)
and
Correlation
between
cumulative
score
and
global
rating
scale
for
students
and
examiners
evaluation.
Journal
of
Postgraduate
Medical
Institute;
Vol
27,
No
1
(2012)
19.
Tor
Anvik,
Tore
Gude,
Hilde
Grimstad,
Anders
Baerheim,
Ole
B
Fasmer,
Per
Hjortdahl,
Are
Holen,
Terje
Risberg
and
Per
Vaglum.
Assessing
medical
students
'attitudes
towards
learning
communication
skills
-
which
components
of
attitudes
do
we
measure?
BMC
Medical
Education,
2007,
7;
4.
20.
Jette
A
,Janus
L
T,
Dorte
E
J,
René
H
,Anne
L
Ø,
Poul-Erik
K.
Comparison
of
the
medical
students'
perceived
self-efficacy
and
the
evaluation
of
the
observers
and
patients.
BMC
Medical
Education
2013,
13:49
doi:10.1186/1472-6920-13-49
21.
Back
AL,
Arnold
RM,
Baile
WF,
Fryer-Edwards
KA,
Alexander
SC,
Barley
GE,
Gooley
TA,
Tulsky
JA:
Efficacy
of
communication
skills
training
for
giving
bad
news
and
discussing
transitions
to
palliative
care.
Arch
Intern
Med
2007;167:453-460.
22.
Blanch-Hartigan
D:
Medical
students'
self-assessment
of
performance:
results
from
three
meta-analyses.
Patient
Educ
Couns
2011,
84:3-9.
23.
Kaufman
DM,
Laidlaw
TA,
Langille
D,
Sargeant
J,
MacLeod
H:
Differences
in
medical
students'
attitudes
and
self-efficacy
regarding
patient-doctor
communication.
Acad
Med
2001,
76:188.
24.
Oliver
D.
Teaching
medical
learners
to
appreciate
"difficult"
patients.
Canadian
Family
Physician.
2011;57:506-8.
e148-50.
25.
Bokken
L,
Linssen
T,
Scherpbier
A,
van
der
Vleuten
C,
Rethans
JJ.
Feedback
by
simulated
patients
in
undergraduate
medical
education:
a
systematic
review
of
the
literature.
Med
Educ.
2009;43(3):202-210.
26.
Eva
KW,
Regehr
G:
Self-assessment
in
the
health
professions:
a
reformulation
and
research
agenda.
Acad
Med
2005,
80:S46-S54.
27.
Eva
KW,
Regehr
G.
Knowing
when
to
look
it
up:
A
new
conception
of
self-assessment
ability.
Academic
Medicine.
2007;
82(10
suppl):S81-S84.
28.
Chur-Hansen
A.
The
self-evaluation
of
medical
communication
skills.
Higher
Ed
Res
Devel
2001;20:
71-9.
29.
Mattheos
N,
Nattestad
A,
Falk-Nilsson
E,
Attström
R.
The
interactive
examination:
Assessing
students'
self-assessment
ability.
Medical
Education.
2004;38(4):378-389.
|
|
.................................................................................................................

|
| |
|

