Sodium
Stibogluconate treatment for cutaneous leishmaniasis:
A clinical study of 43 cases from the north of
Jordan
Mamoun
Mohammad Al-Athamneh
Hiathem Qasem Abu Al-haija
Ra'ed Smadi
Ayman S. Qaqaa
Heba Ajlouni
Correspondence:
Dr. Mamoun Al-Athamneh
Amman, Jordan
Mobile: 0962 777 903852
Email:
mamounathamnehh@yahoo.com
|
Abstract
Objective:
to study the efficacy of Sodium Stibogluconate
intramuscular injections in the treatment
of cutaneous leishmaniasis, safety and
side effects.
Method: A total 43 patients were
seen over a period of 12 months, from
January 2009 to December 2010. All cases
were seen at Prince Rashed Military Hospital
in the north of Jordan. The diagnosis
of localized cutaneous leishmania was
made on clinical grounds proved by leishmania
smear or skin biopsy. The distribution
of patients according to gender, age groups,
time of the year, was made. The criteria
for sodium stibogluconate injection were:
the severity of symptoms, site of lesion
on face (ear, nose and cheek), and multiplicity
of lesions.
The dose of sodium stibogluconate given
was 10 mg\kg given as intramuscular injections
daily for total two weeks followed by
complete blood count, liver function test,
electrocardiogram as base line.
Results: 23 patients were males
and 20 were females (16 of them were 14
years and below). The age group ranged
from 2-72 years. One patient (2.3%) had
resistant infection to sodium stibogluconate;
and an admission was for one patient (2,
3%) for a few days because of a picture
of Hepatotoxicity. 42 patients showed
improvement of the lesion (98%); improvement
is defined when the lesion flattens and
ulceration disappears.
One patient (2.3%) demonstrated increase
in liver enzymes after one week of treatment'
upon stopping treatment for one week the
patient then resumes treatment with no
complications and with complete remission.
Conclusion:
Many cases of cutaneous leishmaniasis are
seen in Jordan causing cosmetic problems.
Early introduction of systemic anti-leishmania
agent is recommended. Sodium stibogluconate
is an effective way to decrease scarring
and dispigmentation, with minimum side effects.
Key words: cutaneous leishmania,
sodium stibogluconate, scar |
Leishmaniasis is a widely distributed disease
with both visceral and cutaneous manifestations.
Cutaneous leishmaniasis is the most common form
of this disease. It has an annual incidence of
1 to 1.5 million cases. 90% of cases are reported
in just six countries, Afghanistan, Brazil, Iran,
Peru, Saudi Arabia and Syria (1).
Cutaneous leishmaniasis causes three distinct
clinical entities: localized cutaneous leishmaniasis
(a few lesions), diffuse cutaneous leishmaniasis
(large number of lesions), muco-cutaneous leishmaniasis
(involving mucus membrane like nose, mouth,
larynx). Other leishmania species may attack
viscera causing visceral leishmaniasis or kala-azar
(1,2).
Cutaneous leishmaniasis is divided into: the
Old World and new world leishmaniasis (3). Old
world leishmaniasis is due to L. major (zoonotic
cutaneous leishmaniasis which tends to heal
within 2-4 months), L. tropica (anthroponotic
tends to heal 6-15 months), L. aethiopica and
to L. infantum, which is responsible for all
the cutaneous disease in the northern Mediterranean
region and for some of the disease in North
Africa.
In the New World, localized cutaneous leishmaniasis
is caused mainly by L. peruviana, L. guyanensis,
L. braziliensis or L. mexicana species. Diffuse
cutaneous leishmaniasis is an infection caused
by L. aethiopica in Africa, and L. amazonensis
in South America. However, diffuse cutaneous
leishmaniasis is also observed in immunosuppressed
patients infected with species isolated commonly
in localized forms. Mucosal dissemination is
described in South America. It is caused by
L. braziliensis, and, less frequently by L.
panamensis or L. guyanensis(4).
Leishmania is highly contagious with at least
ninety percent attack rate among susceptible
individuals (5). Affecting children mainly,
usually lesions are at site of sandfly bites
on exposed areas like face (7).
Cutaneous leishmaniasis is a disfiguring disease
that normally resolves within 3 to 18 months
of initial infection. Treatment aims to cure
as well as prevent the development of more complex
manifestations like Muco-cutaneous leishmaniasis
and disseminated cutaneous leishmaniasis (10).
This study was conducted to examine cutaneous
leishmania cases seen over a 12-month period,
taking into consideration patients' ages, the
time of occurrence during the year, the symptoms
and signs at presentation, the treatments given
and the complications encountered in affected
patients.
Forty three patients clinically diagnosed to have
cutaneous leishmaniasis were seen at Prince Rashid
Hospital over a period of 12 months (between January
2009 to December 2010). The distribution of patients
as regards the time of disease occurrence during
the year, sex and age group, were documented.
The diagnosis of cutaneous leishmania was established
on clinical grounds. Nodulo-ulcerative skin lesion,
with erythematous, violaceous, edematous edge
were the most common presenting features. Laboratory
investigations were carried out for all patients
and included leishmania smear to demonstrate Donovan
bodies, skin biopsy was done only if the lesion
was clinically suggestive but smear negative,
followed by routine and biochemical blood tests
including liver function test, ECG as base line.
All patients were given systemic sodium stibogluconate
intramuscular injections, 10 mg/kg per dose daily
for two weeks. The 1st injection was given in
the clinic with the availability of resuscitation
facilities to observe and interfere if anaphylactic
reaction developed, then patient completed the
course of injections at the nearest clinic. Patients
received instructions in regard to the nature
of disease and treatment options and to apply
topical antibiotics. All patients were re-examined
at follow up visit after two weeks to ensure complete
cure of the lesion.
Simple non-parametric statistical analysis was
made when necessary.
Twenty three patients (53.5%) were males and 20
patients were females (46.5%). The age ranged
from 2-72 years. The site of involvement in our
patients is shown in Table 1. The distribution
of patients according to age groups is shown in
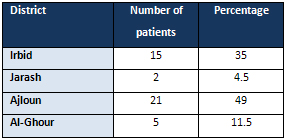
Table 2. The patients were from four districts,
Table 3. The face was commonly involved (49%)
: cheeks (39.2%), nose (18%), forehead (14.3%),
pinna (14.3%), lip (10.7), eyelid (3.5%).
Table 1: Site of involvements and their percentages
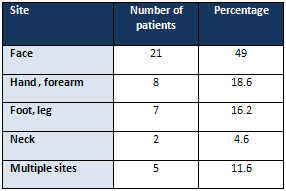
Table 2: The distribution of patients according
to age group
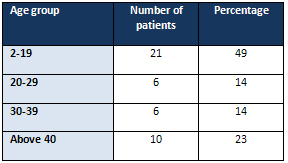
Table 3. The demographic distribution
One patient (2.3%) who was hospitalized, was 6
years old with three skin lesions on hand, neck
and ear and received 2 ml sodium stibogluconate
IM injections for one week and came to hospital
with nausea, vomiting, abdominal pain. Liver function
test showed raised liver enzyme SGOT 1838, SGPT
1306 Alkaline phosphatase 316, the 2nd day after
cessation of therapy SGOT and SGPT dropped to
1314,741 respectively. WBC, PCV, PLATELET were
normal. PT, PTT, INR normal, abdominal U/S normal,
HBSAG, HC antibodies were negative. After 6 days
SGOT and SGPT dropped to 180 and 175 respectively;
lesions at these time showed 70% improvement.
One patient (2.3%) who had ulcerative nodule at
the lower lip, clinically consistent with Cutaneous
leishmania. Leishmania smear was negative but
biopsy confirmative, and patient received sodium
stibogluconate injection for one week and developed
a slight rise in liver enzyme, Patient was stopped
for one week and returned to normal resumption
of injections with no complications with complete
healing but with atrophic scar.
One patient (2.3%) received sodium stibogluconate
injections for two weeks but did not show clinical
improvement after completion of the course of
injections, and was given alternative treatment.
Leishmaniasis are a group of chronic
infections affecting human and other animal
species, belonging to flagellated protozoans
of the order kinetoplastidae, and transmitted
by the bite of sandflies of the genera phlebotomus
and lutzomyia (5). It is an obligate intracellular
parasite that presents in two forms: promastigote
in the gut of sandflies where it multiplies
and migrates to the proboscis and is introduced
to the host whether human, rodent, or other
animal species and immediately phagocytosed
by host phagocytes where it changed into amastigote(7).
It is considered to be a self- limiting disease
when localized to skin but always heals with
retracted scar and dispigmentation but some
may become chronic or disseminated(2).
In endemic areas like Jordan where transmission
is stable, children are especially affected.
Un our study children were affected in 37% of
the cases, as shown in Table 7, and the cumulative
rate of infection as determined by the presence
of scars and positive leishmanin tests may approach
100%.
The treatment of cutaneous leishmaniasis depends
on the species of leishmania but identification
of the species by culture and isoenzyme is time
consuming. Also new techniques of DNA amplification
by polymerase chain reaction are not widely
available which makes treatment depend on the
geographical area and the epidemiology of the
disease; the main cause of cutaneous leishmania
in our area is leishmania tropica (5).
Cutaneous leshmaniasis is the primary infection
with one of the leishmania species starting
as a papule then increasing in size resulting
in a nodulo-ulcerative lesion, usually on exposed
areas at the site of sandfly bite (5). In our
study, there are 21 cases (49%) involving the
face, 8 cases (18.6%) involving the hand and
forearm, 7 cases (16.2%) involving the foot
and leg, 2 cases (4.6%) involving the neck,
5 cases (11.6%) involving multiple sites of
those mentioned above with no single case involving
a non-exposed area.
Ajloun district had the highest number of patients
simply because towns of Ajloun are geographically
appropriate for sandflies living and reproduction
regarding temperature and humidity.
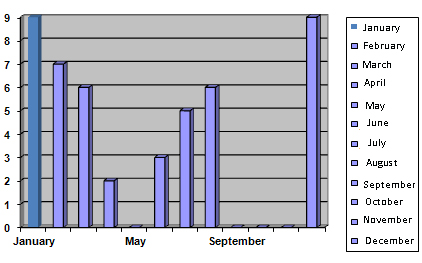
Our study shows the highest number of patients
in January and December then March (Figure 1),
and this may be due to rainy season in winter
with the formation of swamps which allow reproduction
and growth of sand flies which facilitate vector
transmission .
Figure 1: The distribution of patients according
to the time of year
Pentavalent antimonials are the mainstay treatment
for both visceral and cutaneous leishmaniasis
(8). Two forms are currently available: meglumine
antimoniate and sodium stibogluconate. The mechanism
for their effectiveness is not well understood,
but may involve inhibition of adenosine triphosphate
synthesis(9).
The face is affected in 49% of the cases; it
results in scarring and dispigmentation which
is disfiguring on the face.
It is generally recommended that anyone with
cutaneous leishmaniasis is to be treated with
systemic sodium stibogluconate (especially children
and when face is involved) because scar and
dispigmentation will be inevitable and disastrous.
Systemic antimonial decrease the size of the
lesion, there is no progression to ulceration
and results in less scarring, and rapid healing.
Therefore, we started all patients on sodium
stibogluconate injection for two weeks; 98%
showed complete cure of the lesion upon follow
up 2-3 months after completion of the course.
One of the most important side effects of sodium
stibogluconate is prolongation of QT interval
predisposing to arrhythmias, which are uncommon
when used in doses less than 20mg/kg and within
a period of less than 2 weeks (6). In our study
base line ECG was done excluding patients with
abnormal Electrocardiogram from the study; follow
up Electrocardiogram was done with no change.
Hepatotoxicity is another side effect of sodium
stibogluconate injection which is reversible
withen 6 weeks of cessation of treatment (6).
Base line liver function tests were done to
exclude any patient with liver disease from
the study; two patients developed increases
in liver enzyme which returned to normal within
two weeks of cessation of treatment.
Wide use of sodium stibogluconate in the treatment
of cutaneous leishmaniasis can result in the
emergence of a resistant strain(9). In our study
one patient did not show improvement clinically
after completion of the course of injections
(still the lesion was wet and increasing in
size). The mechanism for the development of
resistance is not well understood. It could
be an intrinsic difference in the species sensitivity
to these medications; another mechanism is the
efflux of a drug or its active derivative(9).
Studies showed that the addition of allopurinol
to the treatment regimen gave better results
regarding decrease of the size of the lesion
and clearance (4). In our resistant case just
when it showed no healing, a change to rifampicin
300mg daily for 2 weeks allowed healing of the
lesion.
In addition, there are several alternative treatment
options available; local infiltration with sodium
stibgluonate of the whole lesion intradermally
with 2-3ml every week until 4 weeks (4). Also
Oral zinc sulphate (5 mg/kg/day for 4 weeks)
showed promising results in a recent Indian
trial (8).
Cryotherapy using liquid nitrogen is a well
known option for treatment in the middle east
including Jordan where 2-3 sessions for 20-30
seconds freezing (one month interval) resulted
in healing of most of the lesion but with a
different degree of atrophic scar and dispigmentation.
But when multiple lesions, large lesions, over
the joint, are on the face, the cosmetic unit
usually tries to avoid cryotherapy.
Cutaneous Leishmaniasis is cosmetically disfiguring
and slowly growing skin lesions are not fatal
but occasionally can result in significant morbidity
especially when present on the face.
Early treatment with systemic antimonial agent
is essential in the adults and children to prevent
or decrease the risks of complication like: scarring
and dispigmentation.
We believe that it is highly recommended to give
systemic sodium stibogluconate injection to all
patients with Cutaneous leishmaniasis, especially
when certain areas like ear, eyelid, lip, cheek,
nose, and multiple lesions are present.
1. World health organization
(WHO). Leishmaniasis:
background information
. A brief history of disease
.WHO. 2009. available
from: www.WHO.int\leishmaniasis.
2. Omar Lupi. Protozoa
and worms. In: bolongia
dermatology 2nd Ed.2008.p.1263-1265.
3. Blum J, Desjeux P,
Schwartz E, Beck B, Hatz
C. Treatment of cutaneous
leishmaniasis among travellers.
J Antimicrob Chemother
2004; 53:158-66.
4. Philippe Minodiera,
Philippe Parolab. Cutaneous
leishmaniasis treatment.
Travel Medicine and Infectious
Disease (2007) 5, 150-158(review
article free online).
5. Barbara L. Herwaldt.
Leishmaniasis. In: Kasper
DL (Editor-In-Chief).
Harrison's principles
of internal medicine.
16th Ed. New York: McGraw-Hill
Companies, Inc. 2005.
p. 1233-1236.
6. Wise ES, Armstrong
MS, Watson J, Lockwood
DN. Monitoring Toxicity
Associated with Parenteral
Sodium Stibogluconate
in the Day-Case
Management of Returned
Travellers with New World
Cutaneous Leishmaniasis.
PLoS Negl Trop Dis 6(6):
e1688. doi:10.1371/journal.pntd2012
(free online).
7. Wolff, Klaus; Goldsmith,
Lowell A. Leishmaniasis
and other protozoan infections.
In: Fitzpatrick's Dermatology
in General Medicine, 7th
Edition. McGraw-Hill,
Inc. 2008. ch. 206
8. J.A.A. Hunter, J.A.
Savin, M.V. Dahl. Leishmaniasis.
In: Clinical dermatology.
3rd Ed.2003.p.201-202.
9. Arun Kumar Haldar,
Pradip Sen, and Syamal
Roy .Use of Antimony in
the treatment of Leishmaniasis:
Current Status and Future
Directions. Review Article.
Molecular Biology International
at: http://dx.doi.org/10.4061/2011/571242.2011.
10. Tracy Garnier &
Simon L Croft. Topical
treatment for cutaneous
leishmaniasis.
Department of Infectious
and Tropical Diseases,
London School of Hygiene
& Tropical Medicine.
Email: simon.croft@lshtm.ac.uk
,Current Opinion in Investigational
Drugs 2002 3(4):
|

