|
Medical Education and
the Practice of Medicine in the Muslim countries
of the Middle East
Lesley Pocock
Mohsen Rezaeian
Correspondence:
Lesley Pocock
Publisher - medi+WORLD International
Australia
Email: lesleypocock@mediworld.com.au
|
Abstract
and Overview
Recorded history shows the ancient countries
and populations of the Middle East were
among the first in the world to teach
and practice the science of medicine,
and from the region, it spread to the
rest of the known world.
This paper provides
firstly a history of the regional development
of the science of medicine followed by
a brief snapshot of current regional medical
education and research, to see if it is
matching the needs of the people of the
region, and reaching and setting the same
high standards as it did centuries ago.
|
The Middle East region was not just the cradle
of civilisation, the place where humans stopped
their nomadic hunting and gathering, and started
to form towns and cities and complex cultures,
it was also where some of the more complex sciences
and arts were first practised and recorded.
Historical records show that the practice of
medicine occurred in the early history of Egypt,
Persia, Mesopotamia, China, India, Greece and
the city of Rome, before the third century AD
(1).
In the history of the Middle East the practice
of medicine was first recorded in Persia (Iran).
The Vendidad, a surviving collection of texts,
devotes many chapters to the practice of medicine.
One of these texts describes three kinds of
medicine: medicine by the knife (surgery), medicine
by herbs (pharmacology), and medicine by divine
words (counselling or placebo) (1, 2).
An encyclopaedia of medicine in Pahlavi literature
listed 4,333 diseases (1, 2).
The city of Gondi-Shapur in Persia (226 to
652 AD) had the first institution we would recognise
as a modern day hospital and academic centre
of learning. These institutions were called
bimarestan, a Persian word for ‘a place
for the sick,’ and as well as providing
medical services they also retained patients’
medical records (1-6).
The academy of Gondi-Shapur was established
between 309 to 379 AD and consisted of a university,
a library and a teaching hospital. Similar to
modern academic medicine the bimarestan of Gondi-Shapur
were a place where medical students worked in
the hospital under the supervision of a medical
faculty. There is evidence that the graduates
had to then pass an examination in order to
practice as accredited physicians (1).
After the Arabs conquered Persia in 638 AD,
Gondi-Shapur became the Arabian School of Medicine.
The entire system was gradually transferred
to Baghdad, where it became known as the ‘Golden
Age of Islamic Medicine’ (1).
The philosophy behind this Golden Age of universal
healthcare was the Islamic belief in the Qur’an
and Hadiths, which stated that Muslims had a
duty to care for the sick (3-6). In the Islamic
Age such hospitals were paid for through charitable
donations. They were founded as early as the
8th Century and eventually were set up across
the entire Islamic world (3-6). The hospitals
also provided free medical services to the poor
and sent physicians and midwives into rural
areas. Some hospitals provided early ‘specialist
services’ such as midwifery and care for
lepers and the disabled (3-6).
Al-Razi, (850 - 923), of Persia, was an early
medical researcher. He produced over 200 books
about medicine and philosophy, including a book
where he compiled all known medical knowledge
in the Islamic world. This book was translated
into Latin and was the basis of the early western
medical education system (4).
Al-Razi, also initiated scientific methods
promoting experimentation and observation. He
wrote on the relationship between doctor and
patient, believed in a holistic approach to
medicine and was instrumental in early ‘history
taking,’ not just of the medical background
of the patient but also the patients’ family
members. He advanced medical diagnosis through
looking for the cause of the symptoms (4-6)
and described human physiology and understood
how the brain and nervous system worked (4-6).
In 14th century Persia, the book Tashrih al-badan
(Anatomy of the body), was written by Mansur
ibn Ilyas (c. 1390), and contained an early
Atlas of Anatomy with diagrams of the body’s
structural, nervous and circulatory systems
(4-6).
Human
history
has
seen
the
rise
and
fall
of
many
Empires,
Kingdoms
and
regions.
The
entropy
that
pervades
matter
on
the
micro
scale
seems
to
also
work
on
the
macro
scale
and
while
we
will
not
look
at
the
philosophical
or
psychosocial
reasons
for
these
cycles
in
this
article,
the
glorious
past
of
the
Middle
East
region
is
now
undergoing
some
needed
revival
in
these
scholarly
disciplines.
The
Islamic
religion
fostered
early
the
view
of
medicine
as
a
science
to
be
learned
and
understood,
as
well
as
the
concept
of
parity
of
healthcare
for
all
members
of
society,
(universal
healthcare)
irrespective
of
the
patient’s
ability
to
afford
it.
This
spirit
lives
on
in
the
universal
health
systems
most
Middle
Eastern
countries
have
adopted,
particularly
in
Iran,
which
the
WHO
describes
as
one
of
the
most
robust
health
systems
worldwide,
drawing
its
strength
from
its
pioneering
and
well
established
primary
health
care
system,
which
emphasizes
equity,
community
and
intersectoral
participation,
as
well
as
government
financing
of
essential
and
other
services
(7).
As
well
as
University
based
medical
schools
most
regional
countries
now
have
postgraduate
colleges
to
focus
on
standards
and
ongoing
medical
education
to
support
and
address
the
needs
of
practising
doctors
and
specialists.
The
region
hosts
many
international
medical
conferences
and
quite
a
few
overseas
universities
have
set
up
campuses
in
the
region.
Some
Universities
that
have
recently
re-appraised
their
focus
and
customs
are
high
in
the
list
of
the
top
universities
in
the
world,
(e.g.
Aga
Khan
University
and
Hospital
in
Karachi,
Lahore
University
of
Management
Sciences,
and
Sharif
University
in
Iran)
(2).
Many
countries
have
ongoing
medical
education
programs,
in
the
form
of
Continuing
Medical
Education
(CME)
and
Continuing
Professional
Development
(CPD)
e.g.
UAE,
Jordan,
Turkey
and
Lebanon.
Generally
however,
and
additional
to
the
march
of
time
from
the
glorious
days
of
the
past,
a
multitude
of
factors
has
led
to
various
problems
in
most
countries
of
the
region.
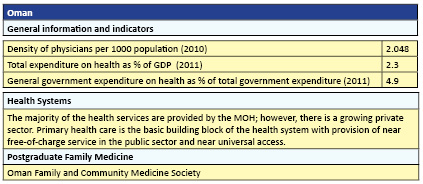
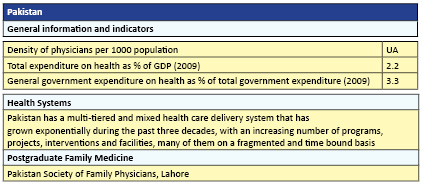
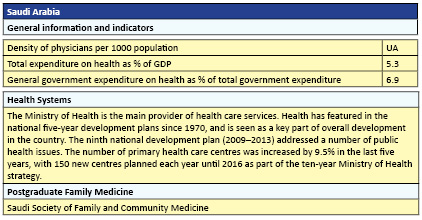
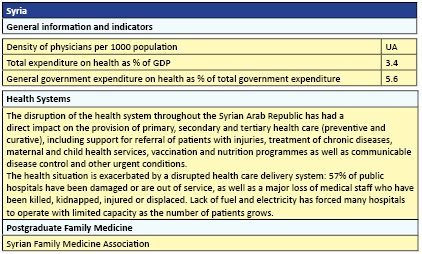
Before
discussing
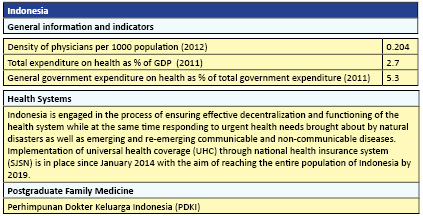
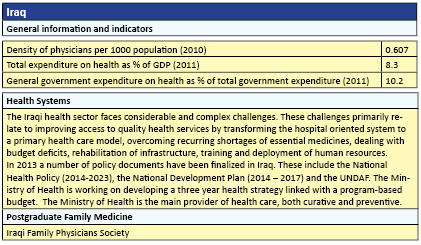
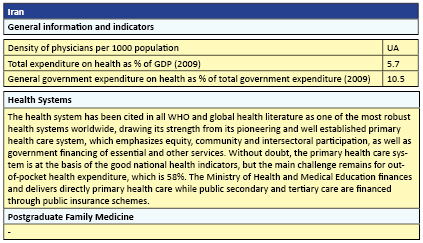
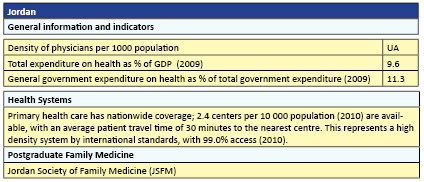
these
factors,
the
following
provides
a
snapshot
of
the
main
features
of
the
health
and
medical
education
status
of
each
major
Middle
East
country
compared
with
some
non-regional
Muslim
countries,
Malaysia
and
Indonesia.
The
practice
of
medicine
is
to
ultimately
address
the
current
health
needs
of
a
population,
through
medical
education
and
training,
research
and
public
health
policies,
along
with
affordable
healthcare.
The
people
of
the
Middle
East
now
face
much
the
same
disease
states
as
the
rest
of
the
developed
world
and
medical
education
and
health
policy
must
now
meet
these
changing
needs.
The
change
of
lifestyles
in
the
Middle
East
and
elsewhere
has
introduced
a
new
range
of
disease
states,
particularly
those
of
a
cardiovascular
nature
(e.g.
diabetes
and
heart
disease).
This
in
turn
has
necessitated
a
change
of
both
health
priorities
and
educational
focus.
In
the
Middle
East
and
North
Africa
region,
incidence
of
non-communicable
diseases
such
as
heart
disease
are
up
by
44%,
stroke
up
by
35%,
and
diabetes
up
87%
since
1990
and
these
diseases
are
causing
more
premature
death
and
disability
than
they
did
in
the
past
(9).
The
region
has
succeeded
in
reducing
disease
burden
from
many
communicable,
newborn,
nutritional,
and
maternal
conditions.
However,
lower
respiratory
infections,
remain
the
second
leading
cause
of
healthy
years
lost
in
the
region
(9).
Aging
populations
and
longevity
add
another
dimension
to
economic
burden,
and
new
diagnostic
equipment,
techniques
and
therapeutics
have
created
higher
expectations
of
successful
medical
outcomes
in
patient
populations.
At
the
same
time
these
innovations
have
greatly
increased
the
cost
of
both
medical
education
and
delivery
of
universal
health
care.
This
also
applies
to
the
cost
of
medicines,
particularly
highly
priced
pharmaceutical
products,
with
many
nations
of
the
world
now
having
to
subsidise
their
high
costs
to
make
them
available
to
their
patient
populations.
At
the
same
time,
poorer
countries
in
the
region,
including
Yemen,
Djibouti,
and
Iraq,
continue
to
struggle
with
a
high
burden
from
infectious
diseases
(9).
Among
the
Muslim
countries
in
the
region,
the
leading
causes
of
disease
burden
range
from
preterm
birth
complications
in
Algeria
and
Palestine,
depression
in
Jordan,
and
ischemic
heart
disease,
or
coronary
artery
disease,
in
Egypt,
Iran
and
Lebanon
(9).
When
comparing
rates
of
diseases
and
injuries
across
countries
in
the
Middle
East
and
North
Africa
and
taking
into
account
differences
in
population
growth
and
ages,
Lebanon,
Syria,
and
Tunisia
performed
best
relative
to
other
countries
in
the
region
while
Iraq,
Yemen,
and
Djibouti
performed
the
worst
(9).
In
places
such
as
Palestine
(and
currently
Syria,
Iraq,
and
Libya)
even
greater
burdens
of
war
are
placed
on
health
systems
that
are
being
destroyed
and
made
ineffective.
It
seems
it
may
even
now
be
policy
to
deliberately
target
doctors
and
hospitals
to
demoralise
such
communities.
Climate
change
and
environmental
problems,
often
exacerbated
by
war
or
government
dysfunction,
(e.g.
no
collecting
of
waste,
scarcity
and
quality
of
clean
drinking
water,
air
pollution)
contribute
to
the
picture
as
does
an
upsurge
in
road
accidents.
There
is
need
for
specific
public
health
promotion
to
limit
lifestyle
disease
and
poor
health
habits
such
as
cigarette
smoking
and
drug
taking
as
well
as
addressing
mental
health
issues
such
as
the
rising
incidence
or
diagnosis
of
depression.
Refugees
within
the
region
bring
their
own
set
of
problems
–
not
just
in
additional
healthcare
needs
but
sequelae
of
war:
malnutrition,
injuries,
mental
health
issues,
overcrowded
conditions
and
disease
risk.
Current
regional
Medical
Education
does
not
always
match
or
meet
the
high
principle
of
universal
healthcare.
Varying
standards
of
education
within
the
region
often
result
in
new
regional
graduates
unable
to
find
employment,
or
even
qualify
for
employment
in
the
region.
At
the
same
time
well
educated
doctors
are
often
poached
by
overseas
employers
who
can
offer
greater
financial
returns.
Conversely
some
Middle
East
countries
preferentially
hire
overseas
doctors
and
nurses
to
meet
their
own
internal
needs
putting
a
greater
burden
on
health
systems.
The
opportunities
for
higher
levels
of
research
and
publication
can
also
be
lacking
in
the
region.
Most
countries
of
the
Middle
East,
and
Muslim
countries
generally
do
now
endeavour
to
provide
universal
healthcare
but
with
varying
success.
It
must
be
said
that
most
countries
of
the
world
have
now
also
adopted
the
principle
of
universal
healthcare
but
with
some
notable
exceptions,
even
among
developed
countries.
The
reasons
why
the
Universities
are
not
providing
adequately
trained
doctors
to
meet
the
needs
of
the
regions’
medical
hiring
organisations
are
complex
and
may
differ
from
country
to
country.
Governments,
academics
and
administrators
of
regional
universities
will
need
to
address
any
deficiencies
in
their
curricula
and
postgraduate
institutions.
The
Organisation
of
Islamic
Cooperation
(OIC)
in
its
Report
of
29
October
2015
recommended
that
governments
must
give
universities
more
autonomy.
Professors
need
to
be
free
to
teach
topics
that
are
not
tightly
regulated
by
ministries
(2).
Universities
need
to
also
be
free
from
political
or
religious
opinion
or
influence.
There
is
precedent.
In
Pakistan,
two
private
universities
established
in
the
1980s,
the
Aga
Khan
University
and
Hospital
in
Karachi
and
Lahore
University
of
Management
Sciences,
revolutionized
medical
and
business
education
within
a
decade
of
their
creation.
Students
elsewhere
began
demanding
the
standard
set
by
these
educational
pioneers
(2).
The
OIC
report
found
that
the
Muslim
countries
on
average
invest
less
than
0.5%
of
their
gross
domestic
product
(GDP)
on
research
and
development
(R&D).
Students
in
the
Muslim
world
who
participate
in
standardized
international
science
tests
perform
below
the
standards
of
their
peers
worldwide,
and
the
situation
seems
to
be
worsening
(2).
An
obvious
reason
for
this
however
may
be
a
non-standardised
curriculum.
The
OIC
recommend
that
Universities
in
OIC
nations
need
to
be
granted
more
autonomy
to
transform
themselves
(2).
University
science
programmes
are
often
found
to
be
using
restricted
content
and
outdated
teaching
methods.
The
OIC
report
also
stated
scientific
research
must
be
relevant
and
responsive
to
society’s
intellectual
and
practical
needs
and
students
must
receive
a
broad,
liberal
education.
Some
basic
scientific
facts
are
still
seen
as
controversial,
and
marginalized
e.g.
evolution
(2).
Another
problem
is
that
faculty
members
rarely
receive
any
training
or
evaluation
in
pedagogy.
In
many
OIC
universities,
didactic
teaching
methods
persist
(2).
In
many
universities,
curriculum
changes,
faculty
appointments
and
promotions
are
dictated
by
governments
Ministries
of
Health
and
other
agents.
The
57
countries
of
the
Muslim
world
that
are
a
part
of
the
Organisation
of
Islamic
Cooperation
(OIC)
are
inhabited
by
nearly
25%
of
the
world’s
people.
But
as
of
2012,
they
had
contributed
only
1.6%
of
the
world’s
patents,
6%
of
its
academic
publications,
and
2.4%
of
the
global
research
expenditure
(2).
The
number
of
scientific
papers
they
produce
remains
below
the
average
of
countries
with
similar
GDP
per
capita.
A
few
institutions
attempt
to
relate
their
students’
learning
to
their
cultural
backgrounds
and
contemporary
knowledge.
The
Times
Higher
Education
world
university
rankings
named
Sharif
University
as
the
top
Iranian
university
and
number
eight
in
the
OIC
(10).
Habib
University,
in
Pakistan,
also
follows
the
same
model.
Textbooks
are
often
imported
from
outside
the
region.
Although
of
a
high
standard,
they
assume
a
Western
undergraduate
experience
and
are
written
in
English
or
French
(2).
Having
English
as
the
standard
international
medical
and
scientific
language
disadvantages
students
from
all
countries
that
are
not
native
English
speakers.
The
heavy
requirements
on
academics
to
publish
whether
there
is
research
of
any
importance
or
repute
occurring
in
their
institution
or
if
there
is
anything
of
significant
merit
to
report
or
not,
can
also
cause
problems.
There
should
be
less
emphasis
on
meeting
quotas,
and
more
on
quality
and
the
merit
of
publishing
particular
research
or
study
(11).
This
also
applies
worldwide.
While
it
is
necessary
to
acknowledge
the
workload
and
academic
pressure
during
medical
training
there
should
also
be
time
and
budgets
allocated
for
meaningful
research
and
publication
(10,
11).
Quality
academics
themselves
need
to
be
properly
salaried
and
remunerated.
Regional
medical
journals
are
assisting
young
researchers
and
academics
(10,
11)
A
healthy
national
medical
education
consists
of
both
tertiary
and
postgraduate
medical
education
institutions.
It
is
well
recognised
these
days,
especially
in
times
of
great
change,
that
education
does
not
stop
once
the
graduate
goes
into
practice
(lifelong
learning).
Not
only
are
there
new
developments
and
techniques,
new
therapeutics
and
new
diagnostic
equipment
at
the
primary
care
population
level,
we
have
seen
the
emergence
of
quite
a
few
new
diseases
(e.g.
Ebola)
and
mutations
of
existing
diseases
(e.g.
Zika).
There
is
also
place
and
requirement
for
the
practising
doctor
to
contribute
to
ongoing
knowledge
regarding
emergence
and
epidemiology
of
emerging
and
mutating
viral
diseases
(15).
Socio-economic
and
psychosocial
issues
affecting
the
practice
and
delivery
of
medicine
can
and
do
vary
from
nation
to
nation.
It
is
no
longer
good
enough
to
‘keep
your
eye’
on
the
medical
journals;
doctors
need
a
consistent
approach
to
ongoing
medical
education.
Many
postgraduate
medical
colleges
have
brought
in
firstly,
Continuing
Medical
Education
(CME),
then
Continuing
Professional
Development
(CPD),
with
the
latter
a
step
ahead
in
that
it
is
no
longer
good
enough
to
know
‘what’s
new’,
doctors
need
to
evaluate
new
information
and
know
if,
when
and
why
they
should
introduce
it
into
practice.
It
is
not
acceptable
to
put
patients
on
a
new
therapy
unless
doctors
are
sure
it
works
in
all
patients
and
all
situations
and
if
its
trials
have
been
sufficient
in
time,
enrolled
numbers
and
efficacy
and
with
no
longterm
adverse
effects
on
patients.
QA&CPD
(Quality
Assurance
and
Continuing
Professional
Development)
was
brought
in
to
provide
a
level
of
science
(and
mathematics)
to
CME/CPD.
Postgraduate
Education
Providers
need
to
know
and
be
able
to
show
that
the
doctor-student
has
indeed
learned
something
(accurate)
from
their
post
graduate
education
and
that
the
education
they
provide
to
the
doctors
has
done
its
job
at
the
level
of
patient
care.
There
also
needs
to
be
someone
to
ensure
the
quality
of
postgraduate
continuing
education
and
this
is
usually
done
by
the
Postgraduate
College
or
Academy
testing
and
training
and
evaluating
postgraduate
education
providers,
be
they
tertiary
colleges,
universities,
a
medical
society,
or
independent
providers.
Finally
Quality
Improvement
(QI)
has
become
the
current
norm.
The
doctor
undergoing
postgraduate
CME/CPD
has
to
now
show
that
the
postgraduate
education
has
brought
Quality
Improvement
into
their
practice.
There
are
many
ways
to
go
about
this
–
even
though
they
require
a
bit
of
subjective
evaluation
on
the
part
of
the
practising
doctor.
To
enforce
Quality
Assurance
(QA)
and
Lifelong
learning
as
part
of
regular
practice,
it
has
become
a
requirement
for
maintaining
ongoing
Professional
Vocational
Registration
(VR)
in
some
countries.
The
Vocational
Registration
requirement
approach
can
however
be
punitive
to
the
patient
populations
if
there
are
not
enough
doctors
practising
(quality
assured
or
not)
-
on
the
assumption
that
those
practising
have
some
basic
skills.
In
countries
greatly
lacking
in
doctors
another
aim
of
CME
should
be
to
improve
the
skills
of
doctors
already
in
practice.
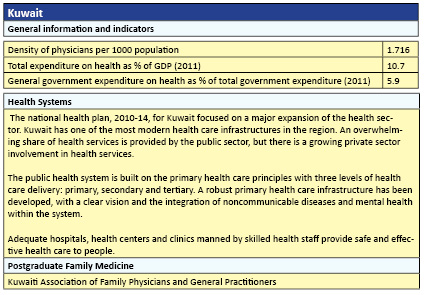
Some
of
the
first
family
medicine
programs
in
the
region
occurred
in
Turkey
in
1961,
in
Bahrain
in
1978,
in
Lebanon
in
1979,
in
Jordan
in
1981,
and
in
Kuwait
in
1983.
Family
medicine
programs
have
also
been
established
in
Qatar,
the
United
Arab
Emirates,
Libya,
and
Iraq.
In
most
programs,
family
medicine
training
occurs
mostly
in
hospitals,
even
though
few
Middle
Eastern
family
physicians
practice
in
hospitals
on
completion
of
residency
training.
Thus,
there
is
a
need
for
better
outpatient
training,
but
resistance
from
those
responsible
for
traditional
medical
education
can
make
it
difficult
to
change
the
current
model.
There
is
need
for
better
opportunities
for
professional
development
after
graduation
and
for
establishing
research
activities
in
family
medicine
(12).
Financing
the
medical
education
and
health
sector
is
an
increasing
national
burden
and
involves
major
and
obvious
considerations
–
good
coordinated
governance
across
all
sectors,
national
wealth
and
development
being
the
most
obvious.
Some
Middle
East
countries
have
a
‘patronage’
system
whereby
institutions
need
to
continually
apply
for
separate
items
of
funding
preventing
them
to
some
degree
from
being
able
to
plan
ahead
and
invest
in
necessary
infrastructure.
Overseas
universities
have
also
set
up
in
the
region
and
thus
provide
their
own
curricula
and
own
education
and
their
graduates
often
then
proceed
to
practice
overseas.
It
does
however
allow
those
employers
seeking
‘western
trained
doctors’
to
employ
graduates
from
the
region.
Regular
and
ongoing
funding
and
sufficient
levels
of
funding
are
needed
to
ensure
that
each
country
produces
sufficient
numbers
of
doctors
to
adequately
care
for
population
health.
Political
will
and
allocation
of
government
budgets
is
tied
together.
Of
course
investing
in
tertiary
education
facilities
and
professional
staffing,
needs
to
also
be
weighted
against
the
potential
student
population.
Small
populations
on
a
pro
rata
basis
require
heavier
financial
commitments.
While
the
principles
and
practice
of
‘universal
healthcare
for
all’
is
well
championed
in
the
Middle
East
region
there
seems
to
be
need
for
improvement
in
the
quality
and
availability
of
undergraduate
and
ongoing
medical
education
to
meet
the
ongoing
needs
and
expectations
of
the
populations
of
each
country.
This
may
need
a
review
of
numbers
entering
the
education
system
as
well
as
the
curriculum
in
medical
schools,
to
ensure
they
meet
all
population
health
needs.
There
is
discrepancy
between
health
planning
and
the
application
in
practice
(14).
In
most
countries
the
medical
education
system
is
not
producing
enough
primary
care
doctors,
or
to
the
standards
now
required
by
the
region
and
the
world.
The
health
care
system
still
tends
to
be
specialist
orientated.
It
is
well
accepted
globally
that
primary
care
is
the
optimum
approach
for
cost
effective
healthcare
for
all
(14).
Keeping
patients
out
of
the
hospital
system
and
the
more
expensive
specialist
system
reduces
national
health
costs
and
saves
those
services
for
the
patients
who
really
need
them.
There
needs
to
be
a
coordinated
governance
system
looking
at
all
sectors
and
making
sure
they
work
together
in
an
efficient
and
complementary
fashion.
Medical
schools
should
meet
three
criteria,
i.e.
educating
medical
students
in
sufficient
numbers
to
quality
international
standards
to
meet
national
requirements
and
needs,
conducting
research,
and
being
a
community
advocate
for
national
and
regional
health
and
medical
issues
and
ensuring
curriculum
meets
these,
and
thirdly,
providing,
via
suitably
educated
graduates,
health
and
medical
care
to
all
members
of
society
based
on
ethical
guidelines.
Medical
schools
should
consider
the
needs
of
the
communities
which
they
serve
and
deliver
their
services
based
on
socially
and
culturally
acceptable
criteria
(13).
It
is
incumbent
on
governments
to
make
the
necessary
financial
allocations
to
the
education
sector
and
to
secure
ongoing
budgets
to
allow
them
to
plan
for
the
future.
The
more
money
spent
on
ensuring
a
fit
and
proper
medical
education
and
health
delivery
system,
the
less
money
spent
later
on
public
health
needs.
In
turn,
universities
and
medical
schools
must
seek
to
contain
the
costs
of
education
and
educate
students
on
cost
effective
treatment
and
processes
of
care.
A
socially
accountable
medical
school
provides
its
services
based
on
the
criteria
of
cost-effectiveness,
relevance,
equity
and
high
quality
(13).
One
process
however
may
not
necessarily
meet
the
specific
needs
of
all
communities
or
nations,
and
it
is
incumbent
on,
firstly,
governments
and
health
administrators
to
plan
national
needs
and
then
have
the
education
systems
capable
of
producing
the
trained
medical
professionals
to
meet
those
needs.
Universities
and
medical
schools
need
to
meet
these
challenges
with
the
appropriate
curriculum
and
processes
if
they
are
to
remain
viable
and
relevant
to
community
needs.
1.
Journal
of
Perinatology
(2011)
31,
236–239.
2011
Nature
America,
Inc.
0743-8346/11
2.
Nidhal
Guessoum,
Athar
Osama.
Revive
universities
of
the
Muslim
world.
Nature,
Vol.
5
2
6,
2
9
October
2
0
1
5
3.
Medicine
in
the
medieval
Islamic
world
-
Wikipedia,
https://en.wikipedia.org/wiki/Medicine_in_the_medieval_Islamic_world
4.
Islamic
Medicine
-
History
of
Medicine
-
Explorable.com.
https://explorable.com/islamic-medicine
5.
Royal
Society.
A
New
Golden
Age?
The
Prospects
for
Science
and
Innovation
in
the
Islamic
World
(Royal
Society,
2010).
6.
Royal
Society.
The
Atlas
of
Islamic
World
Science
and
Innovation
(Royal
Society,
2014).
7.
WHO
Country
Profiles.
http://www.who.int/countries/en/)
8.
Global
Family
Doctor
-
WONCA
Online;
www.globalfamilydoctor.com/
9.
The
World
Bank
/
IHME:
In
Middle
East
and
North
Africa,
Health
Challenges
are
Becoming
Similar
to
Those
in
Western
Countries.
2013
10.
Research
participation
among
medical
trainees
in
the
Middle
East
and
North
Africa
Ahmed
Salem,
Sameh
Hashem,
Layth
Y.I.
Mula-Hussain,
Ala’a
Nour,
Imad
Jaradat,
Jamal
Khader,
Abdelatif
Almousa
11.
Rezaeian
M,
Pocock,
L.
Plagiarism
and
Self
plagiarism
from
the
perspective
of
academic
authors.
MEJFM
May
2016
-
Volume
14,
Issue
4
12.
Abyad
A1,
Al-Baho
AK,
Unluoglu
I,
Tarawneh
M,
Al
Hilfy
TK.
Development
of
family
medicine
in
the
middle
East.Fam
Med.
2007
Nov-Dec;39(10):736-41.
13.
Rezaeian,
M.
Pocock,
L.
Social
accountability
-
a
challenge
for
global
medical
schools.
World
Family
Med
J.
2011;
9
:15-19.
14.
Cayley
Jr
WE,
Pocock
L,
Inem
V,
Rezaeian,
M.
Global
Competencies
in
Family
Medicine.
World
Family
Med
J.
2010;
8
:19-32.
15.
Pocock
L,
Rezaeian
M.
Virology
vigilance
-
an
update
on
MERS
and
viral
mutation
and
epidemiology
for
family
doctors.
Middle
East
J
Family
Med.
2015;
13(5)
:52-59.
|

