|
Improving Hypertension
Control via a Team-based Educational and Refill
Monitoring (TERM) Intervention, Sharjah, United
Arab Emirates
Sameh F.
Ahmed
Hany M. Aiash
Hassan A. Abdel-Wahid
Family
Medicine Department, Faculty of Medicine,
Suez Canal University, Egypt
Correspondence:
Sameh
F. Ahmed
Department of Family Medicine,
Faculty of Medicine,
Suez Canal University, Ismailia, 41111
Egypt
Phone: 0020-01116646623
Email: ymddsm@gmail.com
|
Abstract
Background:
There are insufficient blood pressure
control rates even in high-performing
health systems, and effective management
of hypertension remains a challenge in
a real-life general practice. This is
because of many factors including unhealthy
life style, improper prescribing and poor
medication adherence. Cost effective and
innovative interventions to improve BP
control are therefore needed.
Aim: We aimed to study the impact
of a 6-month Team- based Educational and
Refill Monitoring (TERM) intervention
in improving BP control among UAE adult
citizens diagnosed with hypertension.
Methods:
This is a clinical trial, where, 214
hypertensive UAE citizens 18 years participated
in a 6 months TERM intervention compared
with 214 hypertensive UAE citizens receiving
usual care, Primary Health Care Department,
Sharjah Medical District (SMD), United
Arab Emirates (UAE). Before the intervention,
all physicians, pharmacists and nurses
of the TERM group were enrolled in a one
week medical education three sessions.
These sessions provided information in
two domains: practice guidelines based
on guidelines of the Joint National Committee
(JNC 7) (13) and principles of health
education and communication. As well,
a monthly health education session, telephone
calls and SMS messages have been used
to intensify medication adherence and
hypertension self-management of TERM patients.
The primary outcomes were changes in systolic
blood pressure (SBP), diastolic blood
pressure (DBP), medication refill adherence
(MRA) and blood pressure (BP) control.
Results: Participants
had a mean age of 57.4± 11 years
(TERM) and 57.5± 11.1 years (control).
57.1% were males (TERM) and 57.9% were
females (control). At baseline there was
no significant difference between both
groups in regard to occupation, education,
smoking, blood lipids, body mass index
(BMI), SBP, DBP and MRA. Meanwhile, at
baseline, only 35% of TERM patients compared
to 34.9% of usual care patients had controlled
blood pressure (defined as BP< 140/90
mmHg). At 6 months, TERM participants
achieved greater improvements compared
to usual care group in regard to SBP (139.3
± 14.2 mmHg vs. 152± 13.4
mm Hg, P<0.001), DBP (85.3±
9.3 vs. 92.4± 6.8 mm Hg, P<0.001),
BP control (50% vs. 36%, P = 0.01) and
medication refill adherence (92% vs.86%,
P<0.001).
Conclusion:
A team-based educational intervention
for both staff and patients led to significant
improvement in SBP, DBP, MRA and BP control
in adult hypertensive patients, primary
health care setting, Sharjah Medical District,
UAE.
Key words: Blood
pressure control, health education, medication
adherence, team-based care
|
Hypertension is the single most important
modifiable risk factor for the development of
cardiovascular diseases, accounting for 13%
of mortality worldwide (54% for stroke and 47%
for ischemic heart disease). (1,3,4) A systematic
review reporting data from studies in 35 different
countries between the years 2003 and 2008 demonstrated
an overall hypertension prevalence of 37.8%
for men and 32.1% for women.(2)
It is striking that blood pressure goals continue
to be achieved in only 25–40% of the patients
who take antihypertensive drug treatment, a
statistic that has remained unchanged for the
past 40 years.(3,10,11) Fortunately, adequate
blood pressure (BP) control can reduce mortality
and produce significant cardiovascular benefits
in all patients.(4,5,21) However, translation
into clinical practice of advances in management
of HTN is suboptimal, largely because of barriers
that exist at the levels of the patient, the
health care provider, and the health care system.
One of the main existing barriers to optimal
BP control is poor adherence to timely medication
refill and other issues contributing to lack
of provider intensification of this adherence.(6,21)
Because hypertension is almost entirely managed
by the primary care team, primary health care
tools like health education can create opportunities
for patients to better understand their conditions
and the role of therapies, as well as, to heighten
awareness about disease progression and complications.
Educational intervention can also positively
modify patients’ beliefs and misconceptions,
which in turn can lead to a change in patient’s
behavior, such as improvement in medication
adherence and healthy lifestyle, therefore,
potentially leading to improved blood pressure
control and the related complications.(7-20)
A Cochrane review of 72 randomized controlled
trials compared various interventions for controlling
blood pressure and concluded that a complex
intervention aiming at improving patient recall
systems to intensify medication refill, education
of doctors to improve medication prescribing
skills and patients education to improve healthy
life styles and self-management, were the best
strategies to improve hypertension control.(7)
Owing to the high morbidity and mortality caused
by hypertension, and the global scale of this
important public health issue, we found an urgent
need to continue to investigate suitable interventions
that can improve blood pressure control in a
community like primary health care, where many
opportunities for improvement are available
mainly with the provision of free health care.
Our study tests the impact of a team based educational
and medication intensification intervention
in improving blood pressure control.
This is a controlled clinical trial where 214
known hypertensive UAE citizens, registered
in Sharjah Family Health Center , Sharjah Medical
District, UAE, participated in a 6 months (January
2013 to June 2013) culturally tailored team-based
educational intervention.
This intervention group was compared with 214
hypertensive citizens receiving usual care in
another urban family health center of the same
district (Riqa FHC). Before the intervention,
all physicians, pharmacists and nurses of the
TERM group were enrolled in a one week medical
education three sessions. These sessions provided
information in two domains: core hypertension
knowledge and practice guidelines based on guidelines
of the Joint National Committee (JNC 7) (13)
and principles of health education and communication.
These sessions were conducted by a consultant
family doctor who was also working among TERM
researchers. As well, TERM patients attended
doctor-led once-weekly 2 –hour educational
sessions for one month including: definitions
of high BP, symptoms and complications of HTN,
BP home monitoring, BP control goals, follow
up intervals, MRA as well as nutritional and
exercise advice.
Intensification of medications adherence was
done through scheduled appointments, SMS messages
and phone calls to remind patients of refill
due dates. The patient was considered unreachable
after 3 unsuccessful phone calls, one of them
at the same refill due date. Non adherence to
medication refill was considered immediately
after the due date. Nurses were responsible
for sending SMS, while pharmacists were responsible
for scheduling refill appointments and phone
calls. All TERM members were involved in continuous
patient education and assessment of medication
adherence when the patients attended the PHC
center monthly to refill their medications (as
per local drug dispensing regulations). At base
line, both groups were compared regarding sociodemographic
characteristics (age, sex, marital status, occupation,
and education), smoking status, resting BP,
BMI, and ECG to diagnose left ventricular hypertrophy
and blood samples were collected after a 10-12-hour
fasting for assessment of glycated haemoglobin
(HbA1c), serum lipid profile (SLP) and kidney
function tests (KFT). Patients under dialysis
or who had mental disability were excluded from
the study. Office BP was measured by trained
nurses using an automated BP monitor with the
patient seated comfortably for 5 minutes before
each measurement, following JNC7 guidelines(13).
Blood pressure was defined as uncontrolled if
SBP 140 mm Hg or DBP 90 mmHg. Height and weight
were measured without shoes and measurements
were recorded to the nearest 1 cm and 0.1 kg
respectively. These data were used to compute
body mass index. All the above tests and measures
were obtained at baseline and after 6 months
in both intervention and control groups. Meanwhile
comparison was done within the same group to
compare any change between baseline and end
of the study results. Ethical approval was obtained
from the Ethics Commission of the Sharjah Medical
District (reference number: 13-5537-BO, date
of approval: 7 September 2012) and verbal informed
consent was taken from all TERM patients.
Statistical
analysis:
Data
were
analyzed
using
Statistical
Program
for
Social
Science
(SPSS)
version
18.0.
Quantitative
data
were
expressed
as
mean±
standard
deviation
(SD).
Qualitative
data
were
expressed
as
frequency
and
percentage.
Independent-samples
t-test
of
significance
was
used
when
comparing
between
two
means,
paired
sample
t-test
of
significance
was
used
when
comparing
between
related
samples
and
P-value
<0.05
was
considered
significant.
Base
Line
Characteristics
Table
1:
Comparison
between
intervention
and
control
groups
as
regards
baseline
characteristics
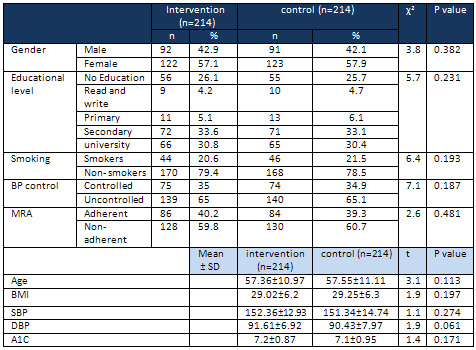
BMI=
body
mass
index,
SBP=
systolic
blood
pressure,
DBP=
diastolic
blood
pressure,
BPC=
blood
pressure
control,
MRA=
medication
refill
adherence
Table
1
shows
no
significant
statistical
difference
in
baseline
characteristics
of
both
intervention
and
control
groups
as
regards
age,
sex,
SBP,
DBP,
BP
control,
BMI
and
medication
refill
adherence.
Intervention
Change
Of
Systolic
And
Diastolic
Blood
Pressure
Table
2:
Comparison
between
intervention
and
control
groups
regarding
systolic
and
diastolic
BP
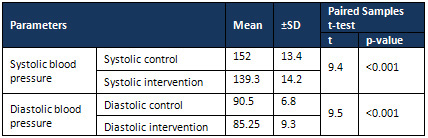
Table
2
shows
high
statistically
significant
difference
in
DBP
between
control
and
TERM
group
after
intervention
as
regards
to
both
SBP
and
DBP
Figure
1:
Comparison
between
control
and
TERM
group
at
baseline
and
after
intervention
as
regards
to
BP
control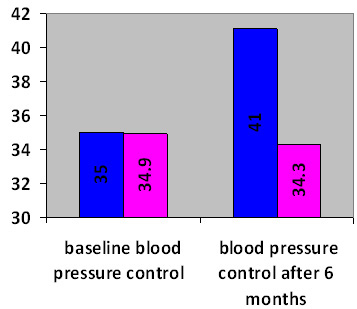
Figure
1
shows
marked
improvement
in
blood
pressure
control
among
TERM
participants
as
compared
with
the
usual
care
group
and
the
baseline
assessment
after
6
month
of
intervention.
Meanwhile,
the
control
rate
declined
in
usual
care
group
after
6
month
of
baseline
assessment.
Post
Intervention
Change
of
Medication
Adherence
Figure
2:
Percentage
of
refilling
in
TERM
vs
control
group
at
base
line
and
after
6
months
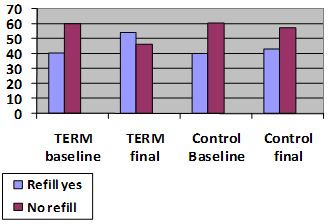
Figure
2
illustrates
significant
improvements
in
refill
adherence
among
TERM
participants
compared
to
usual
care
group
(54%
vs.
43%,
P
=<0.001).
There
was
also
significant
improvement
within
the
TERM
group
in
regard
to
refill
adherence
after
6
months
of
intervention
compared
to
usual
care
group
(54%
vs.
40.2%,
P
=<0.001).
Post
Intervention
Changes
of
Smoking
Habit
Figure
3:
Smoking
status
in
TERM
and
control
groups
at
baseline
and
final
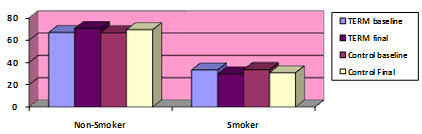
Figure
3
shows
more
improvement
in
smoking
quit
rate
among
TERM
participants(3.9%)
compared
to
usual
care
group
(0.2%).
Similarly
there
was
improvement
in
smoking
cessation
within
the
TERM
participants
after
6
months
of
intervention
(3.6%)
compared
to
baseline,
the
case
which
was
not
found
among
the
usual
care
group.
Post
Intervention
Changes
Of
Cholesterol,
Triglycerides,
BMI
and
HbA1c
Table
3:
Comparison
between
intervention
and
control
groups
regarding
total
cholesterol,
triglycerides,
BMI
and
HbA1c
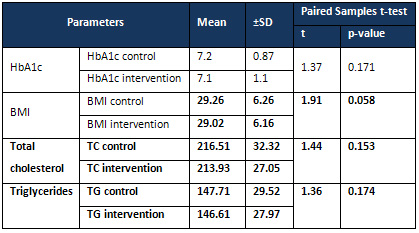
Table
3
shows
insignificant
difference
between
TERM
and
control
group
as
regards
to
mean
HbA1c,
BMI,
total
cholesterol
and
triglycerides.
Fortunately,
adequate
blood
pressure
(BP)
control
can
reduce
mortality
and
produce
significant
cardiovascular
benefits
in
all
patients.(4,5)
It
is
striking
that
blood
pressure
goals
continue
to
be
achieved
in
only
25–40%
of
the
patients
who
take
antihypertensive
drug
treatment,
which
is
a
statistic
that
has
remained
unchanged
for
the
past
40
years.(2,6,8)
In
our
study
BP
was
found
largely
uncontrolled
(65%
and
65.1%
)
in
base
line
assessment
of
intervention
and
control
groups
respectively,
despite
the
fact
that
all
UAE
citizens
have
free
access
and
utilization
of
all
health
care
services.
Unsurprisingly,
many
other
studies
found,
like
ours,
high
rates
of
uncontrolled
HTN
among
patients
with
free
access
to
health
care.
(6–8,18)
This
indicates
the
presence
of
multiple
determinants
of
hypertension
control
other
than
availability
and
utilization
of
free
services.
Many
cluster
randomized
trials
from
different
countries
evaluated
various
educational
and
organizational
approaches
to
improve
blood
pressure
control
rates
in
primary
care
(22-36).
Most
of
these
studies
applied
educational
sessions
for
physicians
and/or
patients
in
combination
with
newly
designed
external
support
structures
(24-31).
Two
types
of
external
support
structures
can
be
differentiated.
The
first
category
comprises
electronic
reminders
on
self-care
(26)
and
the
second
category
used
physician-support
structures,
either
by
external
study/audit
centers
or
clinical
pharmacists.(28-31)
The
effects
of
these
interventions
vary
from
a
mean
group
difference
of
-
0.2
mmHg
(31)
to
10.3
mmHg
in
systolic
blood
pressure(29)
and
from
-
0.4
mmHg(31)
to
4.6
mmHg
in
diastolic
blood
pressure.(28)
Interventions
aimed
at
changing
regular
care
need
to
be
based
on
an
in-depth
understanding
of
the
health
care
system
that
they
are
addressing
(15).
We
designed
the
present
study
for
the
Sharjah
primary
health
care
system,
which
is
based
mainly
on
primary
health
care
centers
that
are
regionally
distributed
in
the
various
neighbourhoods
close
to
their
patients.
These
practices
typically
serve
both
UAE
citizens
and
expatriates
with
free
services
offered
only
to
UAE
citizens.
Imbibing
the
important
milestones
set
by
the
above
referenced
studies,
we
tried
to
conceptualize
a
study
which
was
based
only
on
team
performance
without
any
external
support
system
addressing
the
team-based
care
as
the
master
of
the
practice.
Our
study
revealed
significant
improvement
in
medication
refill
adherence
in
TERM
patients
compared
to
the
usual
care
group
after
6
months
of
intervention
(54%
versus
43%,
P
=<0.001)
with
significant
improvement
in
SBP
(139.3
±
14.2
versus
152±13.4),
DBP
(85.25
±9.3
versus
90.5
±6.8)
and
overall
blood
pressure
control
(41
%
versus
34.9%).
In
a
similar
study,
at
6
months,
intervention
participants
achieved
greater
improvements
in
refill
adherence
(60%
versus
34%,
P
<
0.001),
SBP
(-12.62
versus
-5.31
mm
Hg,
P
<
0.001),
and
blood
pressure
control
(50%
versus
36%,
P
=
0.01)
compared
to
a
usual
care
group
in
primary
health
care
settings.
(22)
A
similar
study
reported
comparable
differences
where
the
intervention
group
had
a
mean
reduction
in
systolic
BP
at
6
months
of
18.3±1.2
compared
with
11.8±1.9
mm
Hg
in
the
usual
care
group.
(17)
In
contrast
to
these
findings,
another
study
showed
no
difference
in
SBP
after
a
14-month
intervention
compared
to
usual
care
group
(-8.9
mm
Hg
in
the
intervention
group
in
comparison
with
-9.0
mmHg
in
usual
care
group).
(12)
In
another
study,
the
proportion
of
adherent
participants
to
medication
refill
increased
in
both
intervention
and
control
groups
compared
to
base
line
assessment
but
with
insignificant
difference
between
the
two
groups
[57•2%
to
63•6%
(control)
versus
60•0%
to
73•5%
(intervention),
P
=
0•23].
The
mean
reduction
in
systolic
BP
was
significantly
greater
in
the
intervention
group
(10•0
mmHg
versus
4•6
mmHg;
P
=
0•05).
(23)
These
findings
show
the
importance
of
evaluating
the
effectiveness
of
different
trials
in
real-life
clinical
settings
before
widespread
adoption
in
all
settings.
In
the
present
study,
there
was
also
significant
reduction
of
smoking
(3.9
%
in
TERM
participants
versus
0.2%
in
control
group
P<
0.001);
however,
there
was
no
significant
difference
in
the
HbA1C,
lipid
profile
or
BMI
amongst
the
two
groups.
These
results
were
expected
as
most
of
the
studies
revealed
effectiveness
of
any
motivational
intervention
even
to
the
level
of
simple
advice
on
the
overall
cigarette
quit
rates.(37)
However,
blood
lipids
and
weight
control
need
more
specific
interventions
that
may
require
a
more
sophisticated
approach
that
combines
diet,
exercise
and
drug
treatment.
In
addition
studies
of
short
duration
like
the
present
one
are
unlikely
to
yield
enough
health-related
outcome
information
to
permit
interpretation
of
intervention
effects.
In
our
study,
the
significant
reduction
difference
after
6
months
from
baseline
between
TERM
and
usual
care
group,
in
not
only
the
systolic
but
also
the
diastolic
blood
pressures)
and
overall
blood
pressure
control
has
proven
that
an
overall
management
package
of
physician
education,
patient
education,
nutritional
and
exercise
advice,
intensification
of
medication
adherence,
has
definitely
proven
its
mettle.
The
limitation
of
this
study
lies
in
the
fact
of
lacking
a
randomization
factor,
as
well
as
a
few
shortcomings
of
data
collection
variables
namely
the
appropriate
classification
of
period
of
hypertension,
current
medications
for
hypertension
or
any
comorbidities
as
well
as
the
dosages,
lack
of
quality
of
life
assessment
(EQ5D
questionnaires),
and
mental
status
assessment.
Furthermore,
there
could
be
a
Hawthorne
effect,
where
there
is
a
tendency
of
some
people
to
work
harder
and
perform
better
when
they
participate
in
an
experiment.
One
of
the
most
frequently
occurring
barriers
against
medication
refill
adherence
was
that
local
drug
dispensing
regulations
allow
UAE
citizens
to
collect
their
medication
from
any
PHC
center
whenever
they
are
overdue.
Finally,
lack
of
staff
and
crowded
practice
posed
the
biggest
challenge
to
implementation
of
the
study.
Future
randomized
studies
incorporating
these
factors
shall
pave
a
more
scientific
proof
for
this
TERM
initiative.
A
team-based
6
months
educational
intervention
involving
doctors,
pharmacists
and
nurses
combined
with
simple
medication
intensification
tools
like
monthly
SMS
and
follow
up
phone
calls
led
to
significant
improvement
in
medication
refill
adherence,
SBP,
DBP
and
hypertension
control
among
adult
hypertensive
citizens,
in
a
primary
health
care
setting,
Sharjah
Medical
District,
UAE.
This
trial
can
be
considered
fruitful
in
lieu
of
the
significant
results
obtained
as
hypothesized.
1.
World
Health
Organization
(WHO):
Global
health
risks:
Mortality
and
burden
of
disease
attributable
to
selected
major
risks.
WHO,
Geneva;
2009.
Available
at:
www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report.
2.
Pereira
M,
Lunet
N,
Azevedo
A,
et
al.
Differences
in
prevalence,
awareness,
treatment
and
control
of
hypertension
between
developing
and
developed
countries.
J
Hypertens
2009;
27:963–75.
3.
Paul
A.
James,
Suzanne
Oparil,
Barry
L.
Carter,
William
C.
Cushman,
Cheryl
Dennison-Himmelfarb,
et
al.
Evidence-Based
Guideline
for
the
Management
of
High
Blood
Pressure
in
Adults:
Report
From
the
Panel
Members
Appointed
to
the
Eighth
Joint
National
Committee
(JNC
8)
JAMA.
2014;311(5):507-520.
4.
Kearney
PM,
Whelton
M,
Reynolds
K,
et
al.
Global
burden
of
hypertension:
analysis
of
worldwide
data.
Lancet
2005;365:217–23.
5.
Lopez
AD,
Mathers
CD,
Ezzati
M,
et
al.
Measuring
the
Global
Burden
of
Disease
and
Risk
Factors,
1990–2001.
Global
Burden
of
Disease
and
Risk
Factors,
2006.
Available
at:
http://www.ncbi.nlm.nih.gov/books/NBK11812/.
6.
Heisler
M1,
Hofer
TP,
Schmittdiel
JA,
Selby
JV,
Klamerus
ML,
et
al.
Improving
blood
pressure
control
through
a
clinical
pharmacist
outreach
program
in
patients
with
diabetes
mellitus
in
2
high-performing
health
systems.
Circulation.
2012
Jun
12;125(23):2863-72.
7.
Glynn
LG,
Murphy
AW,
Smith
SM,
Schroeder
K,
Fahey
T.
Interventions
used
to
improve
control
of
blood
pressure
in
patients
with
hypertension.
Cochrane
Database
Syst
Rev
2010.
Available
at:
http://www.cdc.gov/mmwr/preview/mmwrhtml/6004a4.htm
8.
Achim
Mortsiefer,
Tobias
Meysen,
Martin
Schumacher,
Heinz-Harald
Abholz,
Karl
Wegscheider
and
Jürgen
in
der
Schmitten.
From
hypertension
control
to
global
cardiovascular
risk
management:
an
educational
intervention
in
a
cluster-randomised
controlled
trial.
BMC
Family
Practice.
2015;
56
(16)
9.
Magadza
C,
Radloff
SE,
Srinivas
SC.
The
effect
of
an
educational
intervention
on
patients’
knowledge
about
hypertension,
beliefs
about
medicines,
and
adherence.
Res
Soc
Adme
Pharm
2009;5:363–75.
10.
Mancia
G,
Fagard
R,
Narkiewicz
K,
Redón
J,
Zanchetti
A,
Böhm
M,
et
al.
2013
ESH/ESC
Guidelines
for
the
management
of
arterial
hypertension:
the
Task
Force
for
the
management
of
arterial
hypertension
of
the
European
Society
of
Hypertension
(ESH)
and
of
the
European
Society
of
Cardiology
(ESC).
J
Hypertens
2013,
31:1281-357
11.
Higgins
JPT,
Green
S,
eds.
Cochrane
handbook
for
systematic
reviews
of
interventions
version
5.1.0
[updated
March
2011].
The
Cochrane
Collaboration,
2011.
www.cochrane-handbook.org
12.
Hill
MN,
Miller
NH.
Compliance
enhancement:
A
call
for
multidisciplinary
team
approaches.
Circulation.
1996;93:4–6.
13.
JNC7report:availableat
http://www.nhlbi.nih.gov/files/docs/guidelines/jnc7
14.
Birgitta
Weltermann,
Anja
Viehmann,
and
Christine
Kersting.
Hypertension
management
in
primary
care:
study
protocol
for
a
cluster
randomized
controlled
trial.
Trials.
2015;
16:
105.
15.
Michele
Heisler,
MD,
MPA;
Timothy
P.
Hofer,
MD,
MS;
Julie
A.
Schmittdiel
et
al.
Improving
Blood
Pressure
Control
Through
a
Clinical
Pharmacist
Outreach
Program
in
Patients
With
Diabetes
Mellitus
in
2
High-Performing
Health
Systems.
Circulation.
2015
Jul
14;132(2):93-100.
16.
Tsuyuki
RT1,
Houle
SK2,
Charrois
TL2,
Kolber
MR2,
Rosenthal
MM2,
et
al.
Randomized
Trial
of
the
Effect
of
Pharmacist
Prescribing
on
Improving
Blood
Pressure
in
the
Community:
The
Alberta
Clinical
Trial
in
Optimizing
Hypertension
(RxACTION).
Circulation.
2015
Jul
14;132(2):93-100.
17.
Roumie
CL,
Elasy
TA,
Greevy
R,
Llu
X,
Stone
WJ,
Wallston
KA,
et
al.:
Improving
Blood
Pressure
Control
through
Provider
Education,
Provider
Alerts,
and
Patient
Education.
Ann
Intern
Med
2006,
145:165-75.
18.
Carter
BL,
Bergus
GR,
Dawson
JD,
Farris
KB,
Doucette
WR,
Chrischilles
EA,
et
al.
A
cluster
randomized
trial
to
evaluate
physician/pharmacist
collaboration
to
improve
blood
pressure
control.
J
Clin
Hypertens
2008,
10:260-71.
19.
Carter
BL,
Ardery
G,
Dawson
JD,
James
PA,
Bergus
GR,
Doucette
WR,
et
al.
Physician
and
pharmacist
collaboration
to
improve
blood
pressure
control.
Arch
Intern
Med
2009,
169:1996-2002.
20.
Hennessy
S,
Leonard
CE,
Yang
W,
Kimmel
SE,
Townsend
RR,
Wasserstein
AG,
et
al.:
Effectiveness
of
a
Two-Part
Educational
Intervention
to
Improve
Hypertension
Control:
A
Cluster-Randomized
Trial.
Pharmacotherapy
2006,
26:1342-7.
21.
Lüders
S,
Schrader
J,
Schmieder
RE,
Smolka
W,
Wegscheider
K,
Bestehorn
K:
Improvement
of
hypertension
management
by
structured
physician
education
and
feedback
system:
cluster
randomized
trial.
Eur
J
Cardiovasc
Prev
Rehabil
2010,
17:271-9.
22.
Reuther
LO,
Paulsen
MS,
Andersen
M,
Schultz-Larsen
P,
Christensen
HR,
Munck
A,
et
al.
Is
a
targeted
intensive
intervention
effective
for
improvements
in
hypertension
control?
A
randomized
controlled
trial.
Fam
Pract
2012,
29:626-32.
23.
Mancia
G,
Fagard
R,
Narkiewicz
K,
Redón
J,
Zanchetti
A,
Böhm
M,
et
al.
2013
ESH/ESC
Guidelines
for
the
management
of
arterial
hypertension:
the
Task
Force
for
the
management
of
arterial
hypertension
of
the
European
Society
of
Hypertension
(ESH)
and
of
the
European
Society
of
Cardiology
(ESC).
J
Hypertens
2013,
31:1281-357.
24.
Paul
A.
James,
William
C.
Cushman,
Cheryl
D.
Himmelfarb.
2014
Evidence-Based
Guideline
for
the
Management
of
High
Blood
Pressure
in
Adults:
Report
From
the
Panel
Members
Appointed
to
the
Eighth
Joint
National
Committee
(JNC
8)
.
JAMA.
2014;311(5):507-520.
25.
Svarstad
BL,
Kotchen
JM,
Shireman
TI,
Brown
RL,
Crawford
SY,
Mount
JK,
Palmer
PA,
Vivian
EM,
Wilson
DA.
Improving
refill
adherence
and
hypertension
control
in
black
patients:
Wisconsin
TEAM
trial.
J
Am
Pharm
Assoc
(2003).
2013
Sep-Oct;53(5):520-23.
26.
Stewart
K1,
George
J,
Mc
Namara
KP,
Jackson
SL,
Peterson
GM,
Bereznicki
LR,
Gee
PR,
Hughes
JD,
Bailey
MJ,
Hsueh
YA,
McDowell
JM,
Bortoletto
DA,
Lau
R.
Adherence:
a
cluster-randomized,
controlled
trial
(HAPPy
trial).
J
Clin
Pharm
Ther.
2014
Oct;39(5):527-34.
27.
Heisler
M,
Hofer
TP,
Klamerus
ML,
Schmittdiel
J,
Selby
J,
Hogan
MM,
et
al.:
Study
protocol:
The
Adherence
and
Intensification
of
Medications
(AIM)
study
-
a
cluster
randomized
controlled
effectiveness
study.
Trials
2010,
11:95.
28.
Heisler
M,
Hofer
TP,
Schmittdiel
JA,
Selby
JV,
Klamerus
ML,
Bosworth
HB,
et
al.:
Improving
Blood
Pressure
Control
Through
a
Clinical
Pharmacist
Outreach
Program
in
Patients
With
Diabetes
Mellitus
in
2
High-Performing
Health
Systems:
The
Adherence
and
Intensification
of
Medications
Cluster
Randomized
Controlled
Pragmatic
Trial.
Circulation
2012,
125:2863-72.
29.
Logan
AG,
Irvine
MJ,
McIsaac
WJ,
Tisler
A,
Rossos
PG,
Easty
A,
et
al.:
Effect
of
Home
Blood
Pressure
Telemonitoring
With
Self-Care
Support
on
Uncontrolled
Systolic
Hypertension
in
Diabetics.
Hypertension
2012,
60:51-7.
30.
Roumie
CL,
Elasy
TA,
Greevy
R,
Llu
X,
Stone
WJ,
Wallston
KA,
et
al.:
Improving
Blood
Pressure
Control
through
Provider
Education,
Provider
Alerts,
and
Patient
Education.
Ann
Intern
Med
2006,
145:165-75.
31.
Carter
BL,
Bergus
GR,
Dawson
JD,
Farris
KB,
Doucette
WR,
Chrischilles
EA,
et
al.:
A
cluster
randomized
trial
to
evaluate
physician/pharmacist
collaboration
to
improve
blood
pressure
control.
J
Clin
Hypertens
(Greenwich)
2008,
10:260-71.
32.
Carter
BL,
Ardery
G,
Dawson
JD,
James
PA,
Bergus
GR,
Doucette
WR,
et
al.:
Physician
and
pharmacist
collaboration
to
improve
blood
pressure
control.
Arch
Intern
Med
2009,
169:1996-2002.
33.
Hennessy
S,
Leonard
CE,
Yang
W,
Kimmel
SE,
Townsend
RR,
Wasserstein
AG,
et
al.:
Effectiveness
of
a
Two-Part
Educational
Intervention
to
Improve
Hypertension
Control:
A
Cluster-Randomized
Trial.
Pharmacotherapy
2006,
26:1342-7.
34.
Lüders
S,
Schrader
J,
Schmieder
RE,
Smolka
W,
Wegscheider
K,
Bestehorn
K:
Improvement
of
hypertension
management
by
structured
physician
education
and
feedback
system:
cluster
randomized
trial.
Eur
J
Cardiovasc
Prev
Rehabil
2010,
17:271-9.
35.
Pouchain
D,
Lièvre
M,
Huas
D,
Lebeau
J,
Renard
V,
Bruckert
E,
et
al.:
Effects
of
a
multifaceted
intervention
on
cardiovascular
risk
factors
in
high-risk
hypertensive
patients:
the
ESCAPE
trial,
a
pragmatic
cluster
randomized
trial
in
general
practice.
Trials
2013,
14:318.
36.
Reuther
LO,
Paulsen
MS,
Andersen
M,
Schultz-Larsen
P,
Christensen
HR,
Munck
A,
et
al.:
Is
a
targeted
intensive
intervention
effective
for
improvements
in
hypertension
control?
A
randomized
controlled
trial.
Fam
Pract
2012,
29:626-32.
37.
Núria
Codern-Bové,
Enriqueta
Pujol-Ribera,
Margarida
Pla,
Javier
González-Bonilla,
et
al.:
Motivational
interviewing
interactions
and
the
primary
health
care
challenges
presented
by
smokers
with
low
motivation
to
stop
smoking:
a
conversation
analysis.BMC
Public
Health.
2014;
14:
1225.
|

