|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |


|
Editorial
A. Abyad (Chief Editor)
Special
Editorial - Honour
Lesley Pocock Publisher
and Ethics Edito
|
|
|
|
|
........................................................ |
Original
Contribution / Clinical Investigation
|


|
<-- Egypt -->
Improving
Hypertension Control via a Team-based Educational
and Refill Monitoring (TERM) Intervention, Sharjah,
United Arab Emirates
[pdf version]
Sameh F. Ahmed, Hany M. Aiash, Hassan A. Abdel-Wahid
<-- Oman/United Kingdom/Egypt -->
Perception
of stress, anxiety, depression and coping strategies
among medical students at Oman Medical College
[pdf
version]
Firdous Jahan, Muhammad A Siddiqui, Mohammed
Mitwally, Noor Said Jasim Al Zubidi, Huda Said
Jasim Al Zubidi
|
........................................................
Case Report
........................................................
Special Education Feature
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| September 2016
- Volume 14, Issue 6 |
|
|
CME Needs Assessment:
National Model
Abdulrazak
Abyad (1)
Ninette Bandy (2)
(1) Abdulrazak Abyad, MD, MPH, MBA, AGSF
(2) Ninette Banday, BDS, MPH, DMSc, FICOI,FICD
Correspondence:
Dr Abdulrazak Abyad
Email: aabyad@cyberia.net.lb
This
CME Needs Assessment paper was written to provide
analysis on a particular regional country’s
<<the country>> proposed CME in
Primary Care program. It has been provided as
a National Model that other countries may wish
to replicate.
The vision of <<the country>> is
“To Provide World Class Healthcare.”
One of the first steps to achieve this vision
is to start comprehensive educational programs
to improve the skills of the primary health
care team as Primary Health Care is essentially
the first level of contact of the patient with
the health care system. The suggested programs
include the following:
• Interdisciplinary Primary Care Training
Program. To assist medical centers in organizing
their delivery of care around the of primary
care principals.
• Primary Care Physician Education Initiative
(PCPEI). The goals of the educational intervention
are to better prepare current physicians to
deliver care under this new paradigm.
The aim of the above programs is to create
Family Medicine Model of Care at the primary
health care centers in <<the country>>
through a focus on excellence in health, wellness
and education; in a barrier free environment
that inspires interdisciplinary team approach,
accountability, trust, enthusiasm and pride.
In addition pave the way to excellence by challenging
the practitioner, maximizing professional fulfillment,
promoting research and creating an environment
of learning centering the focus of the program
on the patient, our clients.
Continuing
Medical
Education
(CME)
consists
of
educational
activities
which
serve
to
maintain,
develop
or
increase
the
knowledge,
skills,
and
professional
performance
and
relationships
that
a
physician
or
dentist
uses
to
provide
services
for
patients,
the
public
and
the
profession.
CME
ultimately
manifests
as
better
patient
care
and
better
patient
outcomes.
A
number
of
CME
activities
in
primary
health
care
are
active
within
the
regions
through
the
country’s
CME
department
consisting
of
lectures,
workshops,
activities
in
the
centers
as
well
as
regional
and
international
conferences.
A
lot
of
effort
has
been
done
to
encourage
the
health
care
providers
to
obtain
CME
through
the
official
requirement
of
50
CME
credit
per
physician
per
year
in
order
to
keep
his
license
valid.
However
there
is
a
need
for
establishing
structured
CME
programs.
Quality
Health
Care
requires
considerable
knowledge
and
skills
from
the
practitioners
combined
with
best
professional
attitudes.
Understanding
the
science
of
Medicine
and
its
clinical
effectiveness
are
moving
forward
rapidly
along
with
the
advancement
of
delivering
the
services.
The
knowledge
and
skills
of
the
practitioners
along
with
good
professional
attitudes
requires
updating
through
the
process
of
Continuing
Professional
Development.
It
is
now
well
accepted
that
a
multi-disciplinary
team
approach
is
the
best
way
forwards
for
providing
quality
health
care.
Need
Assessment
In
order
to
develop
a
comprehensive
educational
program
for
the
health
care
team
there
is
a
need
to
carry
extensive
need
assessment,
the
first
step
in
planning
an
educational
activity.
In
an
attempt
to
assess
the
needs
for
professional
development
of
the
medical,
dental
practitioners
and
nursing
staff
a
survey
was
conducted
by
means
of
a
Questionnaire
(APPENDIX
1)
by
the
Department
of
Health
for
<<the
country>>.
The
report
takes
into
account
a
wide
section
of
the
various
staff.
The
wide
range
of
topics
that
were
covered
in
the
survey
is
also
well
elaborated
in
the
report
included
the
following
Part
I-Demographic
Data
465
questionnaires
were
included
in
the
study
out
of
600
hundreds
distributed.
The
exclusion
criteria
were
that
either
the
questionnaire
was
not
returned
or
was
incomplete.
The
response
rate
was
77
percent.
The
mean
age
of
the
study
population
was
42years
(SD
9.70)
with
the
minimum
age
being
23
years
and
maximum
being
74years.
72%
of
the
study
populations
were
below
50
years.
The
mean
of
the
number
of
years
since
graduation
was
18
years
(mean
=8.46,
SD=9.16).
Whereas
the
mean
of
the
number
of
years
in
practice
was
17
years
(Mean=17.18,
SD=9.16).
As
for
gender
distribution
35%
of
the
samples
were
males
vs
65%
who
were
females.
| CME
TOPICS
FOR
PHYSICIANS |
The
response
to
the
various
topics
in
medicine
is
presented
in
the
Tables
in
the
report.
The
topics
that
received
the
highest
rating
were:
1.
Doctor
patient
relationship
2.
How
to
order
diagnostic
tests
3.
Diabetes
mellitus,
thyroid
disorders,
Obesity,
Hyperlipidemia,
chest
pain,
hypertension,
abdominal
pains,
asthma,
dyspnoea,
cerebrovascular
accidents,
epilepsy,
arthritis,
back
pain,
anxiety,
UTI,
fever
of
unknown
origin,
infection
control,
anaemias,
vertigo
&
dizziness,
red
eye,
medical
problems
&
drugs
in
pregnancy,
skin
infections,
ECG,
evaluation
of
breasts
lumps,
sprains,
Basic
&
advanced
life
support,
4.
Pediatrics-
growth
&
developmental
disorders,
nutrition,
otitis
media,
immunization
schedule
Format
of
CME
The
response
rate
for
the
monthly
activity
was
the
highest
with
Hands
–
workshops.
In
<<the
country>>
it
is
clear
that
there
is
a
definite
need
for
improvement.
All
current
physicians
within
the
primary
health
care
setting
will
participate
in
the
PCPEI
and
DCPEI
project
to
upgrade
their
skills.
In
addition
there
is
a
need
to
improve
and
train
people
responsible
for
CME
and
CPD
activities
and
faculty
development
is
necessary
to
ensure
effective
team
teaching
approaches,
interdisciplinary
collaboration,
integration
of
material
across
disciplines
and
courses,
and
focus
on
patient
health
outcomes.
The
integration
of
these
concepts
needs
to
be
across
the
curriculum
and
in
every
course
rather
than
adding
additional
curricular
time.
Faculty
development
for
role
modeling
and
mentoring
techniques
should
be
considered.
The
response
rate
from
the
survey
was
relatively
high,
reflecting
the
interest
of
the
primary
health
care
team
in
CME
and
CPD.
There
are
a
number
of
Barriers
to
obtaining
optimal
CME
including
lack
of
time
and
type
of
activities
which
include:
Lack
of
time,
Motivation
and
fatigue,
Distance,
availability
and
cost.
It
is
clear
that
looking
at
tables
in
the
report
that
the
respondents
rated
the
importance
of
topics
according
to
their
level
of
knowledge.
It
is
an
important
concept
that
revealed
that
the
less
knowledge
they
have
about
a
topic
was
reflected
by
less
score
on
rate
of
importance.
Therefore
in
planning
CME
programs
this
should
be
taken
into
account.
Assessment
Strategies
In
the
implementation
of
any
CME
activities
assessment
strategies
is
critical
to
judge
the
success
of
such
a
program.
For
example
communication
skills
learning
must
be
both
formative
and
summative.
The
knowledge,
skills,
and
attitudes
to
be
assessed
must
be
made
explicit
to
both
learners
and
teachers
alike.
Potential
evaluators
include
local
experts,
course
faculty,
simulated
and
real
patients,
peers,
and
the
learners
themselves.
Formative
assessment
should
occur
throughout
the
communication
skills
curriculum
and
is
intended
to
shape
and
improve
future
behaviors.
Assessment
of
communication
skills
must
include
direct
observation
of
performance.
Evaluation
of
setting
a
therapeutic
environment,
gathering
data
and
providing
information
and
closure
must
be
included.
Evaluation
of
advanced
skills,
including
use
of
interpreters,
providing
bad
news
and
promoting
behavior
change
should
be
done
as
well.
Criteria
should
match
the
novice
level
of
the
end
of
second
year
student,
who
should
be
able
to
identify
the
critical
issues
for
effective
communication
and
perform
the
skills
under
straightforward
circumstances.
It
will
be
as
well
a
good
idea
to
create
a
department
of
Family
Medicine
under
the
umbrella
of
<<the
country>>
that
helps
coordinate
the
implementation
of
the
different
educational
program,
in
addition
to
conducting
a
number
of
ongoing
research
and
academic
activities.
Quality
CME
can
enhance
the
knowledge
base
and
practice
skills
of
the
participating
health
care
provider
and
is
increasingly
used
as
part
of
the
credentialing
and
reappointment
process.
Continuing
Medical
Education
is
important
not
only
as
a
requirement
for
practice,
but
as
means
for
the
profession
to
achieve
one
of
its
primary
goals:
QUALITY
PATIENT
CARE.
To
our
patients
CME
requirements
are
a
commitment
made
by
the
medical
and
dental
practitioner
to
keep
our
knowledge
and
skills
current.
CME
really
is
about
changing
behavior
through
education–about
doing
something
different,
doing
it
better.”
It
is
critical
to
look
at
CME
and
CPD
in
the
mentality
of
21st
century.
We
attempted
to
clearly
present:
that
the
patient’s
concerns,
values
and
outcomes
must
be
the
center
of
care;
that
partnering
with
an
activated
patient
is
essential;
that
self-awareness
is
essential
in
being
an
effective
physician;
that
improving
the
process
of
care
and
health
outcomes
is
the
physician’s
responsibility
and
requires
a
systems
approach.
Quality
CME
can
enhance
the
knowledge
base
and
practice
skills
of
the
participating
health
care
provider
and
is
increasingly
used
as
part
of
the
credentialing
and
reappointment
process.
Continuing
Medical
Education
is
important
not
only
as
a
requirement
for
practice,
but
as
means
for
the
profession
to
achieve
one
of
its
primary
goals:
QUALITY
PATIENT
CARE.
To
our
patients
CME
requirements
are
a
commitment
made
by
the
medical
practitioner
to
keep
our
knowledge
and
skills
current.
In
this
new
millennium
most
nations,
both
developed
and
developing
are
actively
reviewing
national
health
policies
and
strategies
as
well
as
health
delivery
systems.
The
over-riding
imperative
in
all
cases
is
to
deliver
quality
health
care
in
a
cost
efficient
manner
while
addressing
issues
of
access
and
equity.
The
provision
of
health
services
in
<<the
country>>
is
divided
into
federal,
local
and
private
sectors.
The
Health
Authority,
and
the
local
government
agency
is
responsible
for
the
provision
of
integrated,
comprehensive,
and
quality
of
health
services
for
its
population.
Primary
Health
Care
is
essentially
the
first
level
of
contact
with
the
health
care
system.
This
could
mean
seeing
the
family
doctor,
health
unit,
pharmacy,
or
clinic.
Or
it
could
mean
phoning
an
advice
line
staffed
by
health
professionals,
or
even
attending
a
self-care
workshop
to
learn
how
to
take
a
more
active
role
in
ones’
own
health.
Primary
health
care
involves
treating
short-term
health
problems,
managing
long-term
health
conditions
such
as
diabetes,
and
even
helping
to
learn
how
to
prevent
injury
and
illness.
Prevention
is
the
key
objective
of
primary
health
care.
When
properly
organized
and
coordinated,
primary
health
care
has
enormous
potential
to
introduce
improvements
in
the
health
system
leading
to
better
care,
shorter
waiting
lists,
improved
access
to
health
care
services,
and
a
more
sustainable
health
care
system.
The
definition
of
Primary
Care
in
terms
of
its
functions:
•
Integrated
and
accessible
healthcare
•
Services
provided
by
primary
care
clinicians,
generally
considered
to
be
physicians
and
nurse
practitioners,
but
involving
a
broader
array
of
individuals
in
a
primary
care
team
(nurses,
social
workers,
clinical
pharmacists,
dieticians)
•
Accountability
of
clinicians
and
systems
for
quality
of
care,
patient
satisfaction,
efficient
use
of
resources,
and
ethical
behaviour
•
The
majority
of
personal
healthcare
needs,
which
include
physical,
mental,
emotional,
and
social
concerns
•
A
sustained
partnership
between
patients
and
clinicians
•
Primary
care
in
the
context
of
family
and
community
At
the
time
a
primary
care
program
is
first
established
and
routinely
thereafter,
a
system
for
measuring
primary
care
needs
has
to
be
operational.
Indicators
of
how
well
primary
care
is
being
delivered
are
critical
to
guide
program
development,
implementation
and
refinement
and
must
be
regularly
communicated
to
providers
and
managers.
| PRIMARY
HEALTH
CARE
PROGRAM |
The
vision
is
“To
Provide
World
Class
Healthcare.”
One
of
the
first
steps
to
achieve
this
vision
is
to
start
comprehensive
educational
program
to
improve
the
skills
of
the
primary
health
care
team.
The
suggested
programs
include
the
following:
In
order
to
achieve
the
above
vision
number
of
large-scale
primary
health
care
projects
need
to
be
conducted
and
planned
under
Primary
Health
Care
Section.
One
important
aspect
of
the
program
will
be
comprehensive
educational
program
to
improve
the
skills
of
the
primary
health
care
team.
The
suggested
programs
include
the
following:
•
Interdisciplinary
Primary
Care
Training
Program.
To
assist
medical
centers
in
organizing
their
delivery
of
care
around
the
of
primary
care
principals.
•
Primary
Care
Physician
Education
Initiative
(PCPEI).
The
goals
of
the
educational
intervention
are
to
better
prepare
current
physicians
to
deliver
care
under
this
new
paradigm.
By
centering
the
focus
of
the
program
on
the
patient,
rather
than
who
provides
the
functions
and
services,
we
are
best
able
to
define
our
primary
care
program
as
the
provision
of
integrated,
accessible,
cost-effective
health
care,
wellness
and
preventative
services
through
interdisciplinary
teams.
These
teams
are
accountable
for
addressing
the
healthcare
needs
of
their
patients;
developing
a
sustained
partnership
with
their
patients
and
practicing
in
the
larger
context
of
family
and
community.
Medical
education
is
true
learning
where
those
who
attend
gain
knowledge,
apply
it
to
their
profession,
and
then
continue
to
practice
it.
It
is
reinforced
by
various
programs
that
they
participate
in,
or
reminder
systems
that
are
put
in
place,
so
that
their
behavior
changes
for
the
better,
which
ultimately
manifests
as
better
patient
care
and
better
patient
outcomes.
Continuing
Medical
Education
consists
of
educational
activities
which
serve
to
maintain,
develop
or
increase
the
knowledge,
skills,
and
professional
performance
and
relationships
that
a
physician
or
dentist
uses
to
provide
services
for
patients,
the
public
and
the
profession.
A
number
of
CME
activities
in
primary
health
care
are
active
within
the
regions
through
the
CME
department
and
include
lectures,
workshops,
activities
in
the
centers
as
well
as
regional
and
international
conferences.
A
lot
of
effort
has
been
done
to
encourage
the
health
care
providers
to
obtain
CME
through
the
official
requirement
of
50
CME
credit
per
physician
per
year
in
order
to
keep
his
license
valid.
However
there
is
a
need
for
establishing
structured
CME
programs.
Quality
Health
Care
requires
considerable
knowledge
and
skills
from
the
practitioners
combined
with
best
professional
attitudes.
Understanding
the
science
of
both
Medicine
&
Dentistry
and
their
clinical
effectiveness
are
moving
forward
rapidly
along
with
the
advancement
of
delivering
the
services.
The
knowledge
and
skills
of
the
practitioners
along
with
good
professional
attitudes
requires
updating
through
the
process
of
Continuing
Professional
Development.
It
is
now
well
accepted
that
a
multi-disciplinary
team
approach
is
the
best
way
forwards
for
providing
quality
health
care.
| PHYSICIANS
-
Clinically
Deficient |
A
physician
is
believed
to
be
clinically
deficient
when
the
following
factors
are
evidenced
by
the
inability
to
exercise
prudent
medical
judgment
and
the
inability
to
practice
with
reasonable
skills
and
safety
without
jeopardy
to
patient
care:
(a)
unethical
practices,
and/or
(b)
incompetent
(clinical
ineptitude)
These
factors
may
be
substantially
alleviated
through
education
and/or
behavioral
modification.
Need
Assessment
All
health
care
disciplines
share
a
common
and
primary
commitment
to
serving
the
patient
and
working
toward
the
ideal
of
health
for
all.
While
each
discipline
has
its
own
focus,
the
scope
of
health
care
mandates
that
health
professionals
work
collaboratively
and
with
other
related
disciplines.
Collaboration
emanates
from
an
understanding
and
appreciation
of
the
roles
and
contributions
that
each
discipline
brings
to
the
‘delivery
of
care
experience’.
Such
professional
socialization
and
ability
to
work
together
is
the
result
of
shared
educational
and
practice
experiences.
In
order
to
develop
a
comprehensive
educational
program
for
physicians,
dentists,
nurses
and
the
rest
of
the
health
care
team
there
is
a
need
to
carry
extensive
need
assessment.
Needs
assessment
is
the
first
step
in
planning
an
educational
activity.
Identification
of
needs
provides
the
basis
for
writing
activity
objectives.
Many
sources
may
be
used
to
establish
needs.
Physician
needs
may
be
determined
through
prior
activity
evaluations
and/or
surveys
of
individual
needs.
New
advances
in
a
clinical
treatment
may
be
identified
as
an
area
in
which
further
education
is
needed.
Needs
assessment
data
may
be
drawn
from
surveys
(on-site,
email,
Web
site),
focus
groups,
expert
consensus,
faculty
perception,
formal
or
informal
requests
from
physicians,
analyses
of
previous
evaluations,
epidemiological
data,
environmental
scans
including
literature
search/review,
and
quality
assurance/improvement
data
(e.g.,
gaps
between
practice
guidelines
and
practice
performance,
patient
safety/institutional
error
data,
and
information
from
external
entities
such
as
licensing
boards
or
certifying
agencies,
etc.).
It
might
seem
self
evident
that
the
need
to
learn
should
underpin
any
educational
system.
Indeed,
the
literature
suggests
that,
at
least
in
relation
to
continuing
professional
development,
learning
is
more
likely
to
lead
to
change
in
practice
when
needs
assessment
has
been
conducted,
the
education
is
linked
to
practice,
personal
incentive
drives
the
educational
effort,
and
there
is
some
reinforcement
of
the
learning.
On
the
other
hand,
basing
learning
in
a
profession
entirely
on
the
assessment
of
needs
is
a
dangerous
and
limiting
tactic.
So
a
balance
must
be
struck.
The
integration
of
needs
assessment,
education,
and
quality
assurance
of
the
service
is
stressed
.
Clinical
audit,
would
identify
practices
in
need
of
improvement
and
ensure
that
educational
and
organizational
interventions
were
made
to
address
these
needs.
Accordingly,
audit
was
described
as
“essentially
educational”
and
the
educational
process
surrounding
it
described.
In
adult
learning
principles
we
assume
that
learners
needed
to
feel
a
necessity
to
learn
and
that
identifying
one’s
own
learning
needs
was
an
essential
part
of
self
directed
learning.
In
medicine
a
doctor’s
motivation
to
learn
would
therefore
derive
from
needs
identified
during
his
or
her
experience
of
clinical
practice.
The
definition
of
Need
As
in
most
areas
of
education,
for
many
years
there
has
been
intense
debate
about
the
definition,
purpose,
validity,
and
methods
of
learning
needs
assessment.
It
might
be
to
help
curriculum
planning,
diagnose
individual
problems,
assess
student
learning,
demonstrate
accountability,
improve
practice
and
safety,
or
offer
individual
feedback
and
educational
intervention.
Published
classifications
include
felt
needs
(what
people
say
they
need),
expressed
needs
(expressed
in
action)
normative
needs
(defined
by
experts),
and
comparative
needs
(group
comparison).
Other
distinctions
include
individual
versus
organizational
or
group
needs,
clinical
versus
administrative
needs,
and
subjective
versus
objectively
measured
needs.
The
defined
purpose
of
the
needs
assessment
should
determine
the
methods
used
and
the
use
made
of
the
findings.
Exclusive
reliance
on
formal
needs
assessment
in
educational
planning
could
render
education
an
instrumental
and
narrow
process
rather
than
a
creative,
professional
one.
Methods
of
needs
assessment
Although
the
literature
generally
reports
only
on
the
more
formal
methods
of
needs
assessment,
doctors
use
a
wide
range
of
informal
ways
of
identifying
learning
needs
as
part
of
their
ordinary
practice.
These
should
not
be
undervalued
simply
because
they
do
not
resemble
research.
Questionnaires
and
structured
interviews
seem
to
be
the
most
commonly
reported
methods
of
needs
assessment,
but
such
methods
are
also
used
for
evaluation,
assessment,
management,
education,
and
now
appraisal
and
revalidation.
Learning
for
needs
The
main
purpose
of
needs
assessment
must
be
to
help
educational
planning,
but
this
must
not
lead
to
too
narrow
a
vision
of
learning.
Learning
in
a
profession
is
unlike
any
other
kind
of
learning.
Doctors
live
in
a
rich
learning
environment,
constantly
involved
in
and
surrounded
by
professional
interaction
and
conversation,
educational
events,
information,
and
feedback.
The
search
for
the
one
best
or
“right”
way
of
learning
is
a
hopeless
task,
especially
if
this
is
combined
with
attempting
to
“measure”
observable
learning.
Research
papers
show,
at
best,
the
complexity
of
the
process.
Multiple
interventions
targeted
at
specific
behavior
result
in
positive
change
in
that
behavior.
Exactly
what
those
interventions
are
is
less
important
than
their
multiplicity
and
targeted
nature.
On
the
other
hand,
different
doctors
use
different
learning
methods
to
meet
their
individual
needs.
For
example,
in
a
study
of
366
primary
care
doctors
who
identified
recent
clinical
problems
for
which
they
needed
more
knowledge
or
skill
to
solve,
55
different
learning
methods
were
selected.
The
type
of
problem
turned
out
to
be
the
major
determinant
of
the
learning
method
chosen,
so
there
may
not
be
one
educational
solution
to
the
identified
needs.
Much
of
a
doctors’
learning
is
integrated
with
their
practice
and
arises
from
it.
The
style
of
integrated
practice
and
learning
(“situated
learning”)
develops
during
the
successive
stages
of
medical
education.
The
components
of
apprenticeship
learning
in
postgraduate
training
are
made
up
of
many
activities
that
may
be
regarded
as
part
of
practice
(13).
Senior
doctors
might
also
recognize
much
of
their
learning
in
some
of
these
elements
and
could
certainly
add
more—such
as
conversations
with
colleagues.
Thus,
educational
planning
on
the
basis
of
identified
needs
faces
real
challenges
in
making
learning
appropriate
to
and
integrated
with
professional
style
and
practice.
The
first
step
is
to
recognize
the
need
of
learning
that
are
a
part
of
daily
professional
life
in
medicine
and
to
formalize,
highlight,
and
use
these
as
the
basis
of
future
recorded
needs
assessment
and
subsequent
planning
and
action,
as
well
as
integrating
them
with
more
formal
methods
of
needs
assessment
to
form
a
routine
part
of
training,
learning,
and
improving
practice.
Quality
health
care
for
patients
is
supported
by
maintenance
and
enhancement
of
clinical,
management
and
personal
skills.
The
knowledge
and
skills
of
practitioners
require
refreshment,
and
good
professional
attitudes
need
to
be
fostered
through
the
process
of
continuing
professional
development.
In
an
attempt
to
assess
the
needs
for
professional
development
of
the
medical,
dental
practitioners
and
nursing
staff
a
survey
was
conducted
by
means
of
a
Questionnaire
(APPENDIX
1)
by
the
Department
of
Primary
Health
Care.
This
report
takes
into
account
a
wide
section
of
the
various
medical,
dental
and
nursing
staff.
The
purposes
of
the
review,
therefore
were
to:
•
Determine
the
area
of
professional
development
•
Help
the
primary
care
physician,
meet
the
challenge
of
changes
in
the
structure
and
delivery
of
patient
care.
•
Encourage
more
reflection
on
practice
&
learning
needs,
including
more
forward
planning;
and
•
Make
the
educational
methods
used
in
practice
more
effective
The
topics
that
were
covered
in
the
survey
included
the
following
CME
TOPICS
FOR
PHYSICIANS
Family
Medicine
Concepts
Patient
Management
Skills
Critical
Appraisal
Internal
Medicine
-
Endocrinology
&
Metabolic
-
Cardiovascular
-
Gastroenterology
-
Pulmonary
-
Nephrology
-
Neurology
-
Rheumatology
-
Psychiatry
-
Genito
Urinary
-
Infections
Diseases
-
Hematology
Pediatrics
Otorhinolaryngology
Ophthalmology
Maternal
Health
Dermatology
Gerontology
Health
Promotion
and
Disease
Prevention
Diagnostic
Procedures
Therapeutic
Procedures
Special
Topics
Surgery
Emergency
Care
Format
of
CME
Timing
of
the
CME
Type
of
Activities
Self
Study
The
tables
following
represent
a
summary
of
the
data
collected.
Part
I-Demographic
data
465
questionnaires
were
included
in
the
study
out
of
600
hundreds
distributed.
The
exclusion
criteria
were
that
either
the
questionnaire
was
not
returned
or
was
incomplete.
The
response
rate
was
77
percent.
The
mean
age
of
the
study
population
was
42
years
(SD
9.70)
with
the
minimum
age
being
23
years
and
maximum
being
74years.
However
72%
of
the
sample
were
below
50
years.
The
mean
of
the
number
of
years
since
graduation
was
18
years
(
mean
=8.46,
SD=9.16).
Whereas
the
mean
of
the
number
of
years
in
practice
was
17
years
(Mean=17.18,
SD=9.16).
As
for
gender
distribution
35%
of
the
sample
were
males
vs
65%
who
were
females.
Looking
at
years
since
graduation
78
%
of
sample
had
graduated
for
more
than
ten
years,
42%
of
sample
more
than
twenty
years
ago
while
12%
of
sample
had
graduated
since
more
than
30
years.
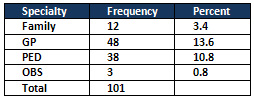
Looking
specifically
at
different
professions
of
the
study
population
and
specialty
only
3.4
percent
were
family
physicians
Table
1:
Current
Specialty
among
Physicians
Part
II:
CME
Topics
for
Physicians
The
response
to
the
various
topics
in
medicine
is
presented
in
Tables
4
to
Tables
29.
The
rating
for
each
topic
were:
(a)
In
order
of
importance
for
having
CME
on
the
topic
(1
=
least
important
to
5
=
most
important)
(b)
Current
level
of
knowledge
of
the
topic.
(1
=
basic
to
5
=
highly
skilled)
(c)
Recommend
CME
activity
on
level
of
priority.
(
1=least
to
5
=
highest
priority
)
Click
here
for
Tables
2-27
(CME
Topics
data)
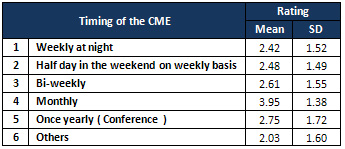
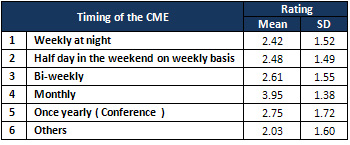
Attempt
was
made
to
establish
the
most
suitable
timings
and
frequency
of
the
CME
activities.
The
ratings
adopted
were
:
1
being
least
appropriate,
5
most
appropriate.
The
results
are
presented
below
and
the
need
for
a
monthly
activity
was
rated
highest
3.95
with
Hands-
on
Training
Table
28:
Timing
of
CME
Table
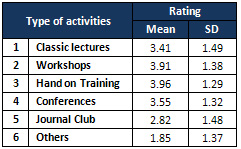
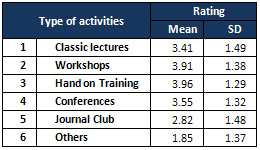
29:
Type
of
Activities
Table
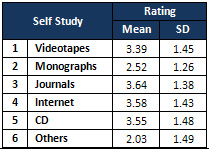
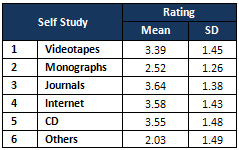
30:
Self
Study
Methods
There
is
little
disagreement
that
medical
education
is
a
continuum,
which
begins
prior
to
the
professional
school,
continues
through
the
four
or
five
years
of
medical
school,
into
graduate
education,
and
proceeds
throughout
the
physician’s/dentists’
lifespan
as
life-long
learning.
There
is
increasing
consensus
that
the
Accreditation
Council
for
Graduate
Medical
Education’s
(ACGME)
Outcome
Project,
with
its
defined
competency
structure,
is
driving
significant
changes
in
graduate
medical
education.
Given
the
continuum
of
medical
education
and
the
remarkable
congruency
of
all
the
broad-based
calls
for
medical
education
reform
with
the
ACGME
competency
structure.
In
the
area
of
Primary
health
care
it
is
clear
that
there
is
a
definite
need
for
improvement.
All
current
physicians
within
the
primary
health
care
setting
will
participate
in
the
project
to
upgrade
their
skills.
Overall
Evaluation
and
Need
for
Improvement
As
curricula
and
methodologies
for
the
training
of
physicians
approach
the
100-year
anniversary
of
the
Flexner
report
(2010),
it
is
important
to
recognize
that
medical
education
has
been
a
constantly
evolving
process
to
address
the
training
needs
of
physicians
to
serve
society
and
its
people.
Understanding
curricular
reform
is
one
of
understanding
its
history
Many
reports
prior
to
1990
(e.g.
Rappleye,
GPEP,
Macy
Foundation)
comment
on
the
process,
as
well
as
the
content
and
structure
of
medical
education.
Several
have
noted
the
glacial
progress
of
reform
and
the
reasons
behind
this
pace.
More
recently
in
the
1990s
and
the
new
century,
the
breadth
of
involved
stakeholders
in
this
process
has
widened,
as
many
entities
within
and
beyond
medical
schools
have
identified
significant
needs
in
the
process
of
education
of
physicians
for
the
21st
century.
These
defined
challenges
reflect
not
only
the
explosion
of
medical
knowledge
and
technology
and
the
changing
demographics
of
the
population,
but
also
the
broader
societal
and
health
care
system
changes
that
are
significantly
affecting
the
contextual
environment
in
which
medicine
is
practiced.
There
is
a
need
to
improve
and
train
people
responsible
for
CME
and
CPD
activities.
Traditional
educational
practice
in
medical
schools
emphasize
the
organ
systems
and
discipline-based
approaches,
but
in
Primary
Health
Care,
faculty
development
is
necessary
to
ensure
effective
team
teaching
approaches,
interdisciplinary
collaboration,
integration
of
material
across
disciplines
and
courses,
and
focus
on
patient
health
outcomes.
The
integration
of
these
concepts
needs
to
be
across
the
curriculum
and
in
every
course
rather
than
adding
additional
curricular
time.
Faculty
development
in
adult
education
techniques
may
be
necessary.
Faculty
development
for
role
modeling
and
mentoring
techniques
should
be
considered.
The
response
rate
from
the
survey
was
relatively
high,
reflecting
the
interest
of
the
primary
health
care
team
in
CME
and
CPD.
There
are
a
number
of
Barriers
to
obtaining
optimal
CME
including
lack
of
time
and
type
of
activities.
Lack
of
time
Lack
of
time
was
seen
as
the
biggest
barrier
to
obtaining
optimal
CME.
All
CME
was
carried
out
in
personal
time.
GPs
were
perceived
as
working
hard
and
long
hours.
Personal
time
is
precious.
‘It
means
night-time
or
weekends.
CME
activity
has
to
fit
in
with
on
call
and
family.
‘I
am
a
working
mother,
time
is
the
essence.’
In
our
survey
most
health
care
members
preferred
CME
activity
on
a
monthly
basis
which
reflects
that
time
is
precious
for
the
busy
primary
health
care
team.
(Table
31)
Table
31:
Timing
of
CME
Motivation
and
fatigue
were
other
barriers
to
CME.
Distance,
availability
and
cost
were
seldom
raised
as
issues
for
urban
GPs.
However,
distance
precluded
attendance
for
many
rural
practitioners,
as
did
difficulty
obtaining
locums,
cover
for
single
days,
availability
of
CME
and
financial
considerations.
The
perceived
challenge
was
to
increase
the
accessibility
of
personally-interactive
CME.
Type
of
Activities
A
number
of
studies
have
shown
preference
of
GPs
for
personal
interaction.
Some
studies
have
shown
a
preference
amongst
physicians
for
lectures
but
this
may
include
interaction.
Others
have
found
journals
the
most
popular
source
of
information
but
interactive
formats
were
still
highly
rated.
Preference
depends
on
the
type
and
quality
of
personal
experience
of
this
type
of
format.
Pendleton
differentiated
the
academic
and
professional
approach
to
CME.
He
postulated
that
the
academic
prefers
the
written
medium
and
the
clinician
prefers
face-to-face.
In
our
survey
the
respondents
preferred
the
most
hand
on
training,
workshop,
and
conferences.
Review
of
randomized
controlled
trials
on
CME
interventions
revealed
that
personal
interaction
to
be
central
to
effectiveness
in
change
in
practice.
Several
studies
have
reported
that
physicians
seek
confirmation
and
validation
of
current
and
new
medical
practices
through
their
peers.
Other
studies
have
confirmed
the
importance
of
interaction
in
changing
professional
behavior.
However,
it
has
not
been
established
which
elements
of
the
interactive
process
enable
learning.
Interaction
allows
for
clarification,
personalisation
of
information,
exploration,
feedback,
and
reflection.
It
can
also
address
other
needs
of
doctors
that
may
not
be
recognized
or
quantified
–
the
need
for
support,
recognition,
motivation
and
fulfillment,
and
the
‘need’
to
belong
to
a
professional
community.
As
for
self
study
methods
the
respondent
preferred
mostly
journals
followed
by
the
internet
followed
by
CD-Table
33
Table
32
:
Type
of
Activities
Table
33:
Self
Study
Methods
Interactive
formats
are
not
inherently
beneficial
nor
always
produce
change.
Some
formats
may
be
more
conducive
to
specific
changes
in
behavior
and
some
to
support.
Group
dynamics,
facilitation,
personal
agendas,
and
internal
and
external
influences
contribute
to
the
complexity
of
the
format.
In
general,
the
focus
was
on
choice
of
CME
as
opposed
to
other
elements
of
the
learning
cycle.
This
approach
has
been
documented
previously
and
reflects
the
traditional
approach
to
learning.
It
is
well
established
that
CME
should
follow
the
principles
of
androgogy
–
adult,
self-directed
learning.
The
term
‘androgogy’
has
been
coined
to
describe
the
learning
culture
appropriate
to
adult
education
.
Whereas
the
term
‘pedagogy’
describes
the
teacher-centred
approach
to
the
education
of
children,
androgogy
‘recognises
education
to
be
a
dynamic
lifelong
process’
that
‘is
learner-orientated’.
This
is
grounded
in
experiential
learning
–
identifying
and
addressing
needs
and
applying
learning
with
continuing
reflection.
Although
much
has
been
written
about
the
theory
and
benefits
of
this
model.
GPs
do
not
appear
to
adopt
it.
This
is
not
unique
to
GPs
–
a
study
of
physicians’
CME
found
that
‘unstructured
ad
hoc
reading
and
postgraduate
activities
predominate
over
methods
based
on
specific,
individual
needs
or
on
current
patient
problems’.
Some
GPs
in
our
study
did
recognise
that
tailoring
their
CME
to
their
identified,
specific
needs
was
better
than
the
opportunistic
approach,
but
few
attempted
this
in
any
structured
way.
Discussions
with
colleagues
one-to-one
and
in
small
groups
may
serve
as
an
informal
process
of
reflection,
even
though
the
benefits
may
not
be
easily
quantifiable.
The
process
of
reflecting
on
issues,
debating
problem
areas
and
formalising
opinions
may
be
helpful
to
the
clinician,
even
where
there
has
not
been
a
specific
updating
of
knowledge.
Lack
of
time
may
be
one
reason
GPs
have
not
embraced
the
adult
learning
model.
Clinical
experience
is
abundant
in
general
practice,
yet
many
may
be
too
busy
to
learn
from
it.
Lack
of
time
has
been
well
documented
as
a
significant
barrier
to
obtaining
optimal
CME,
a
finding
borne
out
strongly
in
this
study.
Perceived
high
workload
and
stress
lead
not
only
to
lack
of
time,
but
also
de-motivation.
Motivation
is
a
complex
issue,
however
one
role
of
CME
is
to
sustain
motivation.
GPs
may
not
be
very
good
at
identifying
their
needs
unassisted.
The
current
system
of
CME
credits
rewards
application
of
the
traditional
model,
one
of
updating
knowledge
and
skills,
with
no
focus
on
utilisation
of
the
adult
learning
cycle.
Without
evaluation
of
CME
undertaken,
GPs
are
likely
to
be
unaware
of
any
failings
of
the
current
system.
Few
tools
are
available
to
facilitate
this
process
of
reflection
and
evaluation.
Personal
development
plans
and
mentorship
have
been
suggested
but
need
to
be
evaluated.
Practical,
evidence-based,
user-friendly
ways
of
addressing
this
issue
are
awaited.
Most
doctors
want
to
improve
the
quality
of
their
action
as
painlessly
as
possible.
They
wish
to
maximise
the
return
on
their
investment
of
time
and
this
becomes
a
matter
of
cost-benefit
analysis
based
on
the
likely
yield
of
the
activity.
Personally
interactive
formats
are
costly
on
time,
especially
when
travelling
is
taken
into
consideration,
yet
most
GPs
prefer
these
formats.
Clearly
GPs
consider
time
spent
in
this
way
to
be
beneficial.
They
may
find
that
the
scheduled
nature
of
these
events
ensures
their
participation,
whereas
spending
the
equivalent
time
on
their
own
reading
or
accessing
the
Internet
may
require
more
personal
discipline.
CME
and
CPD
for
Physicians
Traditionally,
GPs
have
obtained
their
CME
through
didactic
lectures
and
written
material.
Although
these
mechanisms
may
increase
their
knowledge,
there
is
no
evidence
that
they
change
performance.
Recently,
there
has
been
a
move,
in
the
literature
at
least,
towards
application
of
the
Kolb
adult
learning
cycle:
identifying
learning
needs,
addressing
those
needs
and
evaluating
the
outcome,
with
reflection
inherent
in
the
process.
CME
is
undergoing
change
in
many
countries,
in
part
because
of
this
move.
Obtaining
views
regarding
CME
from
GPs
may
facilitate
this
change.
Proposed
changes
are
most
likely
to
succeed
when
compatible
with
existing
beliefs.
Most
GPs
do
not
direct
their
CME
according
to
the
adult
learning
model.
The
challenge
for
CME
providers
is
to
provide
avenues
to
facilitate
needs
identification
and
self-directed
learning.
It
is
clear
that
looking
at
table
4
and
7
showed
that
the
general
practitioners
rated
the
importance
of
topics
according
to
their
level
of
knowledge.
It
is
an
important
concept
that
revealed
that
the
less
knowledge
they
have
about
a
topic
was
reflected
by
less
score
on
rate
of
importance.
Therefore
in
planning
CME
program
this
should
be
taken
into
account
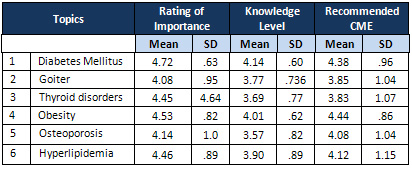
We
divided
the
level
of
importance
of
CME
into
three
categories
between
4.4
to
4.5,
between
4.5
to
4.6
and
above
4.6
CME
that
was
rated
between
4.4
to
4.5
1.
Doctor
Patient
relationship
2.
Hematuria
and
Proteinuria
3.
Urinary
Tract
Infection
4.
Fever
without
a
focus
5.
Normal
Growth
and
development
6.
Nutrition
7.
Development
Disorders
8.
Diarrheas
9.
Red
Eyes
10.
Skin
Infection
11.
Immunization
schedule
CME
that
was
rated
between
4.5
to
4.6
1.
Obesity
2.
Abdominal
Pain
3.
Headache
4.
Use
and
Abuse
of
Antibiotics
5.
Anemia
6.
Drugs
in
Pregnancy
7.
Electrocardiogram
8.
Advanced
Life
Support
CME
that
was
rated
above
4.6
1.
Diabetes
Mellitus
2.
Chest
Pain
3.
Hypertension
4.
Asthma
5.
Evaluation
of
Rash
6.
Basic
Life
Support
Click
here
for
Table
34:
Family
Medicine
Concepts
Table
35:
Endocrinology
&
Metabolic
| CURRICULUM
GUIDELINE
FOR
PRIMARY
CARE
PHYSICIAN
EDUCATION
INITIATIVE
|
CME
cannot
be
entirely
focused
on
GP
preference.
However,
it
is
clear
from
this
study
that
interactive
formats
were
generally
preferred
in
accordance
with
evidence
of
what
changes
GP
behaviour.
More
research
is
needed
into
which
elements
of
interactive
formats
facilitate
learning.
Most
GPs
are
not
directing
their
CME
according
to
the
adult
learning
model.
This
situation
needs
to
be
addressed,
bearing
in
mind
the
barriers
of
lack
of
time
and
motivation,
in
order
to
change
the
status
quo.
This
curriculum
guideline
drawn
from
existing
family
Medicine
Curriculum,
the
need
assessment,
and
clinical
protocol
being
developed
by
the
primary
health
care
clinical
guideline
committee
at
the
authority.
This
will
help
in
preparing
our
current
primary
care
physicians
to
understand
and
practice
with
family
medicine
spirit.
The
CME
program
will
include
a
matrix
structure,
including
family
medicine
principles,
family
medicine
themes,
and
the
competency
structure.
The
CME
Curriculum
will
focuses
on
clinical
competencies
necessary.
The
competencies
were
identified
through
the
consensus
of
experienced
educators
from
the
primary
care
disciplines
and
need
assessment.
The
CCP
has
two
components:
an
overall
compendium
of
suggested
competencies
and
a
delineation
of
6
priority
areas
The
PCPEI
Matrix
incorporates:
•
Six
ACGME
competencies
•
Five
Family
Medicine
Principles
-
Values
that
define
the
profession,
which
should
guide
our
educational
activities.
o
Context
of
Care
o
Continuity
of
Care
o
Comprehensive
Care
o
Coordination
of
Care
o
Biopsychosocial
Approach
•
Three
Family
Medicine
Clerkship
Themes
-
Contexts
in
which
FM
delivers
care.
o
Prevention
and
Wellness
o
Acute
and
Chronic
Illness
o
Community
and
Population
Medicine
•
Family
Medicine
Topic
Areas-
derived
from
the
need
assessment
•
Clinical
protocols
developed
for
primary
health
care
•
Special
topics
of
interest
•
End-of-life
and
palliative
care
•
Geriatrics
•
Genetics
Patient
Care
that
is
compassionate,
appropriate,
and
effective
for
the
treatment
of
health
problems
and
the
promotion
of
health
Medical
Knowledge
about
established
and
evolving
biomedical,
clinical,
and
cognate
(e.g.
epidemiological
and
social-behavioral)
sciences
and
the
application
of
this
knowledge
to
patient
care
Practice-Based
Learning
and
Improvement
that
involves
investigation
and
evaluation
of
their
own
patient
care,
appraisal
and
assimilation
of
scientific
evidence,
and
improvements
in
patient
care
Interpersonal
and
Communication
Skills
that
result
in
effective
information
exchange
and
teaming
with
patients,
their
families,
and
other
health
professionals
Professionalism,
as
manifested
through
a
commitment
to
carrying
out
professional
responsibilities,
adherence
to
ethical
principles,
and
sensitivity
to
a
diverse
patient
population
Systems-Based
Practice,
as
manifested
by
actions
that
demonstrate
an
awareness
of
and
responsiveness
to
the
larger
context
and
system
of
health
care
and
the
ability
to
effectively
call
on
system
resources
to
provide
care
that
is
of
optimal
value
CME
topics
rated
above
4.4
by
respondents
Diabetes
Mellitus
Chest
Pain
Hypertension
Asthma
Evaluation
of
Rash
Basic
Life
Support
Doctor
Patient
relationship
Hematuria
and
Proteinuria
Urinary
Tract
Infection
Fever
without
a
focus
Normal
Growth
and
development
Nutrition
Development
Disorders
Diarrheas
Red
Eyes
Skin
Infection
Immunization
schedule
Obesity
Abdominal
Pain
Headache
Use
and
Abuse
of
Antibiotics
Anemia
Drugs
in
Pregnancy
Electrocardiogram
Advanced
Life
Support
The
Alphabetical
list
of
clinical
guidelines
Acne,
Management
of
Acute
Coronary
Syndrome
and
Chest
Pain;
Diagnosis
and
Treatment
of
Ankle
Sprain
Anticoagulation
Therapy
Supplement
Asthma,
Diagnosis
and
Outpatient
Management
of
Asthma,
ER
and
Inpatient
Management
of
Atrial
Fibrillation
Attention
Deficit
Hyperactivity
Disorder
in
Primary
Care
for
School
Age
Children
and
Adolescents,
Diagnosis
and
Management
of
Breast
Cancer
Treatment
Breast
Disease,
Diagnosis
of
Cardiac
Stress
Test
Supplement
Cervical
Cancer
Screening
Chronic
Obstructive
Pulmonary
Disease
Colorectal
Cancer
Screening
Coronary
Artery
Disease,
Stable
Degenerative
Joint
Disease
of
the
Knee,
Adult;
Diagnosis
and
Treatment
of
Depression,
Major,
in
Adults
for
Mental
Health
Care
Providers
Depression,
Major,
in
Adults
in
Primary
Care
Diabetes
Mellitus,
Type
2;
Management
of
Domestic
Violence
Dyspepsia
&
GERD
Headache,
Diagnosis
and
Treatment
of
Heart
Failure
in
Adults
Hypertension
Diagnosis
and
Treatment
Immunizations
Infertility,
Diagnosis
and
Management
of
Labor,
Management
of
Lipid
Management
in
Adults
Lipid
Screening
in
Adults
Lipid
Screening
in
Children
and
Adolescents
Low
Back
Pain,
Adult
Menopause
and
Hormone
Therapy
(HT):
Collaborative
Decision-Making
and
Management
Obesity;
Prevention
and
Management
of
(Mature
Adolescents
and
Adults)
Osteoporosis,
Diagnosis
and
Treatment
of
Otitis
Media
in
Children,
Diagnosis
and
Treatment
of
Pain,
Acute,
Assessment
and
Management
of
Pain,
Chronic,
Assessment
and
Management
of
Pap
Smear,
Initial
Abnormal;
Management
of
Pharyngitis,
Acute
Pneumonia,
Community-Acquired
Prenatal
Care,
Routine
Stroke,
Ischemic,
Diagnosis
and
Initial
Treatment
of
Tobacco
Use
Prevention
and
Cessation
for
Adults
and
Mature
Adolescents
Tobacco
Use
Prevention
and
Cessation
for
Infants,
Children
and
Adolescents
Urinary
Tract
Infection
in
Women,
Uncomplicated
Venous
Thromboembolism
(formerly
DVT)
Venous
Thromboembolism
Prophylaxis
Stroke,
Ischemic,
Diagnosis
and
Initial
Treatment
of
Tobacco
Use
Prevention
and
Cessation
for
Adults
and
Mature
Adolescents
Tobacco
Use
Prevention
and
Cessation
for
Infants,
Children
and
Adolescents
Urinary
Tract
Infection
in
Women,
Uncomplicated
Venous
Thromboembolism
(formerly
DVT)
Venous
Thromboembolism
Prophylaxis
Viral
Upper
Respiratory
Infection
(VURI)
in
Adults
and
Children
| CLINICAL
PROTOCOLS
FOR
PRIMARY
HEALTH
CARE
|
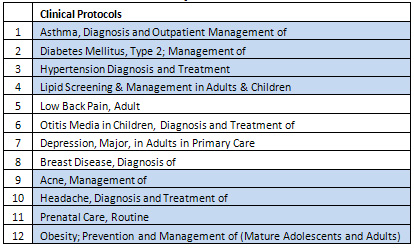
Building
on
the
above
resources
mainly
the
need
assessment,
the
Clinical
protocols
developed
for
primary
health
care,
the
six
ACGME
competencies
,
the
five
Family
Medicine
Principles
,
special
topics
of
interest,
and
the
Three
Family
Medicine
Clerkship
Themes,
We
recommend
a
CME,
CPD
program
that
cover
the
Topics
below
over
a
period
of
two
years.Protocols
to
be
developedAsthma,
Diagnosis
and
Outpatient
Management
of
Diabetes
Mellitus,
Type
2;
Management
of
Hypertension
Diagnosis
and
Treatment
Screening
and
Management
of
Dyslipidemia
Low
Back
Pain,
Adult
Otitis
Media
in
Children,
Diagnosis
and
Treatment
of
Depression,
Major,
in
Adults
in
Primary
Care
Breast
Disease,
Diagnosis
of
Acne,
Management
of
Headache,
Diagnosis
and
Treatment
of
Prenatal
Care,
Routine
Obesity;
Prevention
and
Management
of
(Mature
Adolescents
and
Adults)
Ankle
Sprain
Degenerative
Joint
Disease
of
the
Knee,
Adult;
Diagnosis
and
Treatment
of
Sleep
Apnea,
Diagnosis
and
Treatment
of
Obstructive
Attention
Deficit
Hyperactivity
Disorder
in
Primary
Care
for
School
Age
Children
and
Adolescents,
Diagnosis
and
Management
of
Immunizations
Stroke,
Ischemic,
Diagnosis
and
Initial
Treatment
of
Chronic
Obstructive
Pulmonary
Disease
Coronary
Artery
Disease,
Stable
Heart
Failure
in
Adults
Atrial
Fibrillation
Acute
Coronary
Syndrome
and
Chest
Pain;
Diagnosis
and
Treatment
of
Dyspepsia
&
GERD
Domestic
Violence
Menopause
and
Hormone
Therapy
(HT):
Collaborative
Decision-Making
and
Management
Pap
Smear,
Initial
Abnormal;
Management
of
Cervical
Cancer
Screening
Infertility,
Diagnosis
and
Management
of
Pain,
Acute,
Assessment
and
Management
of
Pain,
Chronic,
Assessment
and
Management
of
Preventive
Counseling
and
Education
Preventive
Risk
Assessment
Forms
Preventive
Services
for
Adults
Preventive
Services
for
Children
and
Adolescents
Colorectal
Cancer
Screening
Osteoporosis,
Diagnosis
and
Treatment
of
Rhinitis
Sinusitis
in
Adults,
Acute
Urinary
Tract
Infection
in
Women,
Uncomplicated
Viral
Upper
Respiratory
Infection
(VURI)
in
Adults
and
Children
Pharyngitis,
Acute
Pneumonia,
Community-Acquired
Preoperative
Evaluation
Anticoagulation
Therapy
Supplement
Venous
Thromboembolism
(formerly
DVT)
Venous
Thromboembolism
Prophylaxis
Sleep
Apnea,
Diagnosis
and
Treatment
of
Obstructive
Tobacco
Use
Prevention
and
Cessation
for
Adults
and
Mature
Adolescents
Tobacco
Use
Prevention
and
Cessation
for
Infants,
Children
and
Adolescents
Topics
that
of
importance
identified
in
the
Need
Assessment
Survey
and
not
matched
to
the
clinical
guidelines
and
protocols
being
developed
Evaluation
of
Rash
Basic
Life
Support
Doctor
Patient
relationship
Hematuria
and
Proteinuria
Fever
without
a
focus
Normal
Growth
and
development
Nutrition
Development
Disorders
Diarrheas
Red
Eyes
Skin
Infection
Abdominal
Pain
Use
and
Abuse
of
Antibiotics
Anemia
Drugs
in
Pregnancy
Electrocardiogram
Advanced
Life
Support
Other
Topics
from
other
sources
Patient
Care
Practice-Based
Learning
and
Improvement
Interpersonal
and
Communication
Skills
Professionalism,
Community
and
Population
Medicine
End-of-life
and
palliative
care
Geriatrics
Genetics
Informatics
Substance
abuse
Mental
health
Bioterrorism
Arthritis
/
Arthralgia
Cancer
Screening
Cultural
Competence
Dementia
Anxiety
Fatigue
Frailty
Skin
Problems
Strains
/
Sprains
Menstrual
Disorders
Nutrition
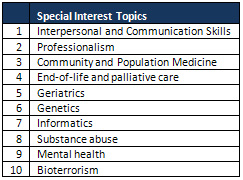
Quality
CME
can
enhance
the
knowledge
base
and
practice
skills
of
the
participating
health
care
provider
and
is
increasingly
used
as
part
of
the
credentialing
and
reappointment
process.
Continuing
Medical
Education
is
important
not
only
as
a
requirement
for
practice,
but
as
means
for
the
profession
to
achieve
one
of
its
primary
goals:
QUALITY
PATIENT
CARE.
To
our
patients
CME
requirements
are
a
commitment
made
by
the
medical
practitioner
to
keep
our
knowledge
and
skills
current.
Learning
in
medicine
occurs
across
a
continuum,
from
the
life
experience
gained
prior
to
beginning
medical
school,
through
the
traditional
four
years
of
medical
student
education,
through
professional
residency
/fellowship
training
and
continually
through
one’s
professional
career.
Practice
based
learning
is
important
within
the
context
of
primary
health
care.
Each
member
of
the
team
should
be
prepared
to
manage
their
learning
about
their
patients’
problems
with
minimal
direction
from
the
attending
physician,
residents,
or
other
physicians
on
the
rotation.
This
self-directed
learning
will
require
a
commitment
to
assessing
one’s
own
needs
for
learning,
an
ability
to
identify
the
types
of
information
pertinent
to
the
care
of
their
patients
(e.g.,
physical
examination
findings,
diagnostic
testing,
treatment
options,
medication
side-effects,
diagnostic
and
therapeutic
procedures),
a
listing
of
perceived
gaps
in
knowledge
in
those
areas,
and
a
strategy
for
finding
and
assessing
the
necessary
information.
To
search
for
information,
the
student
will
need
to
be
able
to
identify
up-to-date
information
through
on-line
resources.
Assessing
information
will
depend
on
an
ability
to
assess
the
validity
of
evidence
in
clinical
guidelines,
reviews,
and
studies
about
diagnosis
or
treatment
of
disease.
The
primary
health
care
team
must
be
committed
and
able
to
appraise
and
assimilate
scientific
evidence
for
improvement
of
patient
care
practices.
•
Demonstrate
commitment
to
personal
role
in
providing
healthcare
outcomes.
•
Effectively
employ
recursive
strategy
for
life-long
learning.
•
Learn
to
direct
own
learning
about
patient’s
problems.
•
Learn
to
locate,
appraise,
and
assimilate
evidence
from
clinical
guidelines,
systematic
reviews,
and
articles
related
to
patients’
problems.
•
Learn
to
apply
knowledge
of
study
designs
and
statistical
methods
to
appraise
information
about
diagnostic
tests
and
therapeutic
interventions.
In
the
implementation
of
any
CME
activities
assessment
strategies
is
critical
to
judge
the
success
of
such
a
program.
For
example
communication
skills
learning
must
be
both
formative
and
summative.
The
knowledge,
skills,
and
attitudes
to
be
assessed
must
be
made
explicit
to
both
learners
and
teachers
alike.
Potential
evaluators
include
local
experts,
course
faculty,
simulated
and
real
patients,
peers,
and
the
learners
themselves.
Formative
assessment
should
occur
throughout
the
communication
skills
curriculum
and
is
intended
to
shape
and
improve
future
behaviors.
This
requires
direct
observation
(in
person
or
videotaped)
of
the
skills
during
role-play
activities,
with
standardized
patients,
and
with
real
patients.
The
feedback
provided
should
be
balanced
and
nonjudgmental.
Self-assessment
during
the
learning
process
should
be
encouraged.
Assessment
of
communication
skills
must
include
direct
observation
of
performance.
Evaluation
of
setting
a
therapeutic
environment,
gathering
data
and
providing
information
and
closure
must
be
included.
Evaluation
of
advanced
skills,
including
use
of
interpreters,
providing
bad
news
and
promoting
behavior
change
should
be
done
as
well.
Criteria
should
match
the
novice
level
of
the
end
of
second
year
student,
who
should
be
able
to
identify
the
critical
issues
for
effective
communication
and
perform
the
skills
under
straightforward
circumstances.
Specific
tools
can
be
chosen
from
among
the
following:
•
Standardized
patients
•
OSCE’s
•
Observed
performance
with
patients
and
others
•
Written
reflections
describing
how
a
learner
would
approach
a
certain
situation
•
MCQ’s
It
is
critical
that
some
of
the
CME
and
CPD
occur
at
the
clinical
setting.
The
characteristics
of
the
ideal
clinical
teaching
setting
were
described
as
follows:
•
The
care
of
patients
should
be
continuous
and
not
limited
by
the
duration,
severity,
or
type
of
illness,
or
by
the
patient’s
age
or
gender.
•
The
patient
population
should
reflect
the
ethnic
and
socioeconomic
mix
of
the
community
at
large
as
closely
as
possible
and
should
be
sufficient
in
volume
to
provide
diversity
in
patient
encounters.
•
The
care
provided
should
be
community-based
(that
is,
where
care
follows
the
need
and
the
setting
most
suited
to
the
patient,
not
just
the
practice)
and
should
occur
wherever
most
appropriate
for
the
patient,
including
the
home,
office,
nursing
home,
hospital,
or
extended
care
facility.
•
The
care
of
patients
should
include
consideration
of
family,
occupation,
social
support,
resources,
and
ethnicity,
and
be
customized
according
to
the
patient’s
needs
and
values.
•
The
faculty
should
be
trained
for,
educated
for,
and
involved
in
the
practice
of
family
medicine.
We
need
as
well
to
apply
the
New
Model
of
Family
Medicine
Care
where,
family
medicine
care
(and
teaching)
will
occur
in
a
dramatically
changed
environment.
Characteristics
of
the
New
Model
of
family
medicine
include:
•
A
patient-centered
team
approach;
•
Elimination
of
barriers
to
access;
•
Advanced
information
systems,
including
an
•
Electronic
health
record;
•
Redesigned,
more
functional
offices;
•
A
focus
on
quality
and
outcomes;
•
And
enhanced
practice
finance.
In
order
to
be
able
to
achieve
the
above
we
need
certain
Characteristics
of
faculty
to
train
physicians
in
this
new
environment:
•
The
faculty
should
be
trained
and
current
in
use
of
technology
at
the
point
of
care
with
patients.
The
setting
should
provide
access
to
web-based
learning
resources
with
access
to
the
Internet
for
all
students.
•
The
faculty
should
be
self-aware
individuals
who
can
demonstrate
and
role
model
life-long
learning
principles
in
their
routine
every-day
care
of
patients.
•
Faculty
diversity
will
reflect
the
diversity
in
the
patient
population
served
at
the
setting
where
student
clinical
training
occurs.
Community
clinical
teaching
sites
in
the
family
medicine
clerkship
provide
a
unique
learning
experience
for
all
medical
students.
Preserving
and
nurturing
these
teaching
settings
is
the
key
to
teaching
a
new
generation
of
student
physicians
the
“New
Model”
for
family
medicine.
Evaluation
of
Patient
Care
requires
utilization
of
multiple
techniques
to
address
knowledge,
skills
and
attitudes
of
future
physicians.
Direct
observation
is
the
key
to
evaluation
of
many
of
the
skills
outlined
above.
This
is
an
area
where
faculty
have
decreased
their
involvement
as
pressures
in
other
aspects
of
their
roles
have
increased.
Faculty
must
return
to
this
foundational
method
of
monitoring
the
growth
and
development
of
patient
care
skills.
Videotaping
of
patient
encounters
and
standardized
patient
evaluation
are
methods
that
enable
assessment
of
patient
care
skills.
Structures
within
the
curriculum
must
be
developed
that
encourage
systematic
feedback
to
physicians
about
patient
care
knowledge,
skills,
and
attitudes.
All
sources
of
input
are
viable,
but
the
key
is
formative
and
summative
evaluations
by
clinical
preceptors.
Medical
knowledge
is
of
ultimate
importance
and
assessment
should
be
highly
visible
and
very
high
stakes
based
on
explicit
expectations
of
students.
Evaluation
will
require
utilization
of
multiple
techniques
to
address
knowledge,
skills
and
attitudes.
Videotaping
of
patient
encounters
and
standardized
patient
evaluations,
participation
in
small
group
discussions,
oral
and
written
examinations,
tests
for
specific
examination
skills,
observations
during
patient
care,
Socratic
questioning
of
individual
physicians,
and
structured
opportunities
for
individual
and
group
reflection
are
all
methods
that
can
be
used.
The
knowledge,
skills,
and
attitudes
of
Practice-Based
Learning
and
Improvement
are
best
learned
in
an
interactive
environment
where
a
variety
of
teaching
strategies
are
used
to
facilitate
physicians
learning.
Basic
knowledge
can
be
transmitted
through
lectures,
computer-assisted
instruction
(such
as
web-based
curricula),
or
readings,
but
understanding
and
applying
the
material
to
actual
patient
care
problems
is
best
accomplished
through
problem-based
methods
using
small
group
experiences
and
active
participation
and
problem
solving.
The
full
application
of
Practice-Based
Learning
and
Improvement
requires
an
on-going
clinical
practice
with
information
systems
that
allow
retrieval
of
practice
information
and
data
from
patient
records.
Faculty
development
should
be
focused
on
increasing
knowledge
about
evidence-based
medicine,
clinical
epidemiology,
and
print
and
electronic
sources
for
reviews
and
guidelines.
However,
often
there
is
faculty
resistance
to
application
of
the
concepts
of
evidence-based
medicine,
clinical
epidemiology,
and
quantitative
approaches
to
decision-making,
because
they
are
sometimes
viewed
as
counter-intuitive,
impractical,
and
undermining
the
“art
of
medicine”
as
well
as
physician
discretion
to
individualize
patient
care.
Faculty
skill
development
is
critical
in
this
area,
especially
skills
in
problem-based
or
case-based
teaching
strategies,
small
group
instruction,
and
methods
of
quick
access
to
information
through
the
WWW
or
hand-held
devices.
| FACULTY
MEMBERS
TEACHING
THE
CURRICULUM
|
Faculty
members
do
not
need
to
be
expert
in
any
of
these
special
topic
areas
to
be
highly
effective
teachers.
There
may
even
be
benefit
in
a
teacher
appearing
to
be
a
non-expert,
yet
a
“champion”
for
the
topic.
Physicians
need
to
understand
that
a
basic
level
of
mastery
in
such
a
topic
is
an
essential
component
of
every
physician’s
practice.
A
teacher
who
shows
expertise
only
in
one
specific
area
may
represent
an
unattainable
or
even
undesirable
role
model.
A
champion
who
demonstrates
a
broad
range
of
competence
with
a
variety
of
patient
problems,
and
conveys
both
enthusiasm
and
a
solid
understanding
of
a
topic,
can
serve
as
an
ideal
role
model.
A
champion
conveys
an
essential
enthusiasm
to
students.
Clearly,
all
teachers
cannot
be
champions
for
all
topics;
rather,
programs
may
want
to
identify
faculty
members
with
enthusiasm
for
one
or
more
of
the
various
topics
areas
and
then
support
those
champions
in
the
development
and
implementation
of
these
curricular
topics.
Adult
Learning
Principles
In
addition
to
being
“champions,”
teachers
need
to
employ
principles
of
adult
learning
in
their
approach
to
teaching
these
topics.
The
knowledge
base
for
any
of
these
topics
is
changing
every
day
with
the
information
and
technology
explosion
that
has
occurred
in
the
last
quarter-century.
Genetics
is
a
perfect
example
of
a
topic
subject
to
rapid,
ongoing
revision
based
upon
new
research
findings.
Physicians
must
learn
how
to
identify
their
own
learning
needs
and
address
these
needs
effectively,
in
order
to
keep
up
with
the
ever-advancing
knowledge
base
in
most
of
these
topic
areas.
Self-Awareness
In
addition
to
fostering
an
enthusiastic
approach
to
lifelong
learning,
the
instructional
method
must
encourage
physicians
to
reflect
upon
their
own
lives
in
relationship
to
the
topic.
The
topic
of
geriatrics,
for
example,
emphasizes
many
issues
that
every
student
will
face,
through
the
aging
of
parents
and
themselves.
Substance
abuse,
end-of-life,
and
other
topics
often
elicit
strong
emotions
within
students,
as
physicians
remember
past
experiences
or
recognize
ongoing
struggles
within
their
own
lives.
Teachers
must
create
environments
that
are
safe
enough
to
foster
trust
and
intimacy,
and
yet
challenge
physicians
to
reflect
upon
their
own
experience
of
life,
as
they
develop
a
basic
level
of
mastery
in
these
special
topic
areas.
CME
really
is
about
changing
behavior
through
education–about
doing
something
different,
doing
it
better.”
The
bottom
line
of
CME
in
the
past
has
been
the
activities
we
produced—how
many,
how
much
they
cost,
how
many
people
came.
In
essence,
CME
was
more
activity-oriented
than
learner-oriented.
“Not
only
do
you
have
to
focus
on
the
learner,”
“you
have
to
focus
on
the
learner
in
the
context
in
which
they
are
learning,
which
is
the
healthcare
environment
where
they
practice
medicine.”
The
aim
of
the
proposal
is
to
‘to
provide
leadership
in
the
delivery
of
high
quality
education,
for
the
primary
care
team,
in
the
context
of
a
caring
and
vibrant
academic
environment’
It
is
critical
to
look
at
CME
and
CPD
in
the
mentality
of
21st
century.
We
attempted
to
clearly
present:
that
the
patient’s
concerns,
values
and
outcomes
must
be
the
center
of
care;
that
partnering
with
an
activated
patient
is
essential;
that
self-awareness
is
essential
in
being
an
effective
physician;
that
improving
the
process
of
care
and
health
outcomes
is
the
physician’s
responsibility
and
requires
a
systems
approach.
In
conclusion,
GPs
in
this
study
displayed
a
strong
preference
for
personally
interactive
formats
and
non-interactive
formats
were
viewed
as
adjunctive.
What
this
demonstrates
is
the
value
GPs
place
on
personal
contact
with
their
colleagues,
despite
the
added
demand
this
places
on
their
time.
Quality
CME
can
enhance
the
knowledge
base
and
practice
skills
of
the
participating
health
care
provider
and
is
increasingly
used
as
part
of
the
credentialing
and
reappointment
process.
Continuing
Medical
Education
is
important
not
only
as
a
requirement
for
practice,
but
as
means
for
the
profession
to
achieve
one
of
its
primary
goals:
QUALITY
PATIENT
CARE.
To
our
patients
CME
requirements
are
a
commitment
made
by
the
medical
and
dental
practitioner
to
keep
our
knowledge
and
skills
current.
|
|
.................................................................................................................

|
| |
|

