|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................ |
Original
Contribution / Clinical Investigation
|





|
<-- Jordan, USA -->
Herpetic
Eye Disease and Glaucoma Related Diagnosis
[pdf version]
C. Dan Earley, Amal M Althawabi,
Paul R Cotran, Sarkis H Soukiasian
<-- Turkey, Lebanon, Australia -->
Cholelithiasis
may also be a consequence of metabolic syndrome
[pdf
version]
Mehmet Rami Helvaci, Mursel Davarci,
Orhan Veli Ozkan, Ersan Semerci, Abdulrazak
Abyad, Lesley Pocock
<-- Iran -->
SUMO1 pseudogene
3 (SUMO1P3) expression in human gastric cancer
and its clinical significance
[pdf version]
Hamid Reza Baradaran-Ghahfarokhi, Habib Malekpour,
Ehsan Nazemalhosseini Mojarad,
Hamid Asadzadeh Aghdaei, Majid Asadi-Samani,
Azar Baradaran
<-- Iran -->
Decoy Cell
Viruria in Kidney Transplant Patients. Does
it correlate with Renal Function?
[pdf version]
Akram Abedi, Mojgan Mortazavi,
Omid Mirmosayyeb, Shahram Taheri,
Nooshin Afsharmoghadam,
Majid Asadi-Samani, Shahram Sajadieh,
Azar Baradaran
<-- Iran, Austria -->
To determine
how frequently pregnant asthmatics are sensitive
to food and inhalation allergens
[pdf version]
Nasrin Fazel, Michael Kundi,
Erika Jensen-Jarolim,
Isabella Maria Pali-Schöll,
Asghar Kazemzadeh, Mojtaba Fattahi Abdizadeh,
Habibollah Esmaily,
Roya Akbarzadeh, Raheleh Ahmadi
|
........................................................
Special Education Feature
........................................................
International Health
Affairs
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| July 2017 - Volume
15, Issue 5 |
|
|
Herpetic Eye Disease
and Glaucoma Related Diagnosis
C.
Dan Earley
(1)
Amal M Althawabi (1,3)
Paul R Cotran (1,2)
Sarkis H Soukiasian (1,2)
(1) Dept. of Ophthalmology, Lahey Clinic, Burlington,
MA
(2) Dept. of Ophthalmology, Tufts Medical Center,
Boston, MA
(3) Royal Medical Services, King Hussein Medical
Center, Amman, Jordan.
Correspondence:
Dr. Amal Al-Thawabi
Cornea and refractive surgery specialist in
King Hussein Medical Center
Amman,
Jordan
Email: aalthawabi@hotmail.com
|
Abstract
This is a
medical record review that was performed
at Lahey Hospital Medical Center. Medical
records in the period between 12/2003
and 12/2013 were reviewed; 1098 medical
records were reviewed, those who were
carrying diagnosis of Herpetic Eye Disease
(HED) were divided into 2 groups according
to the etiological agent: Herpes Simplex
virus (HSV) (n=473) , Varicella Zoster
Virus (VZV) (n=625).
The groups were evaluated for the age
at diagnosis and the etiologies of elevated
Intra occular Pressure (IOP), whether
it was HED related (trabeculitis, steroid
response), or non HED Glaucoma Related
Diagnosis.
Although many of the features between
HSV and VZV subgroups are similar, the
VZV group was older and appeared to have
more prolonged hypertensive course than
the HSV group.
4.3% of patients with HED have significant
elevated IOP directly related to disease
or treatment.
Secondary glaucoma is a consequence of
Herpetic Eye disease, but fortunately
surgical intervention is rarely required
to control IOP.
Key words:
Herpetic Eye Disease, Glaucoma related
diagnosis, Ocular Hypertension,
steroid responder.
|
Present the overall incidence of glaucoma related
diagnosis (GRD) in a population of patients with
herpetic eye disease.
Describe the incidence of glaucoma (Gl) or ocular
hypertension (OHT) directly attributed to HED
or treatment [e.g. steroid response (SR)].
Identify differentiating characteristics of GL,
OHT or SR within the HED population (VZV vs HSV).
Herpetic eye disease is the most common cause
of infectious anterior uveitis seen at tertiary
referral centers.(1)
Elevated intraocular pressure may be seen as
a presenting or complicating feature of herpetic
eye diseases (HED) due to both Varicella Zoster
Virus (VZV) and Herpes Simplex Virus (HSV).
Potential mechanisms include decreased outflow
due to inflammation of the trabecular meshwork
(trabeculitis), outflow blockage due to inflammatory
and pigmentary debris, as well as a hypertensive
response to topical corticosteroids.
Most patients with acute iritis have low IOP.
High IOP in a patient with uveitis should raise
a high index of suspicion of a herpetic etiology,
especially with the presence of other signs
such as large greasy KP's, iris transillumination
defects and segmental iris atrophy(1).
There are other possible causes for elevated
IOP associated with HSV and VZV keratouveitis,
Although secondary angle closure may occur due
to pupillary block by posterior synechiae, most
patients who developed glaucoma had open angles.(2)
This is likely attributed to increase in aqueous
debris from elevated aqueous proteins, fibrin,
and inflammatory cells.(3,4) Consecutive damage
to the trabecular meshwork by HSV and VZV infection
has also been noticed (12).
Steroid response glaucoma could be another mechanism
of IOP elevation associated with herpetic keratouveitis,
Treatment with topical steroids will reduce
the risk of persistent or progressive stromal
keratouveitis, but should be adjusted according
to the IOP values after starting steroid treatment.(6,7,8)
The purpose of our study is to present the overall
incidence of glaucoma related diagnosis (GRD)
in a population of patients with herpetic eye
disease; describe the incidence of glaucoma
(Gl) or ocular hypertension (OHT) directly attributed
to HED or treatment [e.g. steroid response (SR)]
and to identify differentiating characteristics
of GL, OHT or SR within the HED population (VZV
vs HSV).
This
is
a
retrospective
medical
records
review
that
was
conducted
in
patients
evaluated
at
the
Lahey
Hospital
and
Medical
Center
Department
of
Ophthalmology
between
12/2003
and
12/2013.
All
the
records
were
screened
for
ICD-9
codes
of
Herpetic
Eye
Disease
(053.2…
and
054.4…).
All
medical
records
of
patients
with
both
HED
and
concurrent
GRD
codes
were
reviewed
to
identify
GRD
directly
attributable
to
HED
or
treatment.
Elevated
IOP
was
considered
significant
if
>25
on
two
consecutive
measurements.
This
study
specifically
separated
causes
of
IOP
in
Herpetic
Eye
Disease.
Although
many
of
the
features
between
HSV
and
VZV
subgroups
are
similar,
the
VZV
group
was
older
and
appeared
to
have
a
more
prolonged
hypertensive
course
than
the
HSV
group.
Surgical
intervention
was
rare,
consistent
with
literature.
1,098
patients
were
included
in
our
medical
review;
57%
carried
the
diagnosis
of
VZV
and
43%
had
HSV.
32%
had
Glaucoma
related
diagnosis
(GRD)
and
Herpetic
Eye
Disease
(HED).
The
average
age
of
presentation
was
67
years
for
VZV
diagnosis
and
58
years
for
HSV
diagnosis.
In
the
majority
of
patients,
the
GRD
was
not
directly
related
to
HED
(87%
had
unrelated
glaucoma
related
diagnosis).
Approximately
4%
of
all
patients
with
HED
had
elevated
IOP
directly
related
to
HED
or
treatment.
(Table
1).
Table
1:
shows
patient
distribution
of
the
total
number
of
medical
records
reviewed,
the
number
of
cases
with
glaucoma
related
and
unrelated
to
HED
diagnosis,
average
age
of
presentation
and
average
age
to
IOP
elevation
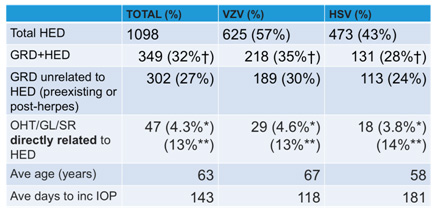
HED=Herpetic
Eye
Disease
GRD-Glaucoma
Related
Diagnosis
OHT/GL/SR-
Ocular
Hypertension/
Glaucoma/
Steroid
Responder
†
%
out
of
Total
HED
(HSV
+VZV)
*
%
out
of
Total
HED
population
**
%
out
of
GRD
+
HED
In
only
13%
of
patients
identified
with
both
HED
and
GRD
was
the
elevated
IOP
directly
related
to
HED
or
treatment.
HZV
patients
appeared
older
than
HSV
patients
and
approached
statistical
significance.
Chronic
elevated
IOP
(requiring
treatment
>
3
months)
due
to
inflammation
was
more
often
noted
with
VZV
(Figure
1).
Figure
1:
Rates
of
Inflammatory
OHT
(Ocular
Hypertension)
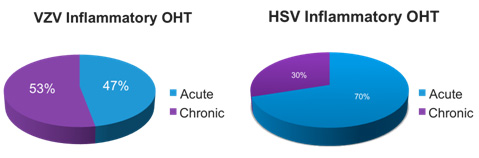
Peak
IOPs
and
number
of
glaucoma
medications
used
were
similar
between
HSV
and
VZV
groups
(Data
not
presented).
We
were
able
to
classify
the
etiologies
of
increased
IOP
among
this
group
(Table
2).
We
found
that
2.5%
had
an
inflammatory
etiology,
1.4%
was
due
to
steroid
response
and
0.5%
was
combined
effect
of
inflammatory
and
steroid
response.
Table
2:
Etiology
of
Increased
IOP
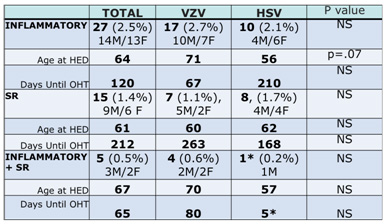
*
1
Patient
HED=Herpetic
Eye
Disease
GRD-Glaucoma
Related
Diagnosis
OHT/GL/SR-
Ocular
Hypertension/
Glaucoma/
Steroid
Responder
†
%
out
of
Total
HED
(HSV
+VZV)
*
%
out
of
Total
HED
population
**
%
out
of
GRD
+
HED
Surgical
intervention
was
rare,
consistent
with
the
literature.(8)
Table
3:
Patients
requiring
surgical
intervention
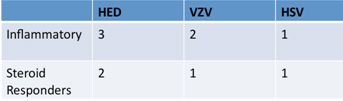
This
study
specifically
separated
causes
of
IOP
in
HED
(Inflammation
vs
Steroid
Response
vs
Mixed
diagnosis).
4.3%
of
patients
with
HED
have
significant
elevated
IOP
directly
related
to
disease
or
treatment.
Although
many
of
the
features
between
HSV
and
VZV
subgroups
are
similar,
the
VZV
group
was
older
and
appeared
to
have
more
prolonged
hypertensive
course
than
the
HSV
group.
Surgical
intervention
was
rare,
consistent
with
literature.
Study
limited
by
retrospective
study
design.
Some
differences
between
HSV
and
VZV
sub
groups
approached
statistical
significance
but
small
study
population
limited
critical
statistical
evaluation.
Future
study
of
larger
population
of
patients
may
help
better
define
potential
differences
between
HSV
and
VZV.
Although
by
ICD
9
searching
32%
of
patients
with
HED
had
associated
GRD,
the
vast
majority
were
unrelated
to
herpes.
1.
Doran,
M.
Understanding
and
Treating
Viral
Anterior
Uveitis.
EyeNet
magazine.
2009
(1);
33-37.
2.
Falcon
MG,
Williams
HP.
Herpes
simplex
keratouveitis
and
glaucoma.
Trans
Ophthal
Soc
UK.
1978;98:101-104.
3.
Peretz
WL,
Tomasi
TB.
Aqueous
humor
proteins
in
uveitis.
Immunoelectrophoretic
and
gel
diffusion
studies
on
normal
and
pathological
human
aqueous
humor.
Arch
Ophthalmol.
1961;65:20-23.
4.
Hogan
MJ,
Kimura
SJ,
Thygeson
P.
Pathology
of
herpes
simplex
keratouveitis.
Trans
Am
Ophthalmol
Soc.
1963;61:75-99.
5.
Tiwari
V,
Clement
C,
Scanlan
P,
et
al.
A
role
for
herpes
virus
entry
mediator
as
the
receptor
for
herpes
simplex
virus
1
entry
into
primary
human
trabecular
meshwork
cells.
J
Virol.
2005;79(20):13173-13179.
6.
Gorla,
M.,
&
Brown,
S.
(2013).
Glaucoma
Associated
With
Herpes
Simplex
Virus.
Glaucoma
Today,
46-48.
7.
Wilhelmus
KR,
Gee
L,
Hauck
WW,
et
al.
Herpetic
Eye
Disease
Study.
A
controlled
trial
of
topical
corticosteroids
for
herpes
simplex
stromal
keratitis.
Ophthalmology.
1994;101:1883-1896.
8.
Sungur,
G.,
Hazirolan,
D.,
Yalvac,
I.,
Ozer,
P.,
Aslan,
B.,
&
Duman,
S.
(n.d.).
Incidence
and
prognosis
of
ocular
hypertension
secondary
to
viral
uveitis.
International
Ophthalmology,191-194
9.
Wensing,
B.,
Relvas,
L.,
&
Caspers,
L.
(2011).
Comparison
of
rubella
virus-
and
herpes
virus-associated
anterior
uveitis:
Clinical
manifestations
and
visual
prognosis.
Ophthalmology,
118(10),
1905-1910.
|
|
.................................................................................................................

|
| |
|

