|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................ |
Original
Contribution / Clinical Investigation
|





|
<-- Jordan, USA -->
Herpetic
Eye Disease and Glaucoma Related Diagnosis
[pdf version]
C. Dan Earley, Amal M Althawabi,
Paul R Cotran, Sarkis H Soukiasian
<-- Turkey, Lebanon, Australia -->
Cholelithiasis
may also be a consequence of metabolic syndrome
[pdf
version]
Mehmet Rami Helvaci, Mursel Davarci,
Orhan Veli Ozkan, Ersan Semerci, Abdulrazak
Abyad, Lesley Pocock
<-- Iran -->
SUMO1 pseudogene
3 (SUMO1P3) expression in human gastric cancer
and its clinical significance
[pdf version]
Hamid Reza Baradaran-Ghahfarokhi, Habib Malekpour,
Ehsan Nazemalhosseini Mojarad,
Hamid Asadzadeh Aghdaei, Majid Asadi-Samani,
Azar Baradaran
<-- Iran -->
Decoy Cell
Viruria in Kidney Transplant Patients. Does
it correlate with Renal Function?
[pdf version]
Akram Abedi, Mojgan Mortazavi,
Omid Mirmosayyeb, Shahram Taheri,
Nooshin Afsharmoghadam,
Majid Asadi-Samani, Shahram Sajadieh,
Azar Baradaran
<-- Iran, Austria -->
To determine
how frequently pregnant asthmatics are sensitive
to food and inhalation allergens
[pdf version]
Nasrin Fazel, Michael Kundi,
Erika Jensen-Jarolim,
Isabella Maria Pali-Schöll,
Asghar Kazemzadeh, Mojtaba Fattahi Abdizadeh,
Habibollah Esmaily,
Roya Akbarzadeh, Raheleh Ahmadi
|
........................................................
Special Education Feature
........................................................
International Health
Affairs
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| July 2017 - Volume
15, Issue 5 |
|
|
Cholelithiasis may also
be a consequence of metabolic syndrome
Mehmet Rami
Helvaci (1)
Mursel Davarci (2)
Orhan Veli Ozkan (3)
Ersan Semerci (3)
Abdulrazak Abyad (4)
Lesley Pocock (5)
(1) Specialist of Internal
Medicine, M.D.
(2) Specialist of Urology, M.D.
(3) Specialist of General Surgery, M.D.
(4) Middle-East Academy for Medicine of Aging,
Chairman, M.D., MPH, MBA, AGSF
(5) medi-WORLD International
Correspondence:
Mehmet Rami Helvaci, M.D.
07400, ALANYA,
Antalya,
Turkey
Phone: 00-90-506-4708759
Email: mramihelvaci@hotmail.com
|
Abstract
Background:
We tried to understand whether or not
there is a significant relationship between
cholelithiasis and parameters of the metabolic
syndrome.
Methods: The study was performed
in Internal Medicine Polyclinics on routine
check up patients. All cases with cholelithiasis
or already performed cholecystectomy for
cholelithiasis were put into the first
group and age and sex-matched control
cases were put into the second group.
Results: One hundred and fourty-four
cases either with cholelithiasis or already
performed cholecystectomy for cholelithiasis
were detected among 3.437 cases, totally
(4.1%). One hundred and sixteen (80.1%)
of them were female with a mean age of
53.6 years. Obesity was significantly
higher (54.8% versus 43.7%, p<0.01)
and normal weight was significantly lower
(7.6% versus 18.0%, p<0.01) in the
cholelithiasis group, and the mean body
mass indexes (BMI) were 31.0 versus 28.9
kg/m2 in them, respectively (p<0.01).
Probably parallel to the higher mean BMI,
prevalences of hypertension (26.3% versus
13.1%, p<0.001) and hypertriglyceridemia
(25.0% versus 18.0%, p<0.05) were also
higher in the cholelithiasis group, significantly.
On the other hand, hyperbetalipoproteinemia
was significantly lower in the cholelithiasis
group with unknown reasons (9.7% versus
18.0%, p<0.05).
Conclusions: Cholelithiasis is
a common pathology in society and nearly
four-fold more frequent in women, particularly
in their fifties. There are significant
relationships between cholelithiasis and
parameters of the metabolic syndrome including
female predominance, elder age, BMI, obesity,
hypertension, and hypertriglyceridemia.
On the other hand, the significantly lower
prevalence of hyperbetalipoproteinemia
in the cholelithiasis patients should
be researched with further studies.
Key words: Cholelithiasis, metabolic
syndrome, obesity, hyperbetalipoproteinemia
|
Chronic endothelial damage may be the most common
type of vasculitis and the leading cause of aging,
morbidity, and mortality in human beings. Much
higher blood pressure (BP) of the afferent vasculature
may be the major underlying cause by inducing
recurrent injuries on endothelium, and probably
whole afferent vasculature including capillaries,
are involved in the process. Thus the term of
venosclerosis is not as famous as atherosclerosis
in the literature. Secondary to the chronic endothelial
inflammation, edema, and fibrosis, vascular walls
become thickened, their lumens are narrowed, and
they lose their elastic natures that reduce blood
flow and increase systolic BP further. Some of
the well-known indicators of the inflammatory
process are sedentary life style, animal-rich
diet, overweight, smoking, alcohol, hypertriglyceridemia,
hyperbetalipoproteinemia, dyslipidemia, impaired
fasting glucose, impaired glucose tolerance, white
coat hypertension, and other chronic inflammatory
processes including rheumatologic disorders, prolonged
infections, and cancers for the development of
irreversible consequences including obesity, hypertension,
diabetes mellitus (DM), cirrhosis, peripheric
artery disease (PAD), chronic obstructive pulmonary
disease (COPD), chronic renal disease (CRD), coronary
artery disease (CAD), mesenteric ischemia, osteoporosis,
and stroke, all of which terminate with early
aging and death. Although early withdrawal of
causative factors may prevent final consequences,
after development of cirrhosis, COPD, CRD, CAD,
PAD, or stroke, endothelial changes cannot be
reversed completely due to their fibrotic natures.
They were researched under the title of metabolic
syndrome in the literature, extensively (1-4).
On the other hand, gallstone is also found among
one of the most common health problems in developed
countries (5), and it is particularly frequent
in women above the age of 40 years (6). Most of
the gallstones are found in the gallbladder, which
is also called cholelithiasis. Its pathogenesis
is uncertain and it appears to be influenced by
genetic and environmental factors (7). Excess
weight is a known and age-independent risk factor
for gallstone (8). Delayed bladder emptying, decreased
small intestinal motility, and sensitivity to
cholecystokinin were associated with obesity and
gallstone disease (9). An increased risk was confirmed
in obese diabetics with hypertriglyceridemia (10),
and plasma cholesterol levels were found related
with gallstone (11). Even more conflicting results
were reported about an association between gallstone
and smoking (12-14). We tried to understand whether
or not there is a significant relationship between
cholelithiasis and parameters of the metabolic
syndrome.
The study was performed in Internal Medicine
Polyclinics of the Dumlupinar and Mustafa Kemal
Universities on routine check up of patients
between August 2005 and November 2007. We took
consecutive patients below the age of 70 years
to avoid debility induced weight loss in elders.
Their medical histories, including smoking habit,
hypertension, DM, dyslipidemia, and already
used medications and performed operations were
learnt, and a routine check up procedure including
fasting plasma glucose (FPG), triglyceride,
high density lipoprotein cholesterol (HDL-C),
low density lipoprotein cholesterol (LDL-C),
and an abdominal ultrasonography was performed.
Patients with devastating illnesses including
type 1 DM, malignancies, acute or chronic renal
failure, chronic liver diseases, hyper- or hypothyroidism,
and heart failure were excluded to avoid their
possible effects on weight. Current daily smokers
for the last six months and cases with a history
of five pack-years were accepted as smokers.
Cigar or pipe smokers were excluded. Body mass
index (BMI) of each case was calculated by the
measurements of the same physician instead of
verbal expressions since there is evidence that
heavier individuals systematically underreport
their weight (15). Weight in kilograms is divided
by height in meters squared, and underweight
is defined as a BMI of lower than 18.5, normal
weight as 18.5-24.9, overweight as 25.0-29.9,
and obesity as a BMI of 30.0 kg/m2 or greater
(16). Cases with an overnight FPG level of 126
mg/dL or greater on two occasions or already
receiving antidiabetic medications were defined
as diabetics (16). An oral glucose tolerance
test with 75-gram glucose was performed in cases
with a FPG level between 110 and 125 mg/dL,
and diagnosis of cases with a 2-hour plasma
glucose level 200 mg/dL or greater is DM (16).
Patients with dyslipidemia were detected, and
we used the National Cholesterol Education Program
Expert Panel's recommendations for defining
dyslipidemic subgroups (16). Dyslipidemia is
diagnosed when LDL-C is 160 or higher and/or
TG is 200 or higher and/or HDL-C is lower than
40 mg/dL. Office BP was checked after a 5-minute
rest in seated position, with a mercury sphygmomanometer
on three visits, and no smoking was permitted
during the previous 2 hours. A 10-day twice
daily measurement of blood pressure at home
(HBP) was obtained in all cases, even in normotensives
in the office due to the risk of masked hypertension
after a 10-minute education session about proper
BP measurement techniques (17). The education
included recommendation of upper arm while discouraging
wrist and finger devices, using a standard adult
cuff with bladder sizes of 12 x 26 cm for arm
circumferences up to 33 cm in length and a large
adult cuff with bladder sizes of 12 x 40 cm
for arm circumferences up to 50 cm in length,
and taking a rest at least for a period of 5
minutes in the seated position before measurement.
An additional 24-hour ambulatory BP monitoring
was not required due to the equal efficacy of
the method with HBP measurement to diagnose
hypertension (18). Eventually, hypertension
is defined as a BP of 135/85 mmHg or greater
on HBP measurements (17). Cholelithiasis was
diagnosed ultrasonographically. Eventually,
all cases either with presenting cholelithiasis
or already performed cholecystectomy for cholelithiasis
were put into the first group and age and sex-matched
control cases were put into the second groups.
Prevalences of smoking, normal weight, overweight,
obesity, hypertension, DM, hypertriglyceridemia,
hyperbetalipoproteinemia, and dyslipidemia and
mean BMI values were detected in both groups
and compared in between. Mann-Whitney U test,
Independent-Samples t test, and comparison of
proportions were used as the methods of statistical
analyses.
Although
the
exclusion
criteria,
119
cases
with
cholecystectomy
for
cholelithiasis
and
25
with
already
presenting
asymptomatic
cholelithiasis
were
detected
among
3.437
cases,
total
(4.1%).
One
hundred
and
sixteen
(80.1%)
of
them
were
female
with
a
mean
age
of
53.6
years,
so
cholelithiasis
is
mainly
a
disorder
of
females
in
their
fifties.
Prevalences
of
smoking
were
similar
in
the
cholelithiasis
and
control
groups
(18.0%
versus
19.4%,
p>0.05,
respectively).
There
was
not
any
patient
with
underweight.
Interestingly,
92.3%
(133
cases)
of
the
cholelithiasis
group
had
excess
weight
and
only
7.6%
(11
cases)
of
them
had
normal
weight.
Obesity
was
significantly
higher
(54.8%
versus
43.7%,
p<0.01)
and
normal
weight
was
significantly
lower
(7.6%
versus
18.0%,
p<0.01)
in
the
cholelithiasis
group.
Mean
BMI
values
were
31.0
and
28.9
kg/m2,
(p<0.01)
in
them.
Probably
parallel
to
the
higher
mean
BMI,
prevalences
of
hypertension
(26.3%
versus
13.1%,
p<0.001)
and
hypertriglyceridemia
(25.0%
versus
18.0%,
p<0.05)
were
also
higher
in
the
cholelithiasis
group,
significantly.
Differences
were
nonsignificant
according
to
the
prevalences
of
DM
and
dyslipidemia.
On
the
other
hand,
hyperbetalipoproteinemia
was
significantly
lower
in
the
cholelithiasis
group
with
unknown
reasons
(9.7%
versus
18.0%,
p<0.05)
(Table
1).
Table
1:
Comparison
of
cases
with
and
without
cholelithiasis
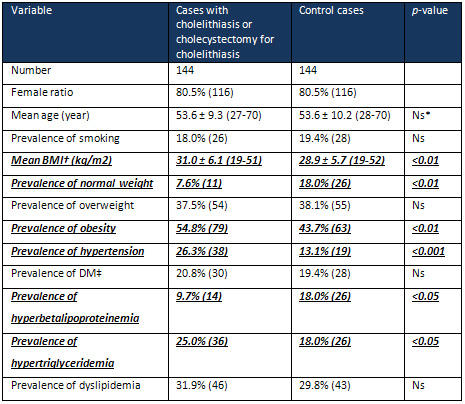
*Nonsignificant
(p>0.05)
†Body
mass
index
‡Diabetes
mellitus
Excess
weight
leads
to
both
structural
and
functional
abnormalities
of
many
organ
systems
of
the
body.
Recent
studies
revealed
that
adipose
tissue
produces
biologically
active
leptin,
tumor
necrosis
factor-alpha,
plasminogen
activator
inhibitor-1,
and
adiponectin
which
are
closely
related
with
the
development
of
complications
(19).
For
instance,
the
cardiovascular
field
has
recently
shown
a
great
interest
in
the
role
of
inflammation
in
development
of
atherosclerosis
and
numerous
studies
indicated
that
inflammation
plays
a
significant
role
in
the
pathogenesis
of
atherosclerosis
and
thrombosis
(20,
21).
Adipose
tissue
is
involved
in
the
regulation
of
cytokines
(22).
On
the
other
hand,
individuals
with
excess
weight
will
have
an
increased
circulating
blood
volume
as
well
as
an
increased
cardiac
output,
thought
to
be
the
result
of
increased
oxygen
demand
of
the
excessive
fat
tissue.
The
prolonged
increase
in
circulating
blood
volume
can
lead
to
myocardial
hypertrophy
and
decreased
compliance,
in
addition
to
the
common
comorbidity
of
hypertension.
In
addition
to
the
hypertension,
the
prevalences
of
high
FPG,
high
serum
total
cholesterol,
and
low
HDL-C,
and
their
clustering
were
all
raised
with
the
higher
BMI
(23).
Combination
of
these
cardiovascular
risk
factors
will
eventually
lead
to
an
increase
in
left
ventricular
stroke
with
higher
risks
of
arrhythmias,
cardiac
failure,
and
sudden
cardiac
death.
Similarly,
the
incidences
of
CHD
and
stroke
have
increased
with
a
higher
BMI
in
the
other
studies
(23,
24),
and
risk
of
death
from
all
causes
including
cancers
increases
throughout
the
range
of
moderate
and
severe
excess
weight
for
both
genders
in
all
age
groups
(25).
As
another
consequence
of
excess
weight
on
health,
the
cholelithiasis
cases
had
a
significantly
higher
mean
BMI
in
the
present
study
(31.0
versus
28.9
kg/m2,
p<0.01)
similar
to
the
previous
reports
(8,
9).
Probably
as
a
consequence
of
the
significantly
higher
BMI,
the
prevalences
of
hypertension
(26.3%
versus
13.1%,
p<0.001)
and
hypertriglyceridemia
(25.0%
versus
18.0%,
p<0.05)
were
also
higher
in
the
cholelithiasis
patients.
The
relationship
between
excess
weight
and
elevated
BP
and
hypertriglyceridemia
is
already
described
in
the
metabolic
syndrome
(26),
and
clinical
manifestations
of
the
syndrome
include
obesity,
dyslipidemia,
hypertension,
insulin
resistance,
and
proinflammatory
as
well
as
prothrombotic
states
(27).
The
above
confirmed
increased
risk
of
cholelithiasis
in
obese
diabetics
with
hypertriglyceridemia
may
also
be
an
indicator
of
its
association
with
the
metabolic
syndrome
(10,
26).
Although
the
presence
of
some
conflicting
results
in
the
literature
(12-14),
we
did
not
find
any
significant
association
between
cholelithiasis
and
smoking
in
the
present
study
(p>0.05).
On
the
other
hand,
the
lower
prevalence
of
hyperbetalipoproteinemia
in
the
cholelithiasis
patients
in
the
present
study
(9.7%
versus
18.0%,
p<0.05),
although
the
significantly
higher
mean
BMI
values
of
them,
should
be
researched
with
further
studies.
As
a
conclusion,
cholelithiasis
is
a
common
pathology
in
society
and
nearly
four-fold
more
frequent
in
women,
particularly
in
their
fifties.
There
are
significant
relationships
between
cholelithiasis
and
parameters
of
the
metabolic
syndrome
including
female
predominance,
elder
age,
BMI,
obesity,
hypertension,
and
hypertriglyceridemia.
On
the
other
hand,
the
significantly
lower
prevalence
of
hyperbetalipoproteinemia
in
the
cholelithiasis
patients
should
be
researched
with
further
studies.
1.
Eckel
RH,
Grundy
SM,
Zimmet
PZ.
The
metabolic
syndrome.
Lancet
2005;
365:
1415-1428.
2.
Helvaci
MR,
Kaya
H,
Sevinc
A,
Camci
C.
Body
weight
and
white
coat
hypertension.
Pak
J
Med
Sci
2009;
25:
6:
916-921.
3.
Helvaci
MR,
Aydin
LY,
Aydin
Y.
Digital
clubbing
may
be
an
indicator
of
systemic
atherosclerosis
even
at
microvascular
level.
HealthMED
2012;
6:
3977-3981.
4.
Helvaci
MR,
Aydin
Y,
Gundogdu
M.
Atherosclerotic
effects
of
smoking
and
excess
weight.
J
Obes
Wt
Loss
Ther
2012;
2:
7.
5.
Tazuma
S.
Gallstone
disease:
Epidemiology,
pathogenesis,
and
classification
of
biliary
stones
(common
bile
duct
and
intrahepatic).
Best
Pract
Res
Clin
Gastroenterol
2006;
20:
1075-1083.
6.
Katsika
D,
Grjibovski
A,
Einarsson
C,
Lammert
F,
Lichtenstein
P,
Marschall
HU.
Genetic
and
environmental
influences
on
symptomatic
gallstone
disease:
a
Swedish
study
of
43,141
twin
pairs.
Hepatology
2005;
41:
1138-1143.
7.
Lammert
F,
Sauerbruch
T.
Mechanisms
of
disease:
the
genetic
epidemiology
of
gallbladder
stones.
Nat
Clin
Pract
Gastroenterol
Hepatol
2005;
2:
423-433.
8.
Erlinger
S.
Gallstones
in
obesity
and
weight
loss.
Eur
J
Gastroenterol
Hepatol
2000;
12:
1347-1352.
9.
Mathus-Vliegen
EM,
Van
Ierland-Van
Leeuwen
ML,
Terpstra
A.
Determinants
of
gallbladder
kinetics
in
obesity.
Dig
Dis
Sci
2004;
49:
9-16.
10.
Fraquelli
M,
Pagliarulo
M,
Colucci
A,
Paggi
S,
Conte
D.
Gallbladder
motility
in
obesity,
diabetes
mellitus
and
coeliac
disease.
Dig
Liver
Dis
2003;
35:
12-16.
11.
Devesa
F,
Ferrando
J,
Caldentey
M,
Borghol
A,
Moreno
MJ,
Nolasco
A,
et
al.
Cholelithiasic
disease
and
associated
factors
in
a
Spanish
population.
Dig
Dis
Sci
2001;
46:
1424-1436.
12.
Kono
S,
Eguchi
H,
Honjo
S,
Todoroki
I,
Oda
T,
Shinchi
K,
et
al.
Cigarette
smoking,
alcohol
use,
and
gallstone
risk
in
Japanese
men.
Digestion
2002;
65:
177-183.
13.
Okamoto
M,
Yamagata
Z,
Takeda
Y,
Yoda
Y,
Kobayashi
K,
Fujino
MA.
The
relationship
between
gallbladder
disease
and
smoking
and
drinking
habits
in
middle-aged
Japanese.
J
Gastroenterol
2002;
37:
455-462.
14.
Jorgensen
T.
Gall
stones
in
a
Danish
population.
Relation
to
weight,
physical
activity,
smoking,
coffee
consumption,
and
diabetes
mellitus.
Gut
1989;
30:
528-534.
15.
Bowman
RL,
DeLucia
JL.
Accuracy
of
selfreported
weight:
a
meta-analysis.
Behav
Ther
1992;
23:
637-635.
16.
Third
Report
of
the
National
Cholesterol
Education
Program
(NCEP)
Expert
Panel
on
Detection,
Evaluation,
and
Treatment
of
High
Blood
Cholesterol
in
Adults
(Adult
Treatment
Panel
III)
final
report.
Circulation
2002;
106:
3143-3421.
17.
O'Brien
E,
Asmar
R,
Beilin
L,
Imai
Y,
Mallion
JM,
Mancia
G,
et
al.
European
Society
of
Hypertension
recommendations
for
conventional,
ambulatory
and
home
blood
pressure
measurement.
J
Hypertens
2003;
21:
821-848.
18.
Helvaci
MR,
Seyhanli
M.
What
a
high
prevalence
of
white
coat
hypertension
in
society!
Intern
Med
2006;
45:
671-674.
19.
Funahashi
T,
Nakamura
T,
Shimomura
I,
Maeda
K,
Kuriyama
H,
Takahashi
M,
et
al.
Role
of
adipocytokines
on
the
pathogenesis
of
atherosclerosis
in
visceral
obesity.
Intern
Med
1999;
38:
202-206.
20.
Widlansky
ME,
Gokce
N,
Keaney
JF
Jr,
Vita
JA.
The
clinical
implications
of
endothelial
dysfunction.
J
Am
Coll
Cardiol
2003;
42:
1149-1160.
21.
Ridker
PM.
High-sensitivity
C-reactive
protein:
Potential
adjunct
for
global
risk
assessment
in
the
primary
prevention
of
cardiovascular
disease.
Circulation
2001;
103:
1813-1818.
22.
Yudkin
JS,
Stehouwer
CD,
Emeis
JJ,
Coppack
SW.
C-reactive
protein
in
healthy
subjects:
associations
with
obesity,
insulin
resistance,
and
endothelial
dysfunction:
a
potential
role
for
cytokines
originating
from
adipose
tissue?
Arterioscler
Thromb
Vasc
Biol
1999;
19:
972-978.
23.
Zhou
B,
Wu
Y,
Yang
J,
Li
Y,
Zhang
H,
Zhao
L.
Overweight
is
an
independent
risk
factor
for
cardiovascular
disease
in
Chinese
populations.
Obes
Rev
2002;
3:
147-156.
24.
Zhou
BF.
Effect
of
body
mass
index
on
all-cause
mortality
and
incidence
of
cardiovascular
diseases--report
for
meta-analysis
of
prospective
studies
open
optimal
cut-off
points
of
body
mass
index
in
Chinese
adults.
Biomed
Environ
Sci
2002;
15:
245-252.
25.
Calle
EE,
Thun
MJ,
Petrelli
JM,
Rodriguez
C,
Heath
CW
Jr.
Body-mass
index
and
mortality
in
a
prospective
cohort
of
U.S.
adults.
N
Engl
J
Med
1999;
341:
1097-1105.
26.
Helvaci
MR,
Kaya
H,
Gundogdu
M.
Association
of
increased
triglyceride
levels
in
metabolic
syndrome
with
coronary
artery
disease.
Pak
J
Med
Sci
2010;
26:
667-672.
27.
Tonkin
AM.
The
metabolic
syndrome(s)?
Curr
Atheroscler
Rep
2004;
6:
165-166.
|
|
.................................................................................................................

|
| |
|

