|
Narrowband UVB Therapy
in Yemeni Patients
Amer Omer
Bin Zou (1)
Asia Hussain Al-Asbahi (1)
Maysa Saeed Al-Noban (2)
(1) Assistant Professor, Department of Dermatology,
Faculty of Medicine, University of Aden
(2) Lecturer, Department of Community medicine
and Public Health, Faculty of Medicine,
University of Aden
Correspondence:
Dr. Amer Omer Bin Al-Zou
Assistant professor, dermatology,
Faculty of medicine, University of Aden, Yemen.
Mobile: +967 736 361 344
Email: amer_zou2009@yahoo.com
|
Abstract
Objective: This
study aimed to assess the usefulness of
narrow band UVB (NB-UVB) therapy in Yemeni
patients with different skin conditions.
Methods: A
prospective clinical audit was conducted
of 120 Yemeni patients (45 males and 75
females), aged 5-54 years from all patients
with different skin diseases in dermatology
clinic (January 2013 - May 2014), treated
by NB-UVB irradiation without being combined
with topical steroid or topical chemotherapy
during the course of the study.
Results:
120 patients enrolled in this study with
mean age 25.8±12.6 years old. Females
consisted of the major rate (62.5%), and
patients who came from Aden had a high
rate (77.5%).
Ninety four (78.3%) patients had complete
response to treatment, 6.7% had partial
and 15% had no response. Mycosis fungoid
and atopic dermatitis had a high mean
number of session (84.50±0.70),
followed by vitiligo with mean number
of sessions 27.10±23.70. The Lichen
planus, Mycosis and Pityriasis had complete
response (100%) to treatment, followed
by vitiligo 79.3%, while partial response
appeared in patients with alopecia (66.7%)
and atopic dermatitis (22.2%). Patients
with chronic renal failure had no response
to treatment in 33.3%, followed by Parapsoriasis
(20%).
Conclusion: Our
study proves that NB-UVB therapy is an
effective and safe tool in the management
of skin diseases and is considered the
first-line phototherapeutic option for
many skin conditions.
Key words:
Narrowband UVB, Phototherapy, Skin Diseases,
Response.
|
For years, phototherapy has been used in a
wide range of skin diseases, which is unsurprising
as skin is the anatomical feature most directly
exposed to light. Phototherapy became a common
practice in dermatology at the beginning of
the 20thcentury, when Goeckerman introduced
a combination of coal tar and UVB. Later, Ingram
developed a similar treatment protocol, which
consisted of a 15-30-minute bath in a tar solution
followed by a UVB dose. It started with 30-50%
of the minimum erythema dose and this light
dose was increased by 30-50% at each session.
Subsequently, an anthralin paste with low concentrations
(0.05-0.1%) was applied to and maintained on
the treated intertegument for 6-24 hours (1).
Nowadays phototherapy is a popular treatment
option, which includes both of the generalized
ultraviolet B (UVB) therapies, broadband UVB
(BB-UVB) and narrowband UVB (NB-UVB). UVB delivers
a high amount of energy to the stratum corneum
and superficial layers of the epidermis and
is primarily responsible for sunburn, suntan,
and skin cancers. It produces tanning more efficiently
than UVA (2).
Narrow band UVB (NB-UVB) with the wavelength
range from 311 to 313 nm phototherapy offers
potential for the future and is an established
method for managing patients with psoriasis,
as well as difficult eczema, atopic dermatitis
(3) mycosis fungoides (4) and other skin disorders.
It works by reducing inflammation in the skin
using very narrowly defined wavelengths of UV
light to reduce the problems and risks of broadband
ultraviolet light typically seen with sun beds.
It is effective with a fraction of the dose
normally delivered by these commercial machines,
reducing skin cancer risk and side effects.
The results of present studies provides evidence
that narrow band UVB is superior to broad band
UVB as regards to the efficacy of the treatment
of generalized lichen Planus patients. Narrow
-band phototherapy has a higher ratio of therapeutic
to erythemogenic activity, resulting in increased
efficacy, reduced incidence of burning and longer
remission (2). This study aimed to assess the
usefulness of narrow band UVB (NB-UVB) therapy
in Yemeni patients with different skin conditions.
Our study is a descriptive prospective clinical
audit of 120 patients with different skin diseases
who were referred for Narrowband Ultraviolet
B (NB-UVB) therapy at the dermatology clinic
in Aden, Yemen.
All patients were treated with NB-UVB phototherapy
alone without being combined with topical steroid
or topical chemotherapy. The NB-UVB irradiation
was performed in a UV7001K phototherapy cabinet
(Waldmann, Villingen-Schwenningen, Germany)
equipped with TL-01 lamps (Philips Lighting
BV, Roosendaal, Netherlands) emitting NB-UVB
wavelengths between 311 and 313 nm. Fifty patients
were of skin type III and 70 patients were of
skin type IV.
Full history, general examination, and dermatological
examination were carried out before starting
treatment. Severity of psoriasis was ascertained
using the Psoriasis Area Severity Index (PASI)
score. The score ranges from 0 to 72.
The patients were treated three times weekly.
We started with a standard starting dose (0.3
J/cm2) and stepwise increase (20% increase of
the previous dose) depending upon the patient's
erythema response, if mild erythema occurred,
we decreased to the previous dose without further
increase, in case of moderate or severe erythema,
we stopped sessions until erythema faded and
then started with 50% of the previous dose without
further increase.
Improvement was considered as complete (75-100
%), partial (50 -75%) and no response (<50%(.
Therapeutic efficacy and responses to phototherapy
were clinically assessed by the researchers
using clinical photographs with the same digital
camera in the same position under controlled
lighting conditions at each follow-up visit.
Data were collected during the period January
2013 to May 2014.
The data was processed and analyzed by computer
using SPSS program version 17. Percentage was
calculated as summary measure for the qualitative
variables. Mean and standard deviation were
calculated for quantitative ones, to identify
any significant relationship between the study
variables. Chi-Square test was applied with
a significance level of 0.05.
Table
1
reveals
the
descriptive
characteristics
of
the
120
patients.
The
age
of
patients
ranged
between
5-54
years
with
a
mean
age
25.8
±
12.6
years.
There
were
38
(31.7%)
cases
in
the
age
group
21-30
years
followed
by
the
age
group
11-20
years.
Female
patients
represented
75
(62.5%)
of
cases.
The
majority
of
patients
came
from
Aden
governorate
93
(77.5%)
and
58
(48.3%)
of
cases
were
vitiligo,
followed
by
psoriasis
34(28.3%)
cases.
Seventy
nine
(65.8%)
of
patients
under
phototherapy
had
no
side
effect,
while
35
(29.2%)
with
hyperpigmentation,
erythema
4(3.4%)
and
flaring
and
itching
for
each
one
1(0.8%).
Table
1:
Frequency
of
selected
variables
among
the
study
patients
(n=120)
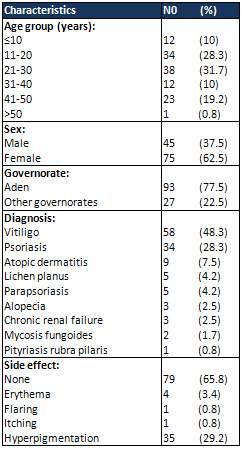
Note:
%
taken
from
total
cases
(120)
The
complete
response
appeared
in
78.3%
of
cases,
but
15%
of
cases
had
no
response
while
partial
response
was
6.7%
as
shown
in
Table
2.
Table
2:
Response
rate
of
patients
with
different
skin
diseases
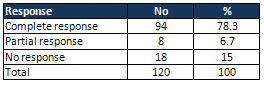
The
patients
with
mycosis
fungoid
and
atopic
dermatitis
had
high
mean
number
of
sessions
(84.50
±0.70)
and
cumulative
of
Joules
(81.69±4.02),
followed
by
the
vitiligo
with
mean
session
27.10
±23.70
and
Joules
35.18±56.89
as
appears
in
Table
3.
Table
3:
Frequency
of
study
subject
according
to
mean
number
of
sessions
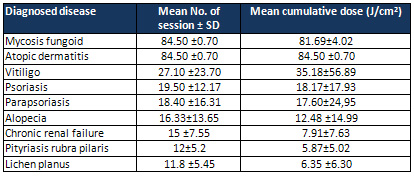
Data
are
mean
±
standard
deviation
According
to
Table
4,
all
cases
of
Lichen
planus,
Mycosis
and
Pityriasis
enrolled
in
this
study
had
complete
response
(100%)
to
treatment,
followed
by
vitiligo
with
79.3%
complete
response.
Partial
response
appears
in
patients
with
alopecia
with
66.7%
and
atopic
dermatitis
with
22.2%.
One
the
cases
with
chronic
renal
failure
had
no
response
to
treatment
with
33.3%,
followed
by
Parapsoriasis
with
20%.
There
was
a
significant
statistical
relationship
between
response
and
type
of
skin
diseases
(p=0.03).
Table
4:
Percentage
of
patients
with
degree
of
response
after
phototherapy
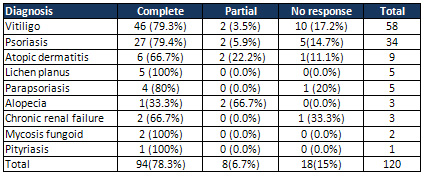
Chi-square
(p<0.05)
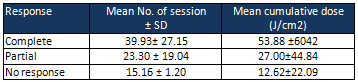
As
appears
in
Table
5
the
complete
response
by
use
NB-UVB
phototherapy
had
mean
number
of
sessions
39.93±
27.15
and
mean
cumulative
dose
of
Joules
53.88
±6042.
Table
5:
Number
of
Session
and
Dose
of
Joules
Needs
for
Complete
Response
Figure
1
and
Figure
2
show
the
vitiligo
and
psoriasis
cases
before
and
after
phototherapy.
Figure
1:
A,
Case
of
psoriasis
patient.
B,
Improvement
with
NB-UVB
after
25
sessions

Figure
2:
A,
Vitiligo
case.
B,
Repigmentation
vitiligo
patches
after
45
sessions
of
NB-UVB
treatment.
C,
after
63
sessions

NB-UVB
is
effective
in
the
treatment
of
such
skin
disorders,
like
plaque
psoriasis,
primary
cutaneous
T-cell
lymphomas,
atopic
eczema,
seborrhoeic
dermatitis,
pityriasis
rubra
pilaris,
lichen
planus,
prurigo
nodularis,
uremic
pruritus
or
even
vitiligo
(5,6).
Since
its
development,
use
of
NB-UVB
has
been
prompted
by
a
combination
of
its
therapeutic
efficacy
and
good
safety
profile
regarding
acute
adverse
events
(7,8).
Our
study
could
be
considered
as
the
first
study
in
Aden,
Yemen
to
study
the
benefit
and
outcome
of
using
NB-UVB
in
dermatology
clinic.
In
the
current
study
we
found
65.8%
of
the
patients
under
NB-UVB
had
no
side
effect,
while
29.2%
of
them
have
hyperpigmentation
and
required
time
to
resolve,
3.4%
burning
erythema.
A
study
from
Malaysia
mentioned
that
3(16.7%)
were
excluded
from
treatment
response
analyses
as
treatment
was
prematurely
discontinued
due
to
development
of
side
effects
(9).
Shamsuddin
et
al
(10)
from
Pakistan
reported
that
3(9.4%)
patients
developed
moderate
erythema
which
settled
after
using
the
standard
protocol
treatment
guidelines
while
painful
erythema
was
seen
in
none
of
their
patients.
Two
(6.3%)
patients
complained
of
itching
after
phototherapy
sessions
which
was
managed
by
regular
use
of
emollients.
Generalized
hyperpigmentation
developed
in
all
patients
and
lesional
post-inflammatory
hyperpigmentation
occurred
in
14(43.8%)
patients.
In
this
study
78.3%
of
patients
had
complete
response
to
treatment,
but
the
partial
response
in
this
study
was
6.7%.
Adauwiyah
et
al
(9)
reported
in
their
evaluation
of
repigmentation
response
to
NB-UVB,
40%
patients
had
moderate
response,
20%
had
good
response
and
another
20%
had
excellent
response
while
13.3%
patients
responded
poorly
and
6.7%
patients
did
not
show
any
repigmentation.
In
the
present
study
patients
with
mycosis
fungoid
had
complete
response
with
100%,
and
with
mean
session
84.50
±0.70
and
cumulative
of
Joules
81.69±4.02.
A
study
from
Spain
reported
that
57%
of
patients
with
mycosis
fungoid
enrolled
in
the
study
had
complete
response
(4).
Hofer
et
al
(11)
from
Austria
studied
20
patients,
6
with
early-stage
mycosis
fungoides
and
14
with
small-plaque
parapsoriasis,
demonstrating
a
histopathologically
confirmed
complete
response
in
19
cases,
after
a
mean
of
20
sessions.
The
mean
time
to
recurrence
was
6
months
after
stopping
phototherapy.
Clark
et
al
(12)
from
Scotland
observed
a
complete
response
in
6
out
of
8
patients
with
patch-stage
mycosis
fungoid
(75%
of
cases),
after
a
mean
of
26
treatment
sessions
(20-37
sessions),
that
is,
9
weeks
of
treatment.
A
study
done
by
Salah
et
al
(13)
from
Jordan
showed
complete
remission
achieved
in
76.4%
of
patients,
within
5-14
weeks
(mean
12.7
weeks).
During
this
period,
15-42
sessions
(mean
28.9
sessions),
equivalent
to
a
cumulative
NB-UVB
dose
of
17.3-48.2
J/cm2
(mean
38.7
J/cm2),
were
needed
to
achieve
this
rate
of
complete
remission.
Our
study
revealed
that
atopic
dermatitis
had
high
mean
number
of
session
84.50
±0.70
and
cumulative
of
Joules
84.50
±0.70
and
with
66.7%
complete
response.
There
is
a
large
body
of
evidence
indicating
that
NB-
UVB
is
effective
in
the
treatment
of
atopic
dermatitis
(14).
Hudson-Peacock
et
al
(15)
described
a
response
rate
of
81%
with
complete
clearance
in
43%
for
NB-UVB.
A
randomized
controlled
double
blind
study
with
73
patients
treated
with
NB-UVB,
broadband
ultraviolet
(bUVB)/ultraviolet
A
(UVA)
or
visible
light
twice
a
week
showed
NB-UVB
to
be
most
effective
(16,17).
Haroon
et
al
(18)
in
his
study
reported
the
mean
cumulative
dose
of
25.91
J/cm2
NB-UVB
at
a
wavelength
of
311nm
was
given
in
a
mean
of
duration
5.2
weeks
treatment
reduced
the
atopic
dermatitis
scores
from
mean
32.2
(range
20.2-45.5)
to
14.2
range
(6.2-12.4)
and
concluded
that
NB-
UVB
appears
to
be
a
promising
treatment
for
atopic
dermatitis.
In
the
current
study,
vitiligo
had
complete
response
in
79.3%
of
cases
(mean
session
27.10
±23.70
and
cumulative
of
Joules
35.18±56.89)
which
is
less
than
that
reported
from
study
done
in
Malaysia
in
which
repigmentation
was
moderate
in
40%
of
patients,
good
response
to
treatment
represented
in
20%,
while
20%
achieved
excellent
results
(9).
A
study
in
India
showed
that
the
majority
of
vitiligo
cases
achieved
75%
repigmentation
(complete
response)
(19).
Westerhof
et
al
(20)
and
Scherschun
et
al
(21)
achieved
up
to
75%
repigmentation
(complete
response)
in
about
two
thirds
of
patients,
while
Tjioe
et
al
(22)
reported
that
repigmentation
more
than
90%
can
even
be
observed.
In
this
study,
patients
with
psoriasis
had
complete
response
with
79.4%,
partial
5.9%
and
no
response
14.7%.
Our
finding
was
higher
than
that
reported
from
a
study
done
in
China
where
the
total
cured
was
25.6
%
and
4.7%
ineffective
or
no
response
(23).
Different
studies
reported
that
the
NB-UVB
is
more
effective
than
BB-UVB
as
a
monotherapeutic
agent
in
the
treatment
of
psoriasis
even
in
children
(24,25,26,27).
According
to
Syed
Shamsuddin
et
al
(10)
NB-UVB
is
safe
and
effective
in
the
treatment
of
psoriasis.
Psoriasis;
twenty-three
out
of
28
(93.3%)
patients
were
cleared
on
a
mean
cumulative
dose
of
42
J/cm2
within
41
sessions
over
a
period
of
13.6
weeks.
The
findings
of
this
study
revealed
that
NB-UVB
is
considered
the
first-line
phototherapeutic
option
for
many
skin
conditions,
but
large
patient
series,
different
dosing
schedules
and
long-
term
safety
considerations
should
be
carefully
evaluated
in
the
future,
to
determine
its
carcinogenic
effects.
1.
Lee
E,
Koo
J.
Modern
modified
"ultra"
Goeckerman
therapy:
a
PASI
assessment
of
a
very
effective
therapy
for
psoriasis
resistant
to
both
prebiologic
and
biologic
therapies.
J
Dermatolog
Treat.
2005;16:102-7.
2.
Takiddin
A
H,
AL-
Homsy
H
M
and
AL-
Abdulla
H.
narrow
Band
Ultraviolet
B
(NB-UVB)"
phototherapy"
in
the
treatment
of
psoriasis,
prospective
clinical
study
in
Qatar.
The
Gulf
Journal
of
Dermatology.
October
2001;
8
(2):
16-23.
3.
Nabi
H,
Shams-ud-Din
S,
Asad
F,
Nadeem
M.
Efficacy
and
safety
of
narrowband
ultraviolet
B
therapy
in
moderate
to
severe
atopic
dermatitis.
Journal
of
Pakistan
Association
of
Dermatologists
2011;
21:
106-108.
4.
Coronel-Pérez
I
M,
Carrizosa-Esquivel
A
M,
Camacho-Martínez
F.
Narrow
Band
UVB
Therapy
in
Early
Stage
Mycosis
Fungoides.
A
Study
of
23
Patients.
Actas
Dermosifiliogr.
2007;98:259-64.
5.
Bandow
G.D.,
Koo
J.Y.M.
Narrow-band
ultraviolet
B
radiation:
A
review
of
the
current
literature.
Int.
J.
Dermatol.2004;43:555-561.
6.
Berneburg
M.,
Röcken
M.,
Benedix
F.
Phototherapy
with
narrowband
vs.
broadband
UVB.
Acta
Derm.
Venereol.2005;
85:
98-108.
7.
Kunisada
M.,
Kumimoto
H.,
Ishizaki
K.,
Sakumi
K.,
Nakabeppu
Y.,
Nishigori
C.
Narrow-band
UVB
induces
more
carcinogenic
skin
tumors
than
broad-band
UVB
through
the
formation
of
cyclobutane
pyrimidine
dimer.
J.
Invest.
Dermatol.2007;
127:2865-2871.
8.
Hearn
R.M.,
Kerr
A.C.,
Rahim
K.F.,
Ferguson
J.,
Dawe
R.S.
Incidence
of
skin
cancers
in
3867
patients
treated
with
narrow-band
ultraviolet
B
phototherapy.
Br.
J.
Dermatol.
2008;159:931-935.
9.
Adauwiyah
J,
Med
M,
Mderm
A,
H
Suraiya
H.
A
Retrospective
Study
of
Narrowband-UVB
Phototherapy
for
Treatment
of
Vitiligo
in
Malaysian
Patients.
Med
J
Malaysia.
2010;
65(4):
299-301
10.
Syed
Shamsuddin,
Faria
Asad,
Muhammad
Nadeem,
Haroon
Nabi.
Efficacy
and
safety
of
narrowband
ultraviolet
B
therapy
in
psoriasis
in
Asian
skin.
Journal
of
Pakistan
Association
of
Dermatologists
2006;
16:
210-214.
11.
Hofer
A,
Cerroni
L,
Kerl
H,
Wolf
P.
Narrowband
(311-
nm)
UV-B
therapy
for
small
plaque
parapsoriasis
and
early-stage
mycosis
fungoides.
Arch
Dermatol
1999;
135:
1377-1380.
12.
Clark
C,
Dawe
RS,
Evans
AT,
Lowe
G,
Ferguson
J.
Narrowband
TL-01
phototherapy
for
patch-stage
mycosis
fungoides.
Arch
Dermatol.
2000;136:748-52.
13.
Salah
A.
Abdallat,
Ayman
S.
Alqaqaa,
Nidal
A.
Obaidat,
and
Rameh
F.
Alnueimi,
"Efficacy
and
Side
Effects
of
Narrowband-UVB
in
Early
Stage
Cutaneous
T-Cell
Lymphoma
in
Jordanian
Patients,"
ISRN
Dermatology,
vol.
2014,
Article
ID
951821,
4
pages.
14.
Collins
P,
Ferguson
J.
Narrow-band
UVB
(TL-01)
phototherapy:
an
effective
preventative
treatment
for
the
photodermatoses.
Br
J
Dermatol
1995;
132:
956-963
15.
Hudson-Peacock
MJ,
Diffey
BL,
Farr
PM.
Narrow-band
UVB
phototherapy
for
severe
atopic
dermatitis.
Br
J
Dermatol
1996;
135(2):
332.
16.
Reynolds
NJ,
Franklin
V,
Gray
JC,
Diffey
BL,
Farr
PM.
Narrow-band
ultraviolet
B
and
broad-band
ultraviolet
A
phototherapy
in
adult
atopic
eczema:
a
randomized
controlled
trial.
Lancet
2001;
357:
2012-2016.
17.
Legat
FJ,
Hofer
A,
Brabek
E,
Quehenberger
F,
Kerl
H,
Wolf
P.
Narrowband
UV-B
vs
medium-dose
UV-A1
phototherapy
in
chronic
atopic
dermatitis.
Arch
Dermatol
2003;
139:
223-224.
18.
Haroon
Nabi,
Syed
Shams-ud-Din,
Faria
Asad,
Muhammad
Nadeem.
Efficacy
and
safety
of
narrowband
ultraviolet
B
therapy
in
moderate
to
severe
atopic
dermatitis.
Journal
of
Pakistan
Association
of
Dermatologists
2011;
21:
106-108.
19.
Hari
Kishan
Kumar,
G.
Raghu
Rama
Rao,
K.
V.
T.
Gopa,
G.
Shanti,
K.
Veerabhadra
Rao.
Evaluation
of
narrow-band
UVB
phototherapy
in
150
patients
with
vitiligo.
Indian
J
Dermatol
Venereol
Leprol.
March-April
2009,
Vol
75
(2):
162-166.
20.
Westerhof
W,
Nieuweboer-Krobotova
L.
Treatment
of
vitiligo
with
UV-B
radiation
vs
topical
psoralen
plus
UV-A.
Arch
Dermatol
1997;
133:
1525-1528.
21.
Scherschun
L,
Kim
JJ,
Lim
HW.
Narrow-band
ultraviolet
B
is
a
useful
and
well-tolerated
treatment
for
vitiligo.
J
Am
Acad
Dermatol
2001;
44:
999-1003.
22.
Tjioe
M,
Gerritsen
MJ,
Juhlin
L,
van
de
Kerkhof
PC.
Treatment
of
vitiligo
vulgaris
with
narrow
band
UVB
(311
nm)
for
one
year
and
the
effect
of
addition
of
folic
acid
and
vitamin
B12.
Acta
Derm
Venereol
2002;
82:
369-372.
23.
Yan
Yuehua,
Ahmad
T.
Khalaf,
Zhai
Xiaoxiang
and
Wang
Xinggang.
Narrow-band
ultraviolet
B
and
Conventional
UVB
phototherapy
in
Psoriasis:
a
Randomised
Controlled
Trial.
American
Journal
of
Applied
Sciences
5
(8):
905-908,
2008.
24.
Van
Weelden
H,
De
La
Faille
HB,
Young
E,
van
der
Leun
JC.
A
new
development
in
UVB
phototherapy
of
psoriasis.
Br
J
Dermatol
1988;
119:
11-19.
25.
Coven
TR,
Burack
LH,
Gilleaudeau
R,
Keogh
M,
Ozawa
M,
Krueger
JG.
Narrowband
UV-B
produces
superior
clinical
and
histopathological
resolution
of
moderate-to-severe
psoriasis
in
patients
compared
with
broadband
UV-B.
Arch
Dermatol
1997;
133:
1514-1522.
26.
Dawe
RS,
Cameron
H,
Yule
S,
Man
I,
Wainwright
NJ,
Ibbotson
SH,
et
al.
A
randomized
controlled
trial
of
narrowband
ultraviolet
B
vs
bath-psoralen
plus
ultraviolet
photochemotherapy
for
psoriasis.
Br
J
Dermatol
2003;
148:
1194-1204.
27.
Pasic
A,
Ceovic
R,
Lipozencic
J,
Husar
K,
Susic
SM,
Skerlev
M,
et
al.
Phototherapy
in
pediatric
patients.
Pediatr
Dermatol
2003;
20:
71-77.
|

