This
cross-sectional
study
has
been
approved
by
Hamad
Medical
Research
Centre
under
research
No.
10014/10.
There
are
22
primary
health
care
(PHC)
centres
in
Qatar.
Of
these
centres,
16
centres
have
diabetic
clinics
providing
specialized
diabetic
services
where
a
qualified
family
physician
and
a
senior
nurse
who
have
been
trained
and
certified
as
diabetic
educators
help
in
providing
health
education
and
document
all
the
diabetes
related
data
in
a
diabetes
follow-up
sheet
which
is
supervised
and
signed
by
the
attending
physician;
so
this
study
was
targeting
Arab
Diabetic
patients
attending
primary
health
care
diabetic
clinics.
We
have
used
a
two
stage
random
sampling
where
we
have
selected
8
health
centres
out
of
16
(4
in
Doha,
the
capital
cities
and
another
4
from
other
towns).
Then
459
Diabetic
patients
of
18
years
of
age
or
older
,
with
type
1
or
type
2
diabetes
who
were
Qataris
or
any
other
Arab
nationals
have
been
recruited
through
random
sampling
by
selecting
three
days
of
the
week
and
selecting
all
diabetic
patients
attending
the
clinics.
We
have
excluded
all
women
with
gestational
diabetes,
and
those
without
a
medical
record
in
the
health
centre.
An
informed
consent
form
has
been
taken
from
each
patient
who
accepted
to
be
recruited
in
this
study.
The
primary
outcome
was
PM
which
can
be
defined
as
depression,
anxiety
and
their
related
symptoms
of
social
dysfunction
and
loss
of
confidence(10),
and
was
measured
using
the
GHQ-12
where
a
score
of
11
and
above
out
of
the
total
36
score,
is
considered
as
a
positive
case.(11)
Personal
data
were
collected
using
a
self-administered
questionnaire
that
included
the
socio-demographic
characteristics,
family
history
of
psychiatric
illness,
smoking
status,
their
willingness
to
receive
psychological
therapy
and
their
perception
about
their
glycemic
control.
Other
clinical
data
were
collected
using
a
data
extraction
sheet
from
the
patients
file
and
that
included
the
diabetes
characteristics,
presence
of
complication
and
presence
of
comorbidities.
The
participants
were
informed
about
the
nature
of
the
study,
its
purpose
and
assured
that
data
will
be
kept
anonymous
and
confidential.
Statistical
analysis:
Frequency
tables
were
used
to
describe
qualitative
data
and
mean
and
standard
deviations
were
used
to
describe
quantitative
data
while
Chi-square
test
was
used
to
compare
proportions
between
categorical
variables.
Logistic
regression
was
used
to
identify
the
most
significant
predictors
associated
with
psychological
morbidity
among
Arab
diabetic
patients.
Dichotomous
independent
variables
and
the
main
outcome
were
entered
into
the
binary
logistic
regression
model
of
the
Statistical
Package
for
the
Social
Sciences
(SPSS)
program
and
odds
ratio
(OR)
was
used
to
estimate
the
strength
of
the
relationship
between
psychological
morbidity
and
the
most
significant
predictors
associated
with
psychological
morbidity
among
Arab
diabetic
patients
using
the
backward
stepwise
(Wald)
method
in
the
logistic
regression
analysis.
A
total
of
459
Arab
diabetic
patients
were
approached
of
which
422
agreed
to
participate
giving
us
a
response
rate
of
91.9
%.
Seven
of
them
were
excluded
from
the
study
due
to
missing
data
in
their
questionnaire,
so
a
total
of
415
subjects
are
included
in
the
analysis
of
the
study.
Their
socio-demographic
characteristics
are
summarised
in
Table
1,
and
their
diabetes
characteristics
are
summarised
in
Table
2.
Table
1:
Distribution
of
socio-demographic
characteristics
of
the
study
subjects.(n=415)
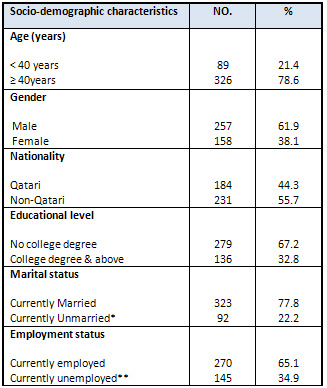
*It
includes
the
single,
divorced
and
the
widowed.
**
It
includes
the
unemployed,
retired,
students
and
housewives.
Table
2:
Distribution
of
diabetes
characteristics
of
the
study
subjects.
(n=415)
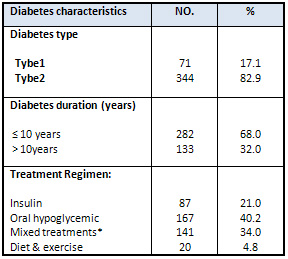
*
This
includes
those
on
insulin
and
oral
hypoglycemics
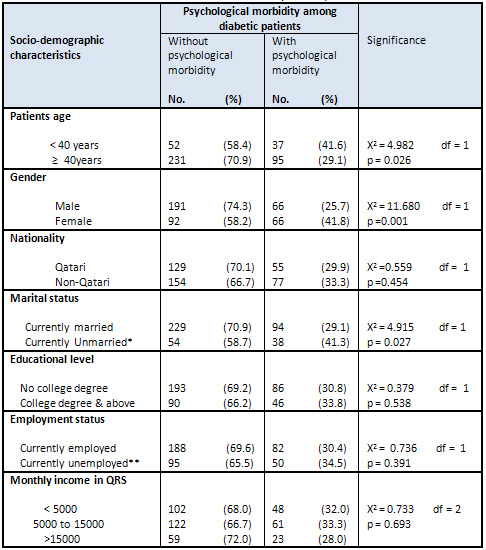
The
prevalence
of
psychological
morbidity
among
Arab
diabetic
patients
attending
primary
health
care
centres
in
Qatar
was
31.8%,
where
a
higher
percentage
of
those
in
the
early
adulthood
period
(<
40
years)
have
psychological
morbidity
than
those
in
the
middle
or
late
adulthood
period
(>
40years)
(41.6%
vs.
29.1%)
and
this
difference
is
statistically
significant
(p<0.05)
-
Table
3.
Concerning
gender
a
lower
proportion
of
males
suffer
from
psychological
morbidity
as
compared
to
females
(25.7%
vs.
41.8%)
and
this
difference
is
statistically
significant.
When
comparing
the
patients
in
terms
of
nationality,
the
percentage
of
patients
with
psychological
morbidity
is
slightly
higher
among
non-Qatari's
(33.3%)
than
Qatari's
(29.9%)
but
this
difference
did
not
reach
a
significant
value
(p>0.05).
Table
3:
Psychological
morbidity
among
diabetic
patients
according
to
their
socio-demographic
characteristics.
(n=415)
 *
It
includes
the
single,
divorced
and
the
widowed.
*
It
includes
the
single,
divorced
and
the
widowed.
**
It
includes
the
unemployed,
retired,
students
and
the
housewives.
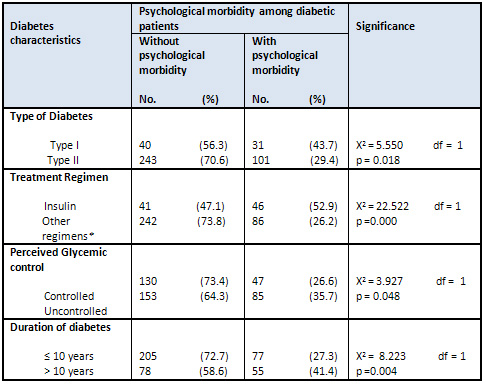
Concerning
the
patient's
diabetes
characteristics
there
is
a
significant
difference
between
them
in
terms
of
type
of
diabetes.
Higher
percentage
of
patients
with
type
I
have
psychological
morbidity
than
those
with
type
II
(43.7%
vs.29.4%),
as
shown
in
Table
4.
Conformingly
a
higher
proportion
of
patients
who
are
using
insulin
only
have
psychological
morbidity
than
those
who
are
using
other
regimens
(oral
hypoglycemic,
diet
&
exercise
or
mixed
treatments)
(52.9%
vs.
26.2%).
This
difference
is
statistically
significant.
The
percentage
of
patients
with
perceived
uncontrolled
diabetes
who
have
psychological
morbidity
are
higher
than
those
who
perceive
a
good
control
of
their
diabetes
(35.7%
vs.
26.6%).
This
difference
is
statistically
significant.
Furthermore
41.1%
of
patients
with
diabetes
duration
longer
than
10
years
suffer
from
psychological
morbidity
as
compared
to
27.3%
among
those
with
a
diabetes
duration
less
than
or
equal
to
10
years.
This
difference
is
statistically
significant.
Table
4:
Psychological
morbidity
among
diabetic
patients
according
to
their
diabetes
characteristics.(n=415)
 *
This
includes
those
on
oral
hypoglycemic,
diet
&
exercise
or
mixed
treatments.
*
This
includes
those
on
oral
hypoglycemic,
diet
&
exercise
or
mixed
treatments.
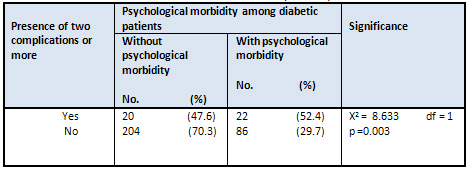
When
comparing
the
distribution
of
psychological
morbidity
among
diabetic
patients
according
to
the
existence
of
more
than
one
complication
in
the
same
individual,
higher
proportions
of
patients
with
two
or
more
complications
have
psychological
morbidity
than
those
with
no
documented
complications
(52.4%
vs.
29.7%),
Table
5.
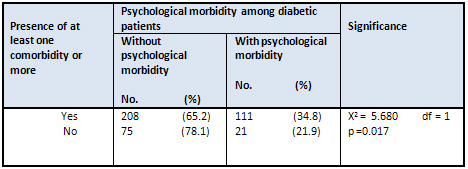
Moreover
those
who
have
at
least
one
or
more
comorbidities,
regardless
of
the
type
of
comorbidity,
have
a
higher
percentage
of
psychological
morbidity
than
those
with
no
existing
comorbid
disease
(34.8%
vs.
21.9%).
This
difference
is
statistically
significant,
as
demonstrated
in
Table
6.
Table
5:
Psychological
morbidity
among
diabetic
patients
according
to
the
presence
of
two
complications
or
more.
(n=332)
Table
6:
Psychological
morbidity
among
diabetic
patients
according
to
presence
of
at
least
one
comorbidity
or
more.
(n=415)
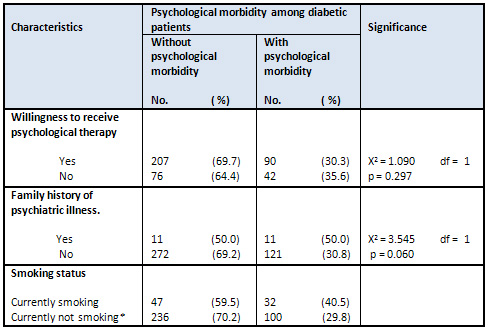
There
is
no
statistically
significant
difference
between
patients
with
psychological
morbidity
according
to
their
willingness
to
receive
psychological
therapy,
family
history
of
psychiatric
illness
and
smoking
status
(p>0.05),
as
illustrated
in
Table
7.
Table
7:
Psychological
morbidity
among
diabetic
patients
according
to
their
willingness
to
receive
psychological
therapy,
family
history
of
psychiatric
illness
and
smoking
status.
(n=415)
*This
includes
the
ex-smoker
and
those
who
never
smoked
| PREDICTORS
OF
PSYCHOLOGICAL
MORBIDITY
AMONG
ARAB
DIABETIC
PATIENTS |
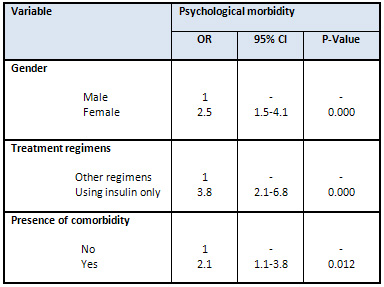
The
determinants
that
have
been
found
to
be
significantly
associated
with
psychological
morbidity
using
the
Pearson's
chi-square
test
are
re-analyzed
again
using
the
multivariate
binary
logistic
regression
to
adjust
for
the
confounding
effect
between
independent
variables
(determinants
of
psychological
morbidity)
and
the
dependent
variable
(psychological
morbidity).
Results
were
presented
in
Table
8.
Regarding
gender;
being
a
female
nearly
doubles
the
chance
of
having
psychological
morbidity
as
they
are
2.5
times
more
likely
to
have
psychological
morbidity
than
males
(OR=2.5,
95%
CI=1.5-4.1),
on
the
other
hand
patients
using
insulin
only
are
3.8
times
more
likely
to
have
psychological
morbidity
than
those
using
other
regimens
(OR=3.8,
95%
CI=2.1-6.8).
Similarly
those
patients
who
had
coexisting
morbidities
are
about
two
times
more
likely
to
have
psychological
morbidity
(OR=2.4,
95%
CI=1.1-3.8)
than
those
who
did
not.
Table
8:
The
most
significant
predictors
associated
with
psychological
morbidity
among
Arab
diabetic
patients
using
the
binary
logistic
regression
analysis
This
cross
sectional
study
explored
the
prevalence
of
psychological
morbidity
among
Arab
diabetic
patients
attending
primary
health
care
centres
in
Qatar
in
order
to
draw
the
attention
to
the
health
care
provided
to
patients
with
a
highly
prevalent
disease
in
the
country
which
is
diabetes
as
an
effort
to
improve
the
quality
of
care
provided
to
them
and
help
in
reducing
the
burden
of
this
prevalent
disease.
This
study
used
a
simple,
inexpensive,
screening
instrument,
which
has
been
used
in
different
studies
with
similar
primary
health
care
settings.
The
response
rate
in
this
study
was
91.9%
which
is
relatively
high
especially
when
we
are
addressing
psychological
morbidity
that
might
be
considered
as
a
stigma
in
the
Arab
world.
However,
the
entire
participants
were
given
a
full
explanation
of
the
nature
of
the
study
and
assurance
that
all
the
data
will
be
kept
anonymous.
Moreover
the
questionnaire
was
distributed
by
the
same
individuals
providing
the
service
i.e.
the
diabetic
educators,
making
it
more
acceptable
to
the
participants.
This
study
found
that
almost
one
third
of
the
Arab
diabetic
patients
in
Qatar
had
psychological
morbidity
(31.8%)
and
this
comes
in
agreement
with
many
international
studies
conducted
among
diabetic
patients
as
in
the
Australian
study,
which
found
that
the
prevalence
of
depression
was
30%
while
anxiety
was
35%(12)
and
similar
finding
were
reported
in
a
Greek(13)
study
and
in
a
Bangladesh
study(14).
On
the
other
hand
some
other
studies
reported
a
much
lower
prevalence
as
two
American
studies(3,
15)
reported
a
prevalence
of
10.1%
for
anxiety
and
8%
for
depression,
but
in
both
of
these
studies
a
telephone
survey
approach
was
used
and
this
might
explain
the
lower
prevalence
of
psychological
morbidities
reported
in
both
of
these
studies
as
it
might
have
excluded
people
who
do
not
have
land-line
phones
in
their
household,
the
homeless,
and
institutionalized
populations,
i.e.
the
low
social
class
people
who
might
have
a
higher
prevalence
of
psychological
morbidity.
Beside
that
people
having
psychological
morbidity
might
be
reluctant
to
answer
the
call
and
participate
in
such
a
survey.
Other
studies
found
a
much
higher
prevalence,
like
the
Iranian
study
which
reported
a
prevalence
of
depression
to
reach
as
high
as
71.8%,
but
this
study
was
conducted
in
a
hospital
setting
which
might
be
different
from
the
setting
used
in
the
present
study
in
terms
of
the
severity
of
diabetes
and
presence
of
more
severe
complications
and
or
other
comorbidities(5).
Although
studies
conducted
in
the
GCC
region
reported
a
more
or
less
similar
rates
as
the
present
study,
like
the
study
conducted
in
Bahrain(6)
and
the
UAE(7),
another
study
conducted
in
Bahrain
found
a
higher
prevalence(16)
than
the
present
study
and
this
again
might
be
explained
by
the
fact
that,
the
investigator
used
a
mixture
of
primary,
secondary
as
well
as
tertiary
level
care
as
a
setting
for
their
study,
as
this
population
might
include
cases
with
more
debilitating
complications.
In
general
the
variation
in
the
prevalence
of
PM
among
diabetic
patients
might
partly
be
explained
by
the
use
of
multiple
tools
to
assess
psychological
morbidities
such
as
the
GHQ,
PHQ,
BDI
and
the
HADS
as
well
as
whether
or
not
the
tool
used
has
been
validated
to
be
used
among
diabetic
patients
or
not.
Among
other
factors
that
might
contribute
to
this
variations
are
the
geographical
location
(urban
vs.
rural),
ethnicity
of
the
subjects
and
the
setting
of
the
study
(primary
care,
community
based,
or
hospital
based).
Gender
was
among
the
most
significant
predictors
of
PM
in
this
study
as
it
has
been
found
that
females
were
more
likely
to
have
PM
than
males
and
this
comes
in
agreement
with
many
studies(13)
and
the
fact
that
women
are
more
susceptible
to
PM
especially
depression
may
be
explained
by
the
theory
that
the
biological
and
physical
make
up
of
women
automatically
puts
them
more
at
risk
of
developing
psychological
morbidity(17)
as
from
puberty
onwards,
fluctuating
hormone
levels
affects
their
body
both
physically
and
emotionally.
Similarly,
during
and
after
pregnancy
women
may
be
particularly
vulnerable
to
depressive
disorders
such
as
postpartum
depression
and
postpartum
psychosis.
In
addition
to
biological
factors,
they
also
tend
to
be
more
affected
by
the
environment
around
them,
and
strive
for
perfection
both
physically
and
otherwise.
This
predefined
social
role,
both
increases
the
pressure,
which
they
place
on
themselves.
This
study
as
well
as
many
other
studies
reported
that
insulin
use
increases
the
likelihood
of
developing
psychological
morbidity(18,19);
this
might
be
explained
by
the
fact
that
these
patients
have
injection
related
anxiety
especially
when
the
insulin
is
self
injected,(20)
as
insulin
self-management
can
be
burdensome,
especially
when
patients
must
deal
with
their
diabetes
all
day
and
every
day,
by
self-monitoring
of
the
blood
glucose,
taking
insulin
and
making
sometimes
complex
decisions
about
insulin
dosage
in
relation
to
physical
activity
and
diet.
Other
factors,
such
as
worries
about
hypoglycemia,
gaining
weight,
the
impact
of
insulin
therapy
on
the
social
environment
and
feeling
of
failure
as
insulin
therapy
signifies
that
one
has
failed
to
manage
diabetes
with
diet/tablets(21).
Many
physicians
also
threaten
their
patients
with
insulin
as
a
final
solution
for
controlling
diabetes,
creating
a
great
feeling
of
anxiety
once
insulin
is
initiated.
Patients
also
want
to
avoid
injections
because
they
see
insulin
injections
as
a
social
stigma
that
labels
them
as
diabetic.
In
addition
those
who
are
using
insulin
only
to
control
their
diabetes,
as
in
the
present
study,
are
prone
to
more
daily
insulin
injection,
as
well
as
since
their
failure
is
intensified
as
they
think
that
no
other
treatment
could
possibly
be
effective
with
their
diabetes
and
their
one
and
only
chance
is
insulin
to
have
a
better
control.
It
is
well
known
that
most
diabetes
patients
have
a
number
of
comorbidities(22)
such
as
hypertension,
hyperlipidemia
and
the
present
study
showed
that
there
is
a
significant
relationship
between
the
presence
of
comorbidity
and
PM
by
both
univariate
and
multivariate
analysis.
This
finding
agrees
with
studies
that
explore
this
relationship
such
as
Ali
et
al.(23,24).
However,
when
comparing
each
comorbid
disease
separately
such
as
hypertension
and
hyperlipidemia,
the
study
analysis
failed
to
find
a
significant
difference,
and
this
might
be
attributed
to
the
fact
that
the
study
addressed
very
prevalent
comorbidities
in
Qatar
as
most
patients
have
them
whether
they
have
psychological
morbidity
or
not
and
maybe
the
study
did
not
have
enough
power
in
some
of
these
comorbidities
to
detect
a
significant
difference
such
as
in
asthma.
The
relationship
between
psychological
morbidity
and
age
must
be
interpreted
with
caution
as
some
studies
showed
that
psychological
morbidity
has
been
shown
to
be
common
among
younger
people
(25,26).
This
might
be
explained
by
many
factors
as
older
people
have
fewer
economic
hardships
and
fewer
experiences
of
negative
interpersonal
exchanges,
beside
younger
adults
may
be
more
reactive
to
life
stressors,
and
they
may
cope
less
effectively
with
these
conditions
than
older
adults(26).
On
the
other
hand
different
studies
showed
contradicting
results,(27)
with
depression
being
more
common
among
older
people
although
older
patients
are
less
likely
to
report
depressive
symptoms
and
they
might
have
suboptimal
cognitive
functions,
which
makes
it
difficult
to
diagnose
psychological
morbidity
among
them(28).
Diabetes
duration
has
been
addressed
in
many
studies
as
a
determinant
of
psychological
morbidity,
where
some
studies
found
that
those
with
longer
duration
of
diabetes
are
more
likely
to
have
PM
than
those
with
a
shorter
duration(13,29).
This
might
be
attributed
to
the
fact
that
living
longer
with
such
a
demanding
disease
exposes
the
individual
to
a
longer
duration
of
stress
that
might
exhaust
his
coping
resources.
Also
it
should
be
noted
that
studies
reported
that
after
ten
years,
the
likelihood
of
developing
diabetes
complications
increases
in
both
types
of
diabetes
as
reported
by
Ammari
(30)
and
Basit
et
al(31).
In
addition
this
study
did
not
show
a
significant
relationship
between
currently
smoking
and
psychological
morbidity
and
this
is
in
agreement
with
Nasser
et
al(6)
while
there
are
other
studies
that
found
a
significant
relationship
between
smoking
and
psychological
morbidity(32).
This
finding
should
be
interpreted
with
caution,
as
smoking
is
not
defined
in
the
same
way
in
many
of
the
studies
addressing
smoking.
Nevertheless,
it
should
be
worth
noting
that
the
majority
of
patients
reported
their
willingness
to
receive
psychological
therapy
when
needed
(71.6%).
This
should
encourage
the
decision
makers
in
the
country
to
consider
incorporating
preventive
psychological
interventions
into
primary
care
services
directed
towards
diabetic
patients
to
enhance
adaptation
to
diabetes
and
reduce
related
stress.
Strengths
and
limitations:
As
in
any
mental
health
screening
using
a
questionnaire,
one
cannot
rule
out
the
social
desirability
bias
or
mental
health
bias;
also
the
clinical
characteristics
in
the
study
are
based
on
the
existing
data
in
the
patient's
file,
as
the
PHC
department
are
still
in
the
process
of
developing
guidelines
which
will
help
in
standardizing
the
services
provided
in
all
PHC
centers
in
Qatar.
However,
this
study
has
its
strength,
as
although
it
is
targeting
a
sensitive
issue
in
the
Arab
world
it
manages
to
achieve
a
high
response
rate
(91.9%),
and
the
investigator
used
a
simple
inexpensive
validated
tool,
which
can
be
used
for
future
screening
of
diabetic
patients
for
psychological
morbidity.
In
addition
this
study
can
act
as
a
baseline
for
the
planning
of
preventive
mental
health
services
for
diabetics
in
Qatar.
Almost
one
third
of
Arab
diabetic
patients
attending
primary
health
care
centres
in
Qatar
have
psychological
morbidity
where
female
gender,
insulin
use
and
presence
of
multiple
comorbidities
are
the
most
significant
predictors
of
psychological
morbidity
among
them.
More
studies
need
to
be
done
in
this
field
in
order
to
identify
the
risk
factors
for
psychological
morbidity
among
people
with
chronic
disease
especially
diabetes,
and
to
improve
the
mental
health
services
that
are
offered
to
these
people
as
in
this
study
about
two
thirds
of
Arab
diabetic
patients
showed
their
interest
in
receiving
psychological
therapy
if
they
need
it.
1.
WHO.
The
Constitution
of
the
World
Health
Organization.
Official
Records
of
the
World
Health
Organization,
No.
2,
P.
100.
New
York
1948.
2.
Moussavi
S,
Chatterji
S,
Verdes
E,
Tandon
A,
Patel
V,
Ustun
B.
Depression,
chronic
diseases,
and
decrements
in
health:
results
from
the
World
Health
Surveys.
Lancet
2007;370:852-8.
3.
C.
Li,
E.S.
Ford,
T.W.
Strine,
A.H.
Mokdad,
Prevalence
of
depression
among
U.S.
adults
with
diabetes:
findings
from
the
2006
behavioral
risk
factor
surveillance
system,
Diabetes
Care
2008;31(1):105-107.
4.
Pouwer
F,
Beekman
AT,
Nijpels
G,
Dekker
JM,
Snoek
FJ,
Kostense
PJ
et
al.
Rates
and
risks
for
co-morbid
depression
in
patients
with
type
2
diabetes
mellitus:
results
from
a
community-based
study.
Diabetologia
2003;
46:
892-898.
5.
Khamseh
ME,
Baradaran
HR,
Rajabali
H.
Depression
and
diabetes
in
Iranian
patients:
a
comparative
study,
Int.
J.
Psychiatry
Med.2007;
37(1):81-86.
6.
Nasser
J,
Habib
F,
Hasan
M,
Khalil
N.
Prevalence
of
Depression
among
People
with
Diabetes
Attending
Diabetes
Clinics
at
Primary
Health
Settings.
Bahrain
Medical
Bulletin
2009;31(3):1-12.
7.
El-rufaie
OE,
Bener
A,
Ali
TA,
Abuzeid
MS.
Psychiatric
morbidity
among
type
II
diabetic
patients:
a
controlled
primary
care
survey.
Primary
Care
Psych
1997;3:189-194.
8.
Goldney
RD,
Phillips
PJ,
Fisher
LJ,
Wilson
DH.
Diabetes,
depression,
and
quality
of
life:
a
population
study.
Diabetes
Care
2004
;27(5):1066-70.
9.
McVeigh
K
H,
Mostashari
F,
Thorpe
L
E.
Serious
Psychological
Distress
Among
Persons
With
Diabetes-New
York
City,
2003.JAMA
2005;
293(4):419-420.
10.
Gao
F,
Luo
N,
Thumboo
J,
Fones
C,
Li
S
and
Cheung
Y.
Does
the
12-item
General
Health
Questionnaire
contain
multiple
factors
and
do
we
need
them?.
Health
and
Quality
of
Life
Outcomes
2004;2:63.
11.
El-Rufaie
O
E,
Bener
A,
Abuzied
M
S,
Ali
T
A.
Psychiatric
screening
among
Type
II
diabetic
patients
:Validity
of
the
General
Health
Questionnaire-12.
Saudi
medical
journal.1999;20(3):
246-250.
12.
Graco
M,
Berlowitz
DJ,
Fourlanos
S,
Sundram
S.
Depression
is
greater
in
non-English
speaking
hospital
outpatients
with
type
2
diabetes.
Diabetes
Res
Clin
Pract.
2009;83(2):e51-3.
13.
Sotiropoulos
A,
Papazafiropoulou
A,
Apostolou
O,
Kokolaki
A,
Gikas
A,
Pappas
S.
Prevalence
of
depressive
symptoms
among
non
insulin
treated
Greek
type
2
diabetic
subjects,
BMC
Res.
Notes
2008;1:101.
14.
Asghar
S,
Hussain
A,
Ali
SM,
Khan
AK,
Magnusson
A.
Prevalence
of
depression
and
diabetes:
a
population-based
study
from
rural
Bangladesh.
Diabet.
Med.
2007;24(8):872-
877.
15.
Fisher
L,
Skaff
M
M,
Mullan
T
J,
Arean
P.
A
longitudinal
study
of
affective
and
anxiety
disorders,
depressive
affect
and
diabetes
distress
in
adults
with
Type
2
diabetes.
Diabet
Med.2008;25(9):1096-1101.
16.
Almawi
W,
Tamim
H,
Al-Sayed
N,
Arekat
MR,
Al-Khateeb
GM,
et
al.
Association
of
comorbid
depression,
anxiety,
and
stress
disorders
with
Type
2
diabetes
in
Bahrain,
a
country
with
a
very
high
prevalence
of
Type
2
diabetes.
J
Endocrinol
Invest.
2008;31(11):1020-4.
17.
Kornstein
SG.
Gender
differences
in
depression:
implications
for
treatment.
J
Clin
Psychiatry
1997;
58(suppl
15):12-8.
18.
Pouwer
F,
Hermanns
N.
Insulin
therapy
and
quality
of
life.
A
review.
Diabetes
Metab
Res
Rev
2009;25
Suppl
1:S4-S10.
19.
Noh
JH,
Park
JK,
Lee
HJ,
Kwon
SK,
Lee
SH,
et
al.
Depressive
symptoms
of
type
2
diabetics
treated
with
insulin
compared
to
diabetics
taking
oral
anti-diabetic
drugs:
a
Korean
study.
Diabetes
Res
Clin
Pract
2005;69(3):243-8.
20.
Fu
AZ,
Qiu
Y,
Radican
L.
Impact
of
fear
of
insulin
or
fear
of
injection
on
treatment
outcomes
of
patients
with
diabetes.
Curr
Med
Res
Opin.
2009
;25(6):1413-20.
21.
Ahmed
U
S,
Junaidi
B,
Ali
A
W,
Akhter
O,
Salahuddin
M,
et
al.
Barriers
in
initiating
insulin
therapy
in
a
South
Asian
Muslim
community.
Diabetic
Medicine
2010;27(2):169-174.
22.
Maddigan
SL,
Feeny
DH,
Johnson
JA.
Health-related
quality
of
life
deficits
associated
with
diabetes
and
comorbidities
in
a
Canadian
National
Population
Health
Survey.
Qual
Life
Res.
2005;
14:
1311-1320.
23.
Commonwealth
of
Australia.
The
Mental
Health
of
Australians
2
Report
on
the
2007
National
Survey
of
Mental
Health
and
Wellbeing.
Commonwealth
of
Australia
.Sydney
.2009.
24.
Ali
S,
Davies
M
J,
Taub
N
A,
Stone
M
A,
Khunt
K.
Prevalence
of
diagnosed
depression
in
South
Asian
and
white
European
people
with
type
1
and
type
2
diabetes
mellitus
in
a
UK
secondary
care
population.
Postgrad
Med
J.2009;85:238-243.
25.
McCollum
M,
Ellis
SL,
Regensteiner
JG,
Zhang
W,
Sullivan
PW.
Minor
depression
and
health
status
among
US
adults
with
diabetes
mellitus.
Am
J
Manag
Care
2007;13(2):65-72.
26.
Schieman
S,
Van
Gundy
K,
Taylor
J.
The
relationship
between
age
and
depressive
symptoms:
a
test
of
competing
explanatory
suppression
influences.
J
Aging
and
Health
2002;14:260-
27.
Stekml
ML,
Vinkers
DJ,
Roos
JR,
Van
der
Mast
ATF,
Beekman
RGJ:
Natural
History
of
Depression
in
oldest
old.
Population-
Based
prospective
Study.
Brit
J
Psychiatry
2006;188:65-69.
28.
Amati
A
.
A
clinical
review
of
depression
in
elderly
people.
BMC
Geriatrics
2010,
10(Suppl
1):L28.
29.
Aikens
JE,
Perkins
DW,
Piette
JD,
Lipton
B.
Association
between
depression
and
concurrent
Type
2
diabetes
outcomes
varies
by
diabetes
regimen.
Diabet
Med
2008;25(11):1324-9.
30.
Ammari
F.
Long-term
complications
of
type
1
diabetes
mellitus
in
the
western
area
of
Saudi
Arabia.
Diabatologia
croatica
2004;33(2):59-63.
31.
Basit
A,
Hydrie
M
Z
I,
Hakeem
R,
Ahmedani
M
Y,
Masood
Q.
Frequency
of
chronic
complications
of
type
2
diabetes.
Journal
of
College
of
Physicians
and
Surgeons
Pakistan
2004;
14
(2):79-83.
32.
Haire-Joshu
D,
Heady
S,
Thomas
L,
Schechtman
K,
Fisher
EB
Jr.
Depressive
symptomatology
and
smoking
among
persons
with
diabetes.
Res
Nurs
Health
1994;17(4):273-82.

