|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................ |
Original
Contribution / Clinical Investigation
........................................................
Review Article
........................................................
Education
and Training
........................................................
Clinical
Research and Methods
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| January 2017 -
Volume 15, Issue 1 |
|
|
What can quality improvement
add to diabetes care?
Almoutaz
Alkhier Ahmed
Correspondence:
Dr. Almoutaz
Alkhier Ahmed
Diabetologist , Senior Family Medicine Specialist
MSc in diabetes , MRCGP[INT] , FESC, FAcadMEs
Dubai Health Authority - Nad Alhammar Health
Center
Dubai - UAE
Cardiff University - Wales/UK - Honorary Lecturer
Email: khier2@yahoo.com
|
Abstract
The concepts of quality should be extended
to expand over all medical specialties
putting the goal of patients' safety as
the first goal in practice.
The growing prevalence of diabetes should
be grounds for the question; Why are the
figures not going down although huge budgets
have been directed to decrease these figures?
One of the answers is the lack of investment
on a quality improvement system integrated
with clinical diabetes care.
In my review, I will discuss how the integration
between quality improvement and clinical
diabetes care could improve the outcome
of diabetes care.
Key words: Diabetes, Quality improvement,
Primary care
|
Why has diabetes mellitus
prevalence increased worldwide?
Although, there were huge efforts to control the
spread of diabetes, incidence is going up?
What have we missed in our current view on providing
diabetes care?
What do we need to know more about?
Why …..what ……where …. When
??????????
All these questions and more came to our mind
when we read the current situation of diabetes
care.
Diabetes mellitus is a group of metabolic diseases
characterized by hyperglycemia resulting from
defects in insulin secretion, insulin action,
or both. The chronic hyperglycemia of diabetes
is associated with long-term damage, dysfunction,
and failure of various organs, especially the
eyes, kidneys, nerves, heart, and blood vessels
(1).
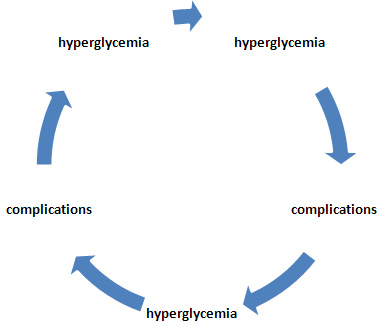
Therefore, diabetes mellitus is a dynamic disorder
running a vicious circle between hyperglycemia
and complications (Figure 1).
Figure 1: Dynamic state of diabetes
Long-term complications of diabetes include
retinopathy with potential loss of vision; nephropathy
leading to renal failure; peripheral neuropathy
with risk of foot ulcers, amputations, and Charcot
joints; and autonomic neuropathy causing gastrointestinal,
genitourinary, and cardiovascular symptoms and
sexual dysfunction. Patients with diabetes have
an increased incidence of atherosclerotic cardiovascular,
peripheral arterial and cerebrovascular disease.
Hypertension and abnormalities of lipoprotein
metabolism are often found in people with diabetes.
Quality improvement (QI) consists of systematic
and continuous actions that lead to measurable
improvement in health care services and the
health status of targeted patient groups. The
Institute of Medicine (IOM) defines quality
in health care as a direct correlation between
the level of improved health services and the
desired health outcomes of individuals and populations
(2).
Benefits of running quality improvement program:
• Improved patient health (clinical) outcomes
that involve both process outcomes (e.g., provide
recommended screenings) and health outcomes
(e.g., decreased morbidity and mortality).
• Improved efficiency of managerial and
clinical processes. By improving processes and
outcomes relevant to high-priority health needs,
the services reduce waste and costs associated
with system failures and redundancy.
• Support proactive processes that recognize
and solve problems before they occur to ensure
that systems of care are reliable and predictable.
A culture of improvement frequently develops
in service that is committed to quality, because
errors were reported and addressed.
• Improved communication with resources
that are internal and external to service, such
as, funders, civic and community organizations.
A commitment to quality shines a positive light
on the service, which may result in an increase
of partnership and funding opportunities. When
successfully implemented, a QI infrastructure
often enhances communication and resolves critical
issues.
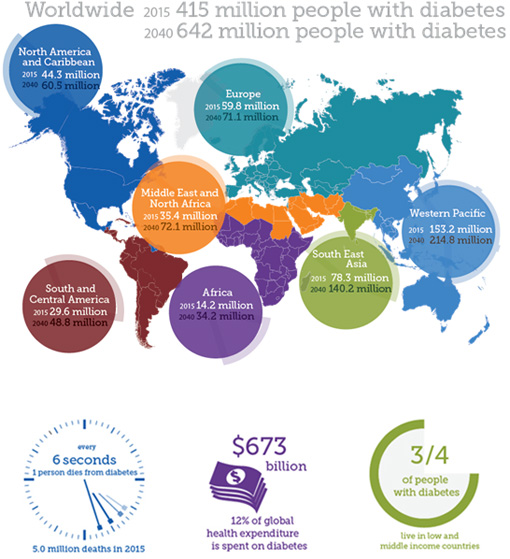
In 2015, IDF estimates that (1):
To
postulate
a
model
of
care
merging
between
practical
and
quality
improvement
concepts.
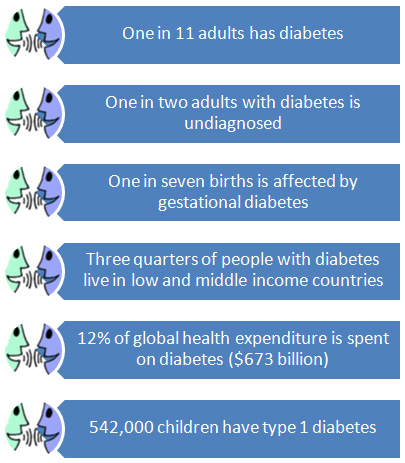
The
concept
of
quality
should
be
inspired
through
diabetes
care
services
at
their
different
levels.
The
domains
of
quality
should
encircle
diabetes
care
(Figure
2).
Figure
2:
Domains
of
quality

Diabetes
care
services
need
to
be
measurable
services.
Diabetes
care
affected
by
multiple
factors.
These
factors
can
be
classified
as
resources,
process
and
outcome
factors
(Figure
3)
(3).
Figure
3:
Inputs,
Processes
and
Outputs/Outcomes
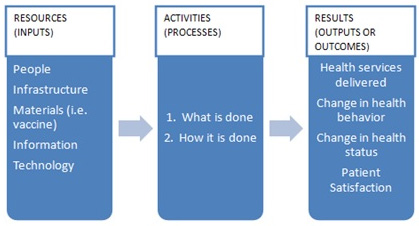
To
make
improvements,
the
service
needs
to
understand
its
own
delivery
system
and
key
processes.
The
concepts
behind
the
QI
approaches
recognize
that
both
resources
(inputs)
and
activities
carried
out
(processes)
are
addressed
together
to
ensure
or
improve
quality
of
care
(outputs/outcomes)
(4).
A
health
service
delivery
system
can
be
small
and
simple,
such
as,
diabetic
clinic,
or
large
and
complex,
like
diabetes
care
center.
QI
can
assume
many
forms
and
is
most
effective
if
it
was
individualized
to
meet
the
needs
of
a
specific
organization's
health
service
delivery
system.
A
Quality
Management
System
is
"The
organizational
structure,
processes,
procedures
and
resources
needed
to
implement,
maintain
and
continually
improve
the
management
of
quality
".
This
is
accomplished
by
creating
an
integrated
"system"
that
is
process
centered,
has
total
employee
involvement
and
is
completely
customer
focused.
Creating
a
culture
that
is
customer
focused
and
collecting
and
studying
data
that
supports
efforts
for
the
customer
are
critical
components
to
the
system.
Steps
to
Creating
quality
improvement
system
at
diabetes
care
services
(Moutaz's
Model):
1)
Clarify
Vision,
Mission
and
Values
:
All
staff
of
diabetes
care
services
with
their
different
positions
in
the
service
need
to
understand
where
the
service
is
headed
(its
vision),
what
it
hopes
to
accomplish
(mission)
and
the
operational
principles
(values)
that
will
steer
its
priorities
and
decision
making.
2)
Identify
Critical
Success
Factors
(CSF):
Critical
success
factors
help
diabetes
care
service
focus
on
those
things
that
help
it
meet
objectives
and
move
a
little
closer
to
achieving
its
mission.
3)
Develop
Measures
and
Metrics
to
Track
CSF
Data:
Once
critical
success
factors
identified,
there
needs
to
be
measurements
put
in
place
to
monitor
and
track
progress
(Figure
6).
4)
Identify
Key
Customer
Group:
Every
diabetes
care
service
has
customers
and
understanding
who
the
key
customer
groups
are
is
important
so
that
services
can
be
developed
based
on
customer
requirements.
The
mistake
a
lot
of
diabetes
care
services
make
is
not
acknowledging
their
own
staff
as
a
key
customer
group.
5)
Solicit
Customer
Feedback:
The
only
way
for
an
organization
to
know
how
well
they
are
meeting
customer
requirements
is
by
simply
asking
the
question.
There
should
be
a
structured
process
to
solicit
feedback
from
each
customer
group
in
an
effort
to
identify
what
is
important
to
them.
Diabetes
care
services
often
make
the
mistake
of
thinking
they
know
what
is
important
to
customers
and
ask
the
wrong
survey
questions
6)
Develop
Survey
Tool:
Next
develop
a
customer
satisfaction
survey
tool
that
is
based
on
finding
out
what
is
important
to
customers.
For
example,
customers
might
care
more
about
quality
than
cost
but
if
you
are
developing
a
service,
trying
to
keep
the
cost
down,
and
skimping
on
the
quality,
you
are
creating
a
service
that
might
not
meet
the
needs
of
the
customer.
7)
Survey
Each
Customer
Group:
Each
customer
group
should
have
a
survey
customized
to
their
particular
requirements
and
they
should
be
surveyed
to
establish
baseline
data
on
the
customers'
perception
of
current
practice.
This
provides
a
starting
point
for
improvements
and
demonstrates
progress
as
improvement
plans
are
implemented
8)
Develop
Improvement
Plan:
Once
the
baseline
is
established,
you
should
develop
an
improvement
plan
based
on
customer
feedback
from
each
group.
Improvement
plans
should
be
written
in
SMART
goals
format.
9)
Resurvey:
After
a
period,
resurvey
key
customers
to
see
if
scores
have
improved.
Customer
needs
and
expectations
change
over
time
so
being
in-tune
to
changing
needs
and
expectations
is
critical
to
long-term
success.
10)
Monitor
CSF:
It
is
important
to
monitor
CSF
to
ensure
there
is
consistent
progress
toward
goals.
This
also
allows
for
course
correction
should
priorities
and
objectives
change
during
the
review
period.
11)
Share
Satisfaction
Data
with
service
customers:
Once
you
have
achieved
some
positive
results
with
the
satisfaction
data,
use
it
as
an
empowering
tool!
Many
successful
diabetes
care
services
miss
the
boat
by
not
letting
others
know
what
they
do
well.
Customers
want
to
know
how
the
diabetes
care
service's
internal
processes
work
especially
if
those
processes
help
to
deliver
an
outstanding
product
or
service!
12)
Technology:
Make
sure
technology
is
user-friendly
and
supports
targeted
improvements.
For
example,
a
website
should
be
easy
to
navigate
and
the
content
should
be
easy
to
understand.
Practical
Diabetes
care
and
continuous
quality
improvement
need
to
run
together
to
produce
an
effective
system
of
diabetes
care
(figure
5)
Figure
5:
Proper
Diabetes
care
system
Measurements
of
diabetes
care
services:
Quality
measure
sets
generally
include
2
types
of
measures;
Process
measures
captures
the
rate
of
use
of
specific,
evidence-based
processes
of
care
for
example,
A1C
screening,
eye
exams
and
Outcome
measures
which
report
a
change
in
patient
condition.
For
example,
percentage
of
patients
achieving
A1C
goals
(5
-
6).
Figure
6:
Measurements
for
diabetes
care
service
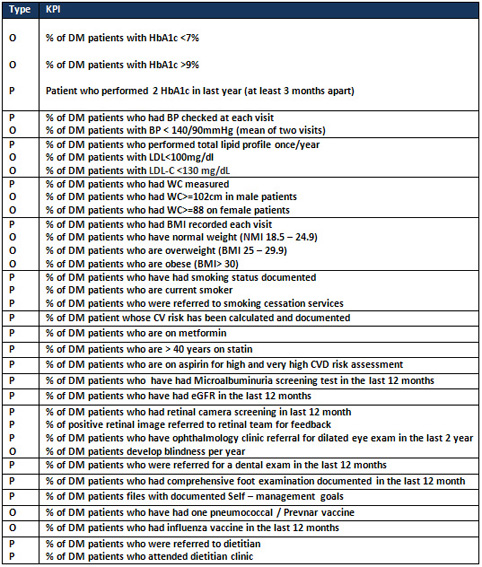
O
=
Outcome
measure;
P=
Process
measure
Implementation
of
a
quality
improvement
system
affects
positively
the
outcome
of
diabetes
care
services.
WU
Wy
and
his
colleagues
(7)
conducted
a
retrospective
comparison
study
in
eastern
New
York
state
to
assess
the
effect
of
quality
improvement
organization
activities
on
outpatient
diabetes
care.
They
concluded
that
quality
improvement
organization
activities
could
improve
outpatients'
care.
P
value
significantly
differed
(P
<0.001)
between
participating
and
non-participating
providers
on
their
performance
in
3
quality
measures.
Equality
is
one
of
the
quality
domains.
In
a
study
done
by
Thomas
D
Sequist
et
al
(8)
assessing
the
effect
of
quality
improvement
on
racial
disparities
in
diabetes
care,
the
researchers
concluded
that
racial
disparities
were
diminished
in
some
aspects
of
diabetes
care
following
variably
successful
quality
improvement.
Another
study
done
in
India
recruited
1150
patients
with
diabetes
and
poor
cardio-metabolic
profiles
who
were
randomly
assigned
to
a
multicomponent
QI
strategy
or
usual
care
for
two
and
a
half
years
(9).
Results
suggested
that
patient
in
the
QI
strategy
group
were
twice
as
likely
to
achieve
combined
diabetes
care
goals
and
larger
reductions
for
each
risk
factor
compared
with
usual
care.
Rachel
Wilf-Miron
et
al
(10)
studied
the
association
between
improved
quality
diabetes
indicators,
health
outcomes
and
costs.
They
concluded
that
their
study
demonstrates
the
effect
of
continuous
improvement
in
quality
care
indicators,
on
health
outcomes
and
resource
utilization,
among
patients
with
diabetes.
These
findings
support
the
business
case
for
quality
improvement,
especially
in
healthcare
systems
with
relatively
low
enrollee
turnover,
where
providers,
in
the
long
term,
could
"harvest"
their
investments
in
improving
quality.
Interesting
systematic
review
and
meta
analysis
by
Tricco
AC
et
al
(11)
showed
that
many
trials
of
quality
improvement
strategies
showed
improvements
in
diabetes
care.
Interventions
targeting
the
system
of
chronic
disease
management
along
with
patient-mediated
quality
improvement
strategies
should
be
an
important
component
of
interventions
aimed
at
improving
diabetes
management.
Interventions
solely
targeting
health-care
professionals
seem
to
be
beneficial
only
if
baseline
HbA1c
control
is
poor.
On
the
other
hand,
Shojania
KG
et
al
(12)
in
their
systematic
review
and
meta-analysis
concluded
that
most
quality
improvement
strategies
produced
small
to
modest
improvements
in
glycemic
control.
Team
changes
and
case
management
showed
more
robust
improvements,
especially
for
interventions
in
which
case
managers
could
adjust
medications
without
awaiting
physician
approval.
Estimates
of
the
effectiveness
of
other
specific
QI
strategies
may
have
been
limited
by
difficulty
in
classifying
complex
interventions,
insufficient
numbers
of
studies,
and
publication
bias.
In
general,
integration
of
quality
improvement
systems
and
programs
into
diabetes
care
add
to
the
outcomes
of
the
service.
Running
a
quality
improvement
system
through
practical
diabetes
care
will
change
the
process
of
care
from
static
service
into
dynamic,
changeable
service.
Isolated
practical
diabetes
care
without
continuous
quality
improvement
could
be
one
of
the
reasons
for
failure
of
controlling
diabetes
spread.
1)
IDF
atlas
,
7th
edition
2015
.
http://www.diabetesatlas.org/
(accessed
in
1/11/2016).
2)
The
Institute
of
Medicine
of
the
National
Academics
.
https://www.nationalacademies.org/hmd/Global/News%20Announcements/Crossing-the-Quality-Chasm-The-IOM-Health-Care-Quality-Initiative.aspx
(accessed
in
26/10/2016)
3)
Wagner
EH:
Chronic
disease
management:
what
will
it
take
to
improve
care
for
chronic
illness?
Effective
Clin
Pract
1:2-4,
1998
4)
Donabedian,
A.
(1988).
The
quality
of
care.
How
can
it
be
assessed?
JAMA,
260(12),
1743-1748.
5)
Pogach
L,
Aron
DC.
Sudden
acceleration
of
diabetes
quality
measures.
JAMA.
2011;305(7):709-710.
6)
Diabetes
Care
2016
Jan;
39
(Supplement
1):
S13-S22.
http://care.diabetesjournals.org/content/39/Supplement_1/S13
(accessed
in
26/10/2016)
7)
Wu
WY1,
Chen
JJ,
Shih
A.
Effect
of
quality
improvement
organization
activities
on
outpatient
diabetes
care
in
eastern
New
York
State.
Med
Care.
2006;44(12):1142-7.
8)
Sequist
TD1,
Adams
A,
Zhang
F,
Ross-Degnan
D,
Ayanian
JZ.
Effect
of
quality
improvement
on
racial
disparities
in
diabetes
care.
Arch
Intern
Med.
2006
Mar
27;166(6):675-81.
9)
Ali
MK1,
Singh
K1,
Kondal
D1,
Devarajan
et
al
.
Effectiveness
of
a
Multicomponent
Quality
Improvement
Strategy
to
Improve
Achievement
of
Diabetes
Care
Goals:
A
Randomized,
Controlled
Trial.
Ann
Intern
Med,
20;
165(6):399-408.
2016
10)
Rachel
Wilf-Miron,
Arkadi
Bolotin,
Nesia
Gordon,
Avi
Porath
and
Ronit
Peled
.The
association
between
improved
quality
diabetes
indicators,
health
outcomes
and
costs:
towards
constructing
a
"business
case"
for
quality
of
diabetes
care
-
a
time
series
study.
BMC
Endocrine
Disorders201414:92
11)
Tricco
AC,
Ivers
NM,
Grimshaw
JM,
et
al.
effectiveness
of
quality
improvement
strategies
on
the
management
of
diabetes:
a
systematic
review
and
meta-analysis.
Lancet
2012;(12)
:
2252-6.
Available
at:
http://www.thelancet.com.
12)
Shojania
KG,
Ranji
SR,
McDonald
KM,
et
al.
Effects
of
quality
improvement
strategies
for
type
2
diabetes
on
glycemic
control:
a
meta-regression
analysis.
JAMA
2006;
296:
427-40
|
|
.................................................................................................................

|
| |
|

