|
Pattern and predictors
of glycemic control among type 2 diabetics in
Armed Forces Hospital of Jizan, southwestern
Saudi Arabia
Hassan A.
Abdelwahid (1)
Saud M. Erwi (2)
Firas S. Alahmari (2)
Amani A.K. Ibrahim(3)
Hesham M. Dahlan (1)
(1) Consultant family medicine, Armed Forces
Hospital of Jizan (AFHJ)
(2) Consultant internal medicine, AFHJ;
(3) Senior registrar family medicine, AFHJ.
Correspondence:
Dr. Hassan
Ali Abdelwahid, Consultant of Family Medicine,
Armed Forces Hospital of Jizan,
PO 45911, Jizan,
Kingdom of Saudi Arabia;
and Professor of Family Medicine,
Suez Canal University.
Tel. +966 543075421;
0021093159111
Email: hassan22220000@yahoo.com
|
Abstract
Objectives:
To assess pattern and predictors of glycemic
control among type 2 diabetics based on
glycosylated hemoglobin (HbA1c) and fasting
plasma glucose (FPG).
Methods: This cross sectional study
was performed at Family Medicine and internal
medicine departments, Armed Forces Hospital
of Jizan (AFHJ), Saudi Arabia. The field
work was conducted during the period of
July 2016 to August 2016. A sample size
of 78 type 2 diabetics was calculated
and selected randomly from the study population.
The Socio-demographic and clinical data
were collected using structured questionnaires.
Also, FPG, HbA1c, total Cholesterol, Low
Density Lipoprotein (LDL), High Density
Lipoprotein (HDL), serum Triglycerides
(TG) and renal function tests (serum urea
and creatinine) were assessed using the
appropriate kits.
Results: The
total number of males was 37 (47.4%) and
that of females was 41(52.6%). Their age
ranged from 22-90 with a mean of 54.6±13
years. The mean of HbA1c was 8.79±2.17
gm % and that FPG was 180.64±42.27mg/dL.
More than two thirds of the patients in
the present study were poorly controlled.
HbA1c target, <7 gm%, was detected
only in 24.4 % (19/78). FPG, HDL and duration
of diabetes were the only significant
independent predictors of HbA1c in the
present study.
Conclusion: Poor glycemic control
and atherogenic lipid profile are highly
prevalent among the study group necessitating
aggressive screening and treatment for
dyslipidemia, and appropriate management
of diabetes.
Key words:
Type 2 Diabetes mellitus, Glycemic
control, Predictors, Glycosylated hemoglobin,
Low-density lipoprotein, High-density
lipoprotein, Triglycerides
|
Diabetes mellitus, DM, is a chronic debilitating
disease that has a serious complication if uncontrolled.
Globally, its prevalence estimates indicate
that it is approaching epidemic proportions.(1)
It was considered a disease of minor significance
to world health, now it is considered as one
the main threats to human health in the 21st
century.(2)
Worldwide, in 2014, it was estimated that almost
422 million people suffer from diabetes with
a prevalence of 8.5 %.( 3) The burden of the
disease is expected to increase to 642 million
by 2040. Diabetes caused 5 million deaths in
2015 and it is estimated that every six seconds
a person dies from diabetes. (1) The Kingdom
of Saudi Arabia is not an exception because
the prevalence of DM has been increased from
2.5% in 1982 to 23.7%(4) in 2004 due to the
westernization of life habits and increased
urbanization. (5) The long term microvascular
and macrovascular complications are also highly
prevalent among Saudi diabetics. (6)
Glycemic control is one of the primary goals
of diabetes management because it is well established
that improved glycemic control delays the onset
and retards the progression of microvascular
and macrovascular complications. (7) Glycemic
control in type 2 diabetes (DM2) patients can
be assessed by three parameters: glycosylated
hemoglobin (HbA1c), fasting plasma glucose (FPG)
and postprandial glucose (PPG). However HbA1c
is the gold standard for assessing glycemic
control. Acute glucose fluctuations could also
be involved in the pathogenesis of chronic complications
in type 2 diabetes and the treatment decisions
should not be based only on HbA1c, but should
also take into account glycemic variability.
(8) The cutoff point of HbA1c for satisfactory
diabetic control is 7% for the American Diabetes
Association (ADA) and 6.5% for the American
College of Endocrinologists. Regarding fasting
blood glucose, recommended goals are within
a range of 70-130 mg/dl (3.9-7.2 mmol/l) for
the American Diabetes Association and at <110
mg/dl (6.1 mmol/l) and 100 mg/dl (5.5 mmol/l)
for the American College of Endocrinologists
and the International Diabetes Federation. The
postprandial glucose threshold values are <180
mg/dl (American Diabetes Association) and <140
for American College of Endocrinologists and
the International Diabetes Federation. Because
of these large discrepancies that are observed
in the guidelines regarding the thresholds of
glycemic control, the ADA recommendations will
be used in the present study. (9)
Despite available health services, glycemic
control is poor in the kingdom. The results
of an interesting study that was conducted on
all patients attending the diabetic clinic of
King Khalid National Guard Hospital in Jeddah
showed that glycemic control was good in, only,
8.1% (HbA1C<7%), fair in 23.2% (HbA1C 7.1-8%),
poor in 26.6% (HbA1C 8.1-9%) and very poor in
41.9% (HbA1C >9%).(10) In order to improve
the provided care of type 2 diabetics, in Armed
Forces Hospital of Jizan (AFHJ), there is an
urgent need to study the pattern and predictors
of glycemic control based on scientific research
outcomes because there are no previous studies
dealing with that topic in AFHJ.
This cross sectional study was performed at
Family Medicine (FM) and internal medicine (IM)
departments, Armed Forces Hospital of Jizan
(AFHJ), Jizan, Saudi Arabia. Jizan is the capital
city of Jizan region that lies in the southwest
corner of Saudi Arabia on the Red Sea coast,
just north of Yemen and has a large agricultural
community. The AFHJ is a 36-bed secondary hospital
that provides health care for military personnel
and their families (approximately 50,000). The
target population included all patients eligible
for medical care in AFHJ and the study population
consisted of type 2 diabetics attending FM and
IM outpatient clinics that are affiliated to
AFHJ.
A sample size of 78 was calculated (11) from
the study population with an estimated prevalence
of diabetes to be 25% (from a previous study)(12),
95% confidence coefficient, 10% confidence interval,
and 5% non-response rate. Systematic random
sampling method was used in which every 3rd
patient, according to their order of attendance
at the reception desk, presenting to the FM
and IM clinics for care, was included in the
study.
The inclusion criteria were:
1) Type 2 diabetics,
2) age >
18 years;
3) eligibility for medical care in AFHJ; and
4) Informed consent to participate in the study.
The exclusion criteria included:
1) Patients with type 1 diabetes mellitus;
2) those for whom the study procedures would
not be feasible due to severe dementia, history
suggestive of mental retardation, or unstable
medical condition; and
3) female patients with gestational diabetes.
The field work was conducted, after we obtained
the ethical approval from the hospital Research
and Ethics committee, from July 2016 to end
of August 2016 and the study was completed in
October 2016. The operational design of the
present study included the following steps:
1) Verbal and written consent was obtained from
the participants by trained Saudi nurses for
better communications;
2) the Socio-demographic data were, also, collected
by trained Saudi nurses using pre-designed structured
questionnaire that was constructed by the researchers
to collect data about patients' characteristics
e.g. age, gender, nationality, marital status,
number of children if any, housing, income,
occupation, education level and family size.
The socio-demographic data and patients' consent
were collected before the doctor consultation.;
3) Important clinical data were collected during
the doctor consultation by the researchers,
using a predesigned structured questionnaire,
e.g. duration of DM, type of medication, family
history, the presence of diabetic complications,
height, weight, BMI, blood pressure, etc.; and
4) Venous blood samples were collected from
all the participants after at least 8 hours
of overnight fasting. Fasting plasma glucose
(FPG), glycosylated hemoglobin (HbA1C), total
Cholesterol (TC) , Low Density Lipoprotein (LD),
High Density Lipoprotein (HDL), serum Triglycerides
(TG) and renal function tests (serum urea and
creatinine) were assessed using the appropriate
kits in the hospital laboratory.
The following ethical points were taken into
consideration based on Helsinki Declaration
(13):
1) Confidentiality: the information was treated
in confidence and the names of the patients
could not be identified.
2) The activities of the research did not lead
the patients and physicians to commit acts,
which diminish their self-respect.
3) Approval of research and ethics committee
to conduct the study.
4) Written consent of the participant was taken.
5) Appropriate management of patients based
on the results of the comprehensive history
taking, physical examination and Lab work-up.
The Statistical Package for Social Sciences
(SPSS version 16.0) was used for data analysis.
Descriptive statistics and appropriate significance
tests were used according to types of variables.
Glycosylated hemoglobin and fasting plasma glucose
were compared between different categories of
important baseline socioeconomic and clinical
variables, using the group t-test. Pearson's
bivariate correlation analysis was used to assess
linear associations between HbA1c and other
continuous variables, One way analysis of variance
(ANOVA) was conducted to test the significance
of differences in HbA1c and FPG levels in different
categories of medical treatment and body mass
index (BMI). Multiple linear regression analysis
was computed to identify the predictors of glycemic
control (HbA1c). The p<0.05 was considered
the significance cut-off point.
The
study
included
78
Saudi
type
2
diabetics.
The
total
number
of
males
was
37
(47.4%)
and
that
of
females
was
41(52.6%).
Their
age
ranged
from
22-90
with
a
mean
of
54.6±13
(Table
1).
The
age
of
males
(57.9±15.9)
was
significantly
higher
(t-value,
2.1
and
P,
0.037)
than
that
of
females
(51.7±8.9),
(not
illustrated
in
Table
1).
Their
BMI
ranged
from
21-46
with
a
mean
of
31.6±6.14
kg/m2.
The
mean
of
HbA1c
was
8.79±2.17
gm
%
and
that
FPG
was
180.64±42.27mg/dL.
The
other
biochemical
findings
are
illustrated
in
Table
1.
Table
1:
Baseline
characteristics
of
the
study
group
(n,
78)
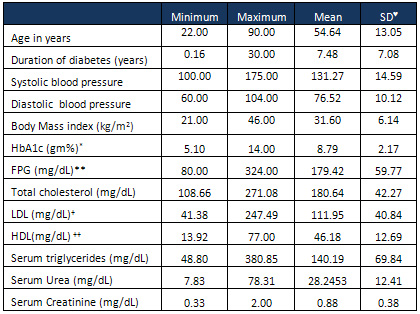
 ,
SD,
Standard
deviation;
*,
HbA1c,
Glycosylated
hemoglobin;
**,
FPG,
Fasting
plasma
glucose;
+,
LDL,
Low
Density
Lipoprotein;
and
++,
HDL,
High
Density
Lipoprotein;.
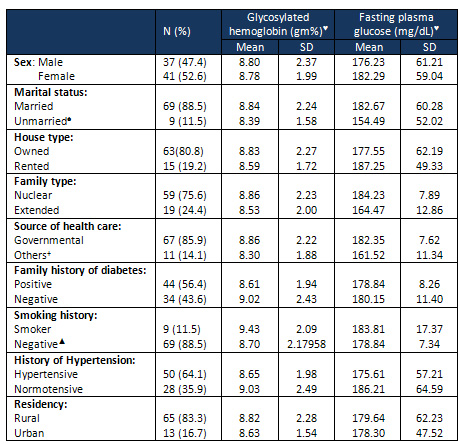
Table
2
illustrates
that
the
majority
of
the
participants
were
married
(88.5
%),
living
in
rural
areas
(83.3%)
and
had
nuclear
families
(75.6%).
Positive
family
history
of
diabetes
(56.4%)
and
present
history
of
hypertension
(64.1%)
were,
also,
highly
prevalent
among
the
study
group.
Most
of
the
patients
were
illiterate
(n=46,
59.0
%)
and
not
working
(Housewife
or
retired
Male,
n=59,
75.6%).
Glycosylated
hemoglobin
and
fasting
plasma
glucose
were
compared
between
different
categories
of
important
baseline
socioeconomic
and
clinical
variables,
using
the
group
t-test.
The
results
showed
that
there
were
no
significant
differences
between
different
categories
of
all
variables
that
are
listed
in
Table
2.
Pearson's
bivariate
correlation
analysis
was
used
to
study
the
significance
of
linear
associations
between
HbA1c
and
other
continuous
variables
(results
are
not
presented
in
Table
2).
The
results
showed
that
HbA1c
was
significantly
correlated
with
diabetes
duration
(r=0.
338,
P=0.002),
FPG
(r=0.704,
P=0.000),
total
cholesterol
(r=0.311
P=0.006),
Low
Density
Lipoprotein
(r=0.354,
P=0.001),
and
High
Density
Lipoprotein
(r=
-0.278,
P=0.014).
On
the
other
hand
there
were
no
significant
linear
associations
between
HbA1c
and
other
continuous
variables
like
age
of
patients,
serum
triglycerides,
serum
urea,
serum
creatinine,
BMI,
and
blood
pressure
(systolic
and
diastolic
blood
pressure).
Table
2:
Glycosylated
hemoglobin
and
fasting
blood
glucose
levels
in
the
different
categories
of
socioeconomic
and
clinical
variables
 ,
the
P
value
of
the
independent
t
test
>
0.05; ,
the
P
value
of
the
independent
t
test
>
0.05;
 ,
unmarried
(2
diabetics
were
single
and
7
were
widows);
+,
Governmental
health
centers,
private
and
traditional
healer/self-care; ,
unmarried
(2
diabetics
were
single
and
7
were
widows);
+,
Governmental
health
centers,
private
and
traditional
healer/self-care;
 ,
includes
48
nonsmokers
(61.5%)
and
21
Ex-smoker
(26.9%) ,
includes
48
nonsmokers
(61.5%)
and
21
Ex-smoker
(26.9%)
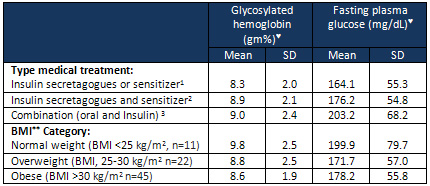
The
type
2
diabetics,
n=78,
were
classified
according
to
types
of
medical
treatment
into
3
subgroups:
group
1
received
insulin
secretagogues
or
sensitizer,
n=
24
(30.8%);
group
2
received
insulin
secretagogues
and
sensitizer,
n=
34
patient
(43.6%);
and
group
3
was
managed
by
Insulin
±
oral
hypoglycemic,
n=
20
(25.6%).
There
were
no
significant
differences
between
different
categories
of
medical
treatment
by
one
way
ANOVA.
Also
there
is
insignificant
difference
between
different
BMI
categories
regarding
HbA1c
and
FPG
as
illustrated
in
Table
3.
Table
3:
One
way
analysis
of
variance:
the
significance
of
differences
in
glycosylated
hemoglobin
and
fasting
blood
glucose
levels
according
to
type
medical
treatment
and
BMI
Category
 ,
P
of
F
ratio,
>0.05;
1,
n=
24
patient
(30.8%);
2,
n=34
patient
(43.6%);
3,
n=20
patient
(25.6%);
and
**,
BMI,
Body
Mass
Index ,
P
of
F
ratio,
>0.05;
1,
n=
24
patient
(30.8%);
2,
n=34
patient
(43.6%);
3,
n=20
patient
(25.6%);
and
**,
BMI,
Body
Mass
Index
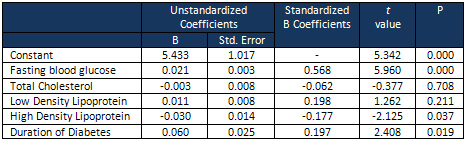
The
following
independent
variables
were
subjected
to
the
multiple
linear
regression
analysis
with
HbA1c
as
a
dependent
variable
and
FPG,
TC,
LDL,
HDL
and
duration
of
diabetes
as
independent
variables.
Table
4
illustrates
that
FPG,
HDL
and
duration
of
diabetes
were
the
only
significant
independent
predictors
of
HbA1c
in
the
present
study.
Table
4:
Predictors
of
glycosylated
hemoglobin
level
among
the
study
group
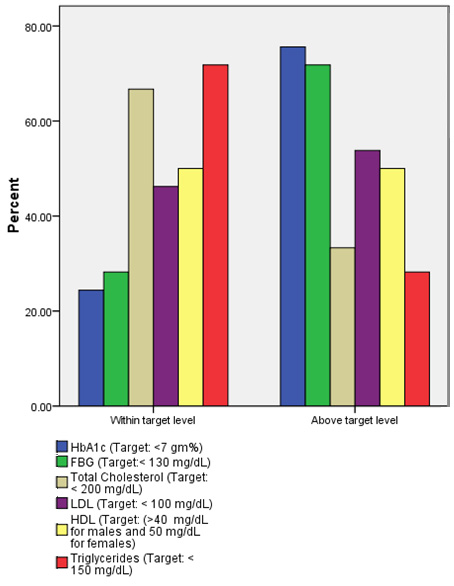
The
standard
targets
of
HbA1c,
FPG
were
detected
in
24.4
%
(19/78),
and
28.2%
(22/78)
respectively.
Also,
the
target
of
total
cholesterol,
LDL,
HDL
and
TG
were
observed
in
66.7%
(52/78),
46.2%
(36/78),
50
%
(39/78)
and
71.8%
(56/78),
respectively,
as
illustrated
in
Figure
1.
Figure
1:
Frequency
distribution
of
type
2
diabetes
based
on
standard
targets
of
glycemic
control
and
lipoproteins
(n=78)
More
than
two
thirds
of
the
patients
in
the
present
study
were
poorly
controlled
with
a
mean
of
glycosylated
hemoglobin
of
8.79±2.17
gm
%.
The
cutoff
point
for
standard
target
of
HbA1c
in
type
2
diabetics,<
7
gm%,
was
detected
only
in
24.4
%
(19/78),
a
result
that
is
consistent
with
a
nationwide
cross
sectional
study,
in
which
data
was
collected
from
28
health
centers
all
over
Kingdom
of
Saudi
Arabia
with
HbA1c
mean
of
8.20±1.89
gm%
and
only
27%
had
reached
the
target
HbA1c
of
<7
gm%.(14)
In
Saudi
Arabia,
the
prevalence
of
poor
glycemic
control
(AIC
>
7%)
among
type
2
diabetics
is
high
in
the
literature.
For
example,
it
was
67.7%(15)
in
type
2
diabetics
attending
the
Primary
Care
Clinic
of
King
Khalid
University
Hospital,
in
2012;
67.9%
in
Al
Hasa
area
of
KSA(16);
76.4%
in
Al-Madinah(17),
and
79.4%
in
patients
attending
a
primary
care
center
in
Riyadh(18).
So
we
can
conclude
that
despite
available
health
services
,
the
glycemic
control
is
poor
in
the
kingdom.
The
low
prevalence
of
good
glycemic
control
in
the
present
study,
24%,
is
consistent
with
the
reported
figures
from
other
Gulf
countries
and
some
neighbouring
Arabic
countries
where
good
glycemic
control
ranges
from
11%
to
41%.(19-24)
Also,
25%
of
European
outpatients
with
Type
2DM
had
adequate
glycemic
control
(HbA1c
<
6.5%).(25)
However
in
Canada,
the
glycemic
control
is
much
better
where
50%
of
type
2
diabetes
patients
had
HbA1c
<
7.0%,.(26)
In
the
USA,
the
mean
HbA1c
nationally
was
7.2%
in
2007-2010
according
to
the
National
Health
and
Nutrition
Examination
Survey.
However,
33-49%
of
patients
still
do
not
meet
targets
for
glycemic,
blood
pressure,
or
cholesterol
control.
(27)
Obesity
and
overweight
are
important
risk
factors
for
type
2
diabetes
and
its
glycemic
control
through
increasing
insulin
resistance.(28)
Unfortunately,
both
risk
factors
are
highly
prevalent,
among
type
2
diabetics
in
general
and
the
participants
of
the
present
study
specifically.
The
BMI
of
the
study
group
ranged
from
21-46
with
a
mean
of
31.6±6.14
kg/m2
and
prevalence
rates
of
28%
(22/78)
and
58%
(45/78)
for
overweight
and
obesity
respectively.
Despite
insignificant
linear
association
between
HbA1c
and
BMI,
the
clinical
significance
of
overweight
and
obesity
as
risk
factors
for
poor
glycemic
control
cannot
be
excluded
because
of
the
small
number
of
patients
with
normal
body
weight
among
the
study
group
and
a
further
study
with
larger
sample
size
based
on
prevalence
of
normal
weight,
overweight
and
obesity
is
recommended.
The
same
explanation
can
be
applied
to
the
results
of
bivariate
analysis,
where
there
were
no
significant
differences
between
different
categories
of
all
clinical
and
socioeconomic
variables
that
are
listed
in
Table
2,
like
marital
status,
smoking
and
hypertension.
The
bivariate
analysis
of
the
present
study
indicates
that
fasting
blood
glucose,
total
cholesterol,
LDL,
HDL
and
duration
of
diabetes
are
associated
with
glycemic
control.
However
the
regression
model
illustrates
that
FPG,
HDL
and
duration
of
diabetes
were
the
only
significant
independent
predictors
of
HbA1c.
The
finding
that
the
duration
of
diabetes
was
associated
with
poor
control
study
is
consistent
with
other
studies
and
may
be
explained
by
deterioration
of
beta
cell
function
over
time.
(7,
29,
30)
The
significant
linear
associations
between
HbA1c
and
cholesterol,
TG,
HDL
and
LDL
in
diabetic
patients,
are
in
agreement
with
the
findings
of
several
other
investigators
who
reported
significant
correlations
between
HbA1c
and
lipid
profiles
and
suggested
the
importance
of
good
management
of
diabetes
in
controlling
dyslipidaemia
(31).
The
stronger
association
of
HbA1c
with
FBG
is
supported
by
an
earlier
study
reporting
higher
correlation
coefficients
for
HbA1c
and
FPG.
(32)
HbA1c
is
a
measure
of
the
degree
hemoglobin
glycosylation
in
red
blood
cells
and
is
expressed
as
a
percentage
of
total
hemoglobin
concentration.(33)
It
reflects
the
mean
glycemic
values
in
the
previous
2-3
months
and
is
an
indicator
for
overall
glucose
exposure
reflecting
both
fasting
and
postprandial
hyperglycemia.
(34-35)
A
number
of
studies
have
reported
significant
correlation
between
HbA1c
and
FPG
levels.
(36)
However,
a
clear
understanding
of
the
relationship
between
different
plasma
glucose
measurements
and
HbA1c
is
necessary
for
achieving
specific
HbA1c
targets.(37
)
The
positive
linear
association
of
HbA1c
with
LDL
and
TG;
and
its
negative
linear
association
with
HDL
can
be
explained
by
the
fact
that
type
2
diabetes
is
associated
with
a
cluster
of
lipid
abnormalities,
including
reduced
HDL
cholesterol
and
elevated
LDL
particles
and
triglycerides
(38),
atherogenic
lipid
profile.
These
changes
are
also
a
feature
of
the
insulin
resistance
syndrome
which
is
prevalent
in
type
2
diabetes.
Also,
it
was
reported
that
efforts
to
reduce
cardiovascular
risks
resulted
in
the
improvement
of
HbA1c
even
in
the
absence
of
any
specific
intervention
targeted
at
improving
glycemic
control
(32)
indicating
the
clinical
significance
of
complex
interactions
involved
in
carbohydrate
and
lipid
metabolism.
The
atherogenic
lipid
profile
of
the
present
study
is
consistent
with
other
studies
that
were
conducted
in
the
southern
region
(39)
of
Saudi
Arabia
and
at
the
national
level
of
the
Kingdom.(40)
The
linear
associations
of
HbA1c
in
the
present
study
with
LDL,
TG
and
HDL
are
in
agreement
with
the
findings
of
other
investigators
who
reported
significant
correlations
between
HbA1c
and
lipid
profiles
and
recommended
aggressive
screening
and
treatment
for
dyslipidemia,
with
appropriate
management
of
diabetes,
as
it
is
associated
with
increased
risk
of
cardiovascular
disease.
(32,
33,
38)
The
study
has
some
limitations.
Although
the
study
sample
was
appropriately
calculated
based
on
sound
sample
size
equation,
it
was
not
large
enough
to
compute
subgroup
analysis.
Further
studies
should
be
conducted
in
the
future
with
larger
sample
sizes
to
allow
for
subgroup
analysis.
The
study
group,
also,
was
derived
from
one
practice
in
a
specific
region.
Acknowledgment:
The
authors
would
like
to
thank
Colonel
Mohammed
Hassan
Alshrani,
the
program
director
of
Armed
Forces
Hospital
of
Jizan
(AFHJ);
and
Colonel
Ali
Ibrahim
Hadi
Najdi,
assistant
program
director
of
AFHJ,
for
their
help,
support
and
encouraging
thorough
different
steps
of
the
research.
We
also
would
like
to
thank
the
Saudi
female
nurses
who
participated
in
data
collection.
The
help
of
the
health
teamwork
of
the
hospital
Lab
is
highly
appreciated.
1.
International
Diabetes
Federation
Diabetes
Atlas
,
7th
edn.
2015.
Accessed
in
May
17,
2016.
Available
at:
www.diabetesatlas.org.
2.
Laakso
M.
Cardiovascular
Disease
in
Type
2
Diabetes
From
Population
to
Man
to
Mechanisms.
Diabetes
Care.
2010
Feb;
33(2):
442-449.
3.
World
Health
Organization.
Diabetes.
Available
at:
http://www.who.int/mediacentre/factsheets/fs312/en/.
Accessed
August
15,
2016.
4.
Alqurashi
KA,
.
Aljabri
KS,
and
.
Bokhari
SA.
Prevalence
of
diabetes
mellitus
in
a
Saudi
community.
Ann
Saudi
Med.
2011
Jan-Feb;
31(1):
19-23.
5.
International
Diabetes
Federation:
Middle
East
and
North
Africa.
Saudi
Arabia,
2016.
Accessed
in
September
8,
2016.
Available
at:
http://www.idf.org/membership/mena/saudi-arabia
6.
Al-Wakeel
JS,
Hammad
D,
Al
Suwaida
A,
Mitwalli
AH,
Memon
NA,
Sulimani
F.
Microvascular
and
macrovascular
complications
in
diabetic
nephropathy
patients
referred
to
nephrology
clinic.
Saudi
J
Kidney
Dis
Transpl.
2009
Jan;20(1):77-85.
7.
Chiu
C.J,
Wray
L.A.
Factors
predicting
glycemic
control
in
middle
-aged
and
older
adults
with
type
2
diabetes.
Preventing
Chronic
Disease.
2010;7(1):A08.
Available
at:
http://www.cdc.gov/pcd/issues/2010/jan/08_0250.htm.
Accessed
September
9,
2016
8.
González
Clemente
JM1,
Cabot
GL.
Assessment
of
glycemic
control:
new
insights
into
the
evaluation
of
the
diabetic
patient.
Med
Clin
(Barc).
2010
Sep;135
Suppl
2:15-9
9.
Monnier
L
and
Colette
C.
Target
for
Glycemic
Control.
Diabetes
Care
2009
Nov;
32(suppl
2):
S199-S204.
10.
Krawagh
AM,
Alzahrani
AM,
and
Tariq
A.
Naser
TA.
Diabetes
complications
and
their
relation
to
glycemic
control
among
patients
attending
diabetic
clinic
at
King
Khalid
national
guard
hospital
in
Jeddah,
Saudi
Arabia.
Saudi
Journal
of
Internal
Medicine.
2011;
1
(1):
29-33.
11.
Sullivan
L.
Power
and
Sample
Size
Determination.
Boston
University
School
of
Public
Health.
Available
at:
http://sphweb.bumc.bu.edu/otlt/MPH-Modules/BS/BS704_Power/.
Accessed
in
June
15,
2016.
12.
Al-Rubeaan
K,
Al-Manaa
H,
Khoja
T,
Ahmad
N,
Al-Sharqawi
A,
Siddiqui
K,
AlNaqeb
D,
Aburisheh
K,
Youssef
A,
Al-Batil
A,
Al-Otaibi
M,
Al
Ghamdi
A.
The
Saudi
Abnormal
Glucose
Metabolism
and
Diabetes
Impact
Study
(SAUDI-DM).2014;
Ann
Saudi
Med
2014;
34(6):
465-475.
13.
Wikipedia,
the
free
encyclopedia.
Declaration
of
Helsinki.
Updated
9
May
2016.
Accessed
in
May
19,
2016.
Available
at:
http://en.wikipedia.org/wiki/Declaration_of_Helsinki.
14.
Al-Elq
A.
Current
practice
in
the
management
of
patients
with
type
2
diabetes
mellitus
in
Saudi
Arabia.
Saudi
Medical
Journal.
2009;30:1551-1556.
15.
Al
Rasheedi
AA.
The
Role
of
Educational
Level
in
Glycemic
Control
among
Patients
with
Type
II
Diabetes
Mellitus.
Int
J
Health
Sci
(Qassim).
2014
Apr;
8(2):
177-187.
16.
Khan
Ataur
R,
Al-Abdul
Lateef
Zaki
N,
Al
Aithan
Mohammad
A,
Bu-Khamseen
Montaser
A,
Al
Ibrahim
Ibrahim,
Khan
Shabbir
A.
Factors
contributing
to
non-compliance
among
diabetics
attending
primary
health
centers
in
the
Al
Hasa
district
of
Saudi
Arabia.
J
Family
Community
Med.2012
Jan-Apr;19(1):26-32.
17.
Almutairi
MA,
Said
S,
Zainuddin
H.
Predictors
of
Poor
Glycemic
Control
among
Type
two
Diabetic
Patients.
American
Journal
of
Medicine
and
Medical
Sciences.
2013;3(2):17-21.
18.
Al-Hussein
FA.
Diabetes
control
in
a
primary
care
setting:
a
retrospective
study
of
651
patients.
Annals
of
Saudi
Medicine.2008;
28:267-271.
19.
Al
Balushi
KA,
Al-Haddabi
M,
Al-Zakwani
I,
Al
Za'abi
M.
Glycemic
control
among
patients
with
type
2
diabetes
at
a
primary
health
care
center
in
Oman.
Prim
Care
Diabetes.
2014
Oct;8(3):239-43.
20.
Venugopal
S,
Kunju
R,
Al
Harthy
S,
Al
Zadjali
N.
Hemoglobin
A1c
in
Muscat,
Oman
-
A
3
year
study.
Oman
Med
J.
2008
Jul;23(3):170-2.
21.
Al-Sultan
FA,
Al-Zanki
N.
Clinical
epidemiology
of
Type
2
diabetes
mellitus
in
Kuwait.
Kuwait
Medical
Journal.
2005;37(2):98-104.
22.
Al-Kaabi
J,
Al-Maskari
F,
Nagelkerke
N.
Assessment
of
Dietary
Practice
among
Diabetic
Patients
in
the
United
Arab
Emirates.
Rev
Diabet
Stud.
2008
Summer;5(2):110-115.
23.
Saadi
H,
Carruthers
SG,
Nagelkerke
N,
Al-Maskari
F,
Afandi
B,
Reed
R,
et
al.
Prevalence
of
diabetes
mellitus
and
its
complications
in
a
population-based
sample
in
Al
Ain,
United
Arab
Emirates.
Diabetes
Res
Clin
Pract.
2007
Dec;78(3):369-77.
24.
Al
Khaja
KA,
Sequeira
RP,
Damanhori
AH.
Comparison
of
the
quality
of
diabetes
care
in
primary
care
diabetic
clinics
and
general
practice
clinics.
Diabetes
Res
Clin
Pract.
2005
Nov;70(2):174-82.
25.
Alvarez
Guisasola
F,
Mavros
P,
Nocea
G,
Alemao
E,
Alexander
CM,
Yin
D.
Glycaemic
control
among
patients
with
type
2
diabetes
mellitus
in
seven
European
countries:
findings
from
the
Real-Life
Effectiveness
and
Care
Patterns
of
Diabetes
Management
(RECAP-DM)
study.
Diabetes
Obes
Metab.
2008
Jun;10(Suppl
1):8-15.
26.
Leiter
LA,
Berard
L,
Bowering
CK,
Cheng
AY,
Dawson
KG,
Ekoé
JM,
et
al.
Type
2
diabetes
mellitus
management
in
Canada:
is
it
improving?
Can
J
Diabetes.
2013
Apr;37(2):82-9.
27.
Linda
M.
Siminerio,
Anastasia
Albanese-O'Neill,
Jane
L.
Chiang,
Katie
Hathaway,
Crystal
C.
Jackson,
Jill
Weissberg-Benchell,
Janel
L.
Wright,
Alan
L.
Yatvin
and
Larry
C.
Deeb.
Care
of
Young
Children
With
Diabetes
in
the
Child
Care
Setting:
A
Position
Statement
of
the
American
Diabetes
Association.
Diabetes
Care
2014
Oct;
37(10):
2834-2842.
28.
American
Diabetes
Association.
Standards
of
Medical
Care
in
Diabetes-2013.
Diabetes
Care
2013
Jan;
36(Supplement
1):
S11-S66.
Available
at:
http://dx.doi.org/10.2337/dc13-S011.
Accessed
in
September,
7,
2016.
29.
Verma
M,
Paneri
S,
Badi
P,
Raman
G.
Effect
of
increasing
duration
of
diabetes
mellitus
type
2
on
glycated
hemoglobin
and
insulin
sensitivity.
Indian
Journal
of
Clinical
Biochemistry
2006;
21:
42-146.
30.
Al-Akour
NA,
Khader
YS,
Alaoui
AM.
Glycemic
Control
and
Its
Determinants
among
Patients
with
type
2
Diabetes
Mellitus
Attending
a
Teaching
Hospital.
J
Diabetes
Metab
2011;
2:129.
31.
Ladeia
AM,
Adan
L,
Couto-Silva
AC,
Hiltner
A,
Guimarães
AC.
Lipid
profile
correlates
with
glycemic
control
in
young
patients
with
type
1
diabetes
mellitus.
Prev
Cardiol.
2006
Spring;9(2):82-8.
32.
Khan
HA
,
Sobki
SH,
Khan
SA.
Association
between
glycaemic
control
and
serum
lipids
profile
in
type
2
diabetic
patients:
HbA1c
predicts
dyslipidaemia.
Clin
Exp
Med.
2007
Mar;7(1):24-9.
33.
Pasupathi
P,
Manivannan
P
M,
Uma
M,
Deepa
M.
Glycated
haemoglobin
(HbA1c)
as
a
stable
indicator
of
type
2
diabetes
Int
J
Pharm.
Biomed
Res.
2010;1(2):53-6.
34.
Swetha
NK.
Comparison
of
fasting
blood
glucose
&
post
prandial
blood
glucose
with
HbA1c
in
assessing
the
glycemic
control.
International
J
of
Healthcare
and
Biomedical
Research.2014;2(3):134-139
35.
Rosediani
M,
Azidah
AK,
Mafauzy
M.
Correlation
Between
Fasting
Plasma
Glucose,
Post
Prandial
Glucose
and
Glycated
Haemoglobin
and
Fructosamine.
Med
J
Malaysia.
2006;
61(1):67-71.
36.
Weerarathne
TP,
Dissanayake
AS.
Value
of
assessing
post
prandial
blood
glucose
as
a
surrogate
for
fasting
blood
glucose
in
an
outpatient
medical
clinic:
a
descriptive
study.
Galle
Medical
Journal.
2006;11(1):06-09.
37.
Ketema
EB
and
Kibret
KT.
Correlation
of
fasting
and
postprandial
plasma
glucose
with
HbA1c
in
assessing
glycemic
control;
systematic
review
and
meta-analysis.
Arch
Public
Health.
2015;
73:
43.
38.
Chahil
TJ
and
Ginsberg
HN
(2006)
Diabetic
dyslipidemia.
Endocrinol
Metab
Clin
North
Am
2006;
35:
491-510
39.
Alavudeen
SS,
Dhanapal
CK,
Khan
NA,
Al
Akhali
KM,
and
Paulliah
SD.
Prevalence
and
control
of
cardiovascular
risk
factors
among
type
2
diabetes
mellitus
patients
in
southern
region
of
Saudi
Arabia.
J
Young
Pharm.
2013
Dec;
5(4):
144-147
40.
Al-Kaabba
AF,
Al-Hamdan
NA,
El
Tahir
A,
Abdalla
AM,
Saeed
AA,
and
Hamza
MA.
Prevalence
and
Correlates
of
Dyslipidemia
among
Adults
in
Saudi
Arabia:
Results
from
a
National
Survey.
Open
Journal
of
Endocrine
and
Metabolic
Diseases.
2012;
2(4):
1-9.
?
|

