When
surgery
is
performed
on
any
skin
lesion
or
subcutaneous
lump,
the
aim
is:
a.
To
completely
excise
the
lesion
and
therefore
provide
optimal
treatment
and
cure.
b.
To
preserve
normal
local
function.
c.
To
obtain
a
good
cosmetic
result.
These
principles
should
be
adhered
to
in
all
other
aspects
of
skin
surgery,
such
for
example,
the
drainage
of
an
abscess,
the
removal
of
foreign
bodies,
the
management
of
lacerations
and
trauma.
The
primary
care
practitioner
can
provide
appropriate
treatment
and
management
of
all
these
conditions.
Excision
of
skin
lesions,
management
of
lacerations
and
trauma,
plus
treatment
of
infection
and
abscess
are
among
the
most
common
type
of
problem
encountered
in
general
medical
practice.
Skin
has
a
basic
structure
but
there
are
specific
characteristics
in
each
body
area
which
need
to
be
taken
account
of
in
surgery.
The
properties
of
skin
which
may
alter
from
one
site
to
the
other
and
from
one
person
to
another
The
properties
of
skin
to
be
considered
are
as
follows:
•
Thickness,
stress
lines,
creases,
blood
supply,
elasticity,
mobility.
•
The
relationship
to
underling
vital
structures
such
as
nerves
,vessels
tendons
and
joints
is
of
the
utmost
importance.
All
of
these
influence
the
method
used
in
surgical
operations.
Each
area
of
the
body
has
its
own
particular
characteristics.
For
example:
The
blood
supply
is
poor
on
the
shin
where
the
skin
is
thin
particularly
in
the
elderly.
This
influences
how
to
treat
or
repair
pretibial
lacerations
where
suturing
may
be
under
tension
and
thus
followed
by
tissue
necrosis.
The
skin
is
thick
on
the
back.
As
well
the
distracting
forces
are
marked.
Thus
heavier
sutures
are
required
-
may
be
a
2/0
suture
as
opposed
to
a
4/0
suture.
The
sutures
may
even
be
left
in
for
2
weeks.
Maybe
remove
half
earlier.
For
3
months
the
scar
will
look
perfect
and
fine
,but
it
often
then
stretches
despite
expert
post
operative
care.
On
the
other
hand
skin
is
lax
and
mobile
on
the
dorsum
of
the
hand
and
much
easier
to
incise,
suture
and
close
a
defect
without
tension.
The
skin
over
the
sternum
has
a
propensity
for
keloid
formation.
An
incision
on
the
chest
wall
is
notorious
for
developing
a
keloid.
Race
is
also
a
significant
factor
here.
Thus
experience
alerts
you
immediately
to
the
problem
you
may
encounter
in
any
particular
area
Factors
that
must
be
considered
when
making
decisions
on
the
method
of
treatment
There
are
many
factors
that
influence
the
decision
to
operate
and
the
choice
of
method
of
treatment.
Decisions
are
often
influenced
by
the
patient's
age,
ethnicity,
community
values,
emotional
status,
patient
expectations
and
associated
medical
problems.
Cost
and
convenience
may
also
be
factors.
In
addition
there
is
often
more
than
one
way
to
treat
a
lesion.
This
needs
to
be
explained
to
the
patient
from
a
risk
management
point
of
view.
This
is
part
of
the
informed
consent
process.
An
example
here
would
be
for
basal
cell
carcinoma
where
there
may
be
a
choice
between
surgery,
radiotherapy,
photo
dynamic
therapy
and
curetting
depending
on
the
type
and
number
of
lesions,
and
even
the
training
of
the
doctor.
.
Trauma
The
program
has
been
designed
to
demonstrate
a
diagnostic
approach
using
the
methodology
of
taking
a
history
and
eliciting
physical
signs.
This
has
been
included
in
this
program
because
the
fundamentals
of
management
are
important
to
all
practitioners.
Cases
of
tetanus
still
occur.
Many
cases
occur
from
simple
gardening
injuries.
It
is
becoming
apparent
that
even
in
our
modern
society,
immunisation
is
still
a
necessity.
The
correct
treatment
of
all
wounds
is
essential.
The
principles
and
practical
aspects
of
management
should
be
learnt
by
all
those
in
the
medical
field.
As
with
any
lesion,
abscess
or
foreign
body,
a
history
of
the
onset,
mechanism
of
injury
and
total
assessment
of
the
patient
will
avoid
possible
mistaken
diagnosis
and
adverse
sequelae.
Trauma
does
not
only
involve
the
skin.
It
can
lead
to
damage
to
deeper
structures,
resulting
in
devitalisation
of
the
tissues
and
possible
injuries
to
nerve,
arteries,
veins,
muscles,
tendons,
bone
or
other
structures.
Infection
still
remains
one
of
the
major
hazards
of
wounds
and
surgical
operations.
With
any
laceration,
the
priority
is
removal
of
foreign
matter
and
devitalised
tissue.
This
mechanical
treatment
which
is
important
in
prevention
of
infection,
is
termed
debridement.
Judgement,
based
on
training
and
experience,
is
essential
in
appropriate
management
for
all
wounds.
A
decision
may
be
required
as
to
whether
the
wound
can
or
should
be
closed
and
if
not,
how
the
wound
should
be
covered.
Anaerobic
conditions
in
ischaemic
or
contaminated
tissues
can
lead
to
the
development
of
tetanus,
or
gas
gangrene,
particularly
in
the
medically
compromised
patient.
The
prevalence
of
hepatitis
B,
hepatitis
C
and
AIDs
has
drawn
attention
to
the
risk
to
which
the
health
worker
is
exposed.
Increasing
protection
is
being
sought.
Infection
control
routines
have
been
set
up
in
most
clinical
practices.
Gloves,
masks
and
goggles
have
assumed
a
new
role
in
clinical
practice,
both
in
the
office
surgery
setting
and
operating
theatre.
Rather
than
relaxing
criteria
because
of
the
availability
of
antibiotics,
infection
control
procedures
have
assumed
increasing
importance.
In
many
Australian
hospitals
we
are
losing
the
battle
against
antibiotic
resistant
organisms
and
chronic
infections,
making
the
GP
office
a
more
attractive
environment
for
minor
surgical
procedures.
Office
surgery
has
increased
rapidly
as
costs
of
hospitalization
have
soared.
The
isolation
of
body
substance
is
now
recommended,
for
blood
and
all
body
fluids
are
potentially
infectious.
Aseptic
technique
is
practiced
not
just
when
the
patient
is
thought
to
be
in
a
high
risk
group,
for
example,
a
drug
user
or
homosexual,
but
as
a
routine.
Key
Concepts
and
Practice
Tips.
o
Assess
all
significant
skin
characteristics
in
the
region
before
attempting
surgery.
o
Always
consider
the
functional
and
cosmetic
implications
when
planning
incisions.
o
Consider
factors
which
may
compromise
healing
(e.g.
vascular
disease)
or
affect
the
cosmetic
result
(e.g.
keloid
tendency)
in
the
particular
patient
or
site.
o
All
dead
tissue
and
foreign
material
must
be
removed
from
traumatic
wounds.
o
Remember
that
superficial
appearances
may
conceal
damage
to
deeper
vital
structures.
o
Assess
the
site,
number
and
depth
of
foreign
bodies
(clinically,
by
ultrasound
and
by
X-ray
if
necessary
)
before
attempting
removal.
o
A
foreign
body
may
present
as
an
abscess
some
time
after
the
initial
injury.
o
Allow
sufficient
time
to
find
and
remove
a
foreign
body.
Ensure
approach
planned
before
starting.
Consideration
needs
to
be
given
to
attaining
a
bloodless
field
by
use
of
a
tourniquet.
o
A
cutaneous
lump
may
be
due
to
a
lesion
in
any
layer
or
appendage
of
the
skin,
or
in
underlying
tissues.
o
Accurate
clinical
assessment
and
diagnosis
is
vital.
o
When
operating
on
a
skin
lesion,
beware
of
underlying
important
motor
nerves
which
are
superficial
at
specific
sites
(e.g.
mandibular
branch
of
facial
nerve
over
the
body
of
mandible,
the
accessory
nerve
in
posterior
triangle
of
neck,
and
the
lateral
popliteal
nerve
over
neck
of
fibula).
Motor
nerves
or
sensory
nerves
may
be
in
danger.
Sensory
may
include
nerves
such
as
the
supratrochlear,
supra
orbital
or
occipital
in
the
forehead
and
scalp.
Others
to
be
aware
of
are
the
post
auricular
and
greater
auricular
of
the
ear.
The
knowledge
of
the
anatomy
of
these
nerves
enables
simple
nerve
block
to
be
performed.
Once
again
the
skin
over
the
ear
is
taut
and
painful
to
infiltrate
with
local
anaesthetic
and
thus
a
nerve
block
may
be
appropriate.
o
Avoid
splashing
antiseptics
into
the
eyes
or
on
mucosa.
o
Alcoholic
skin
preparations
should
not
be
used
on
sensitive
areas
of
the
skin
(e.g.
scrotum)
and
can
ignite
when
in
contact
with
diathermy.
o
Incisions
should
be
placed
in
skin
creases
where
they
are
obvious
(particularly
in
the
trunk,
neck
and
face).
Avoid
incisions
which
cross
joint
lines,
pressure
areas,
hair
lines
and
eyebrows.
Always
align
mucocutaneous
junctions.
The
first
stitch
does
this,
then
follow
up
with
the
remainder
of
the
suturing
o
Areas
with
poor
blood
supply
(e.g.
skin
over
the
tibia)
may
not
heal
well.
o
Excess
tissue
tension
impairs
blood
supply
to
the
wound
edge
and
delays
healing.
o
Areas
with
a
rich
blood
supply
(e.g.
scalp,
face
and
neck)
tend
to
bleed
more
readily
but
heal
well.
o
Beware
of
factors
(e.g.
aspirin,
anti
platelet
and
anticoagulants
or
even
a
family
or
past
history)
,which
may
increase
bleeding.
Surgery
may
proceed
in
some
cases
but
the
risks
need
to
be
considered
and
explained.
Extra
care
is
required.
There
are
some
circumstances
where
these
medications
can
be
modified
and
others
where
they
cannot.
o
Excess
bleeding
may
lead
to
the
formation
of
a
haematoma
and
subsequent
infection
can
cause
an
abscess.
o
Apply
pressure
as
a
first
measure
to
control
excessive
or
unexpected
bleeding
during
the
procedure..There
are
other
techniques
to
control
bleeding.
o
All
deep
wounds
should
be
closed
in
layers.
o
Avoid
leaving
a
dead
space
by
suturing
deeper
layers
separately
or
by
deep
through
and
through
sutures
(in
trunk).
o
Avoid
adherence
of
skin
to
deeper
structures
(which
can
result
in
a
depressed
scar)
by
subcutaneous
sutures
apposing
fascia
and
muscular
layers.
o
Fat
does
not
hold
sutures
well.
o
If
there
is
a
high
risk
of
infection,
delay
closure
of
the
wound.
o
Interrupted
sutures
into
the
skin
edge
aid
haemostasis
particularly
in
vascular
areas.
o
Everted
edges
heal
better-
quicker
and
with
a
better
scar
than
inverted
edges.
o
Mattress
sutures
help
to
evert
the
skin
edges
preventing
inversion
which
delays
healing.
o
A
subcuticular
suture
only
opposes
the
epidermis
and
dermis.
o
To
some
patients
the
fear
of
suture
removal
may
be
greater
than
that
of
the
operation.
o
Some
regions
can
tolerate
some
tension
to
bring
edges
together.
However,
in
the
fingers,
lower
leg,
foot
or
palm
only
minimal
tension
is
permissible.
o
Err
on
the
side
of
leaving
sutures
in
place.
If
there
is
any
doubt,
do
not
remove
all
of
them
at
the
one
time.
This
will
prevent
wound
disruption.
o
If
sutures
appear
too
tight
and
causing
ischaemia,
early
removal
is
advisable.
o
Leave
sutures
for
a
longer
time
in
areas
under
greater
tension
with
a
poor
blood
supply
or
with
any
other
factors
which
may
delay
healing.
o
A
better
scar
is
obtained
by
using
a
large
number
of
fine
sutures
rather
than
fewer,
heavier
sutures
more
widely
spread.
o
Think
of
ways
to
reduce
wound
tension
and
swelling
(e.g.
firm
dressings,
immobilization,
splints).
o
Bandages
which
are
too
tight
impair
blood
supply.
o
Elevation
of
the
limb
minimises
postoperative
swelling.
o
Follow
up
carefully
so
that
postoperative
complications
can
be
detected
and
treated
promptly.
o
Advise
the
patient
to
report
urgently
any
increasing
pain,
swelling,
discolouration,
odour
or
fever.
I
hope
these
simple
tips
will
assist
you
in
the
office
when
taking
care
of
your
patients
and
we
will
continue
to
present
some
further
tips
and
visual
examples
of
surgery
techniques
in
the
coming
series.
Series
One
-
Lacerated
Left
index
finger
in
35
year
old
theatre
sister
This
was
a
clean
incised
kitchen
wound
with
a
sharp
knife.
It
is
on
the
volar
aspect
of
the
index
finger.It
has
been
poorly
managed
due
to
the
basic
error
of
not
examining
the
finger
for
nerve
or
tendon
injury.

Presenting
injury
The
patient,
a
theatre
assistant
had
presented
to
casualty
with
a
bleeding
finger
and
complaining
about
numbness.
After
a
long
wait
local
anaesthetic
was
infiltrated
through
the
wound.
The
patient
had
complained
that
the
bleeding
was
profuse
and
continued
to
spurt
when
pressure
was
released.

Injury
prepared
for
surgery
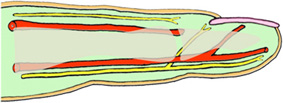
Side
view
Arteries
and
nerves

Sutured
The
wound
was
eventually
sutured.

Incorrect
splinting
Note
that
the
splinting
is
incorrect.

Correctly
splinted
now
The
finger
is
correctly
splinted
this
time
in
the
position
of
function.This
avoids
stiffness
caused
by
immobilization.

5
weeks
later

Post
stiffness
The
scrub
nurse
complained
to
the
surgeon
in
her
theatre
2
days
later
about
the
numbness
on
one
side
of
the
finger.This
lead
to
a
referral
for
digital
nerve
repair.
There
was
also
a
tendon
repair
of
a
partially
divided
flexor
tendon
.The
skin
was
sutured
this
time
with
a
synthetic
absorbable
3/0
vicryl
suture.Not
my
preference
and
it
can
be
seen
there
is
a
severe
inflammatory
reaction
with
the
sutures
being
spat
out
intermittently.This
occurs
more
commonly
with
the
multifilamented
or
braided
suture.
The
images
demonstrate
that
the
initial
immobilization
was
with
a
straight
splint.This
was
incorrect.This
could
lead
to
permanent
stiffness.Six
months
later
there
is
still
some
restriction
on
flexion
of
the
finger.
Interestingly
:ANATOMICALLY
1-
With
the
fingers
and
toes
the
nerves
are
superficial
to
the
arteries
.Thus
if
an
artery
is
divided
(suggested
by
it
spurting)
a
nerve
is
likely
to
have
been
divided.As
well
there
is
a
chance
there
is
a
tendon
injury.
2-
Examination
must
be
carried
out
before
the
local
is
used.
3-
Whilst
local
can
be
injected
directly
into
a
laceration
it
may
be
advisable
to
avoid
the
swelling
in
fingers
to
allow
better
inspection-
Thus
do
a
digital
block.
4-
Splinting
of
fingers,unless
there
is
a
specific
reason
should
be
in
position
of
function
-
not
as
in
this
case.This
is
to
avoid
stiffness.
5-
Some
surgeons
will
use
absorbable
sutures
in
the
skin
-
It
would
not
be
my
choice
because
of
increased
reaction
with
a
braided
suture.
Absorbable
sutures
are
used
in
the
skin
by
some
surgeons,because
they
may
not
need
to
be
removed
and
thus
there
is
possibly
less
pain.This
also
saves
the
surgeon
time.

