|
PRINCIPLES
OF
SURGERY
-
ANO
RECTAL
REGION
|

I
mage
attribution
:
Eizenberg
et
al.
‘Anatomedia’
©
Anatomedia
Publishing
P/L
Melbourne
2003
ISBN
0-734-2691-9
Anatomy
of
the
region
The
Ano
rectal
region
is
a
transitional
zone
from
normal
skin
to
mucosa.
Note
the
clinical
significance
of
the
upper
&
lower
parts
of
the
anal
canal
in
terms
of:
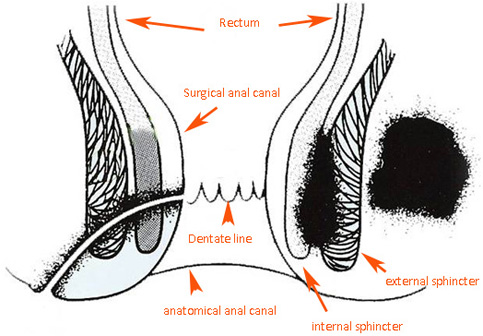
.Lining
-mucosa
above,
adenoma
or
adenocarcinoma
,Squamous
below,
squamous
cell
carcinoma
or
melanoma
Nerves
Above
the
dentate
line
-
sensory
and
motor
to
parasympathetic
hypogastric
plexus
Below
the
dentate
line
-
Sensory
&
motor
-
pudendal
nerve
Lymphatic
drainage
-
to
internal
ilia
above,inguinal
groin
below
The
anal
canal
contains
sensory
nerves.
Above
the
pectinate
line
visceral
afferents
accompany
parasympathetic
nerves.
Below
the
pectinate
line,
somatic
afferents
are
in
the
pudendal
nerve.
Anal
canal
-
arterial
supply
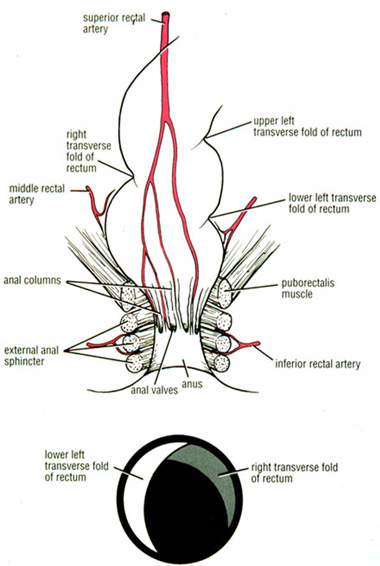 Image:
Image:
Richard
Snell,
'Clinical
Anatomy
for
medical
students'
5th
ed.
fig
7.4
Little,
Brown
&
Co
1995
ISBN
0-316-80135-6
Arterial
supply
to
mucosa
above
the
pectinate
line,
is
via
the
superior
rectal
artery
(direct
continuation
of
inferior
mesenteric
artery)
and
to
mucosa
below
pectinate
line
via
the
inferior
rectal
artery
(branch
of
internal
pudendal
artery).
Note:
anastomosis
across
pectinate
line
and
middle
rectal
artery
(branch
of
internal
iliac
artery)
supplies
muscle
wall
only.
Venous
drainage
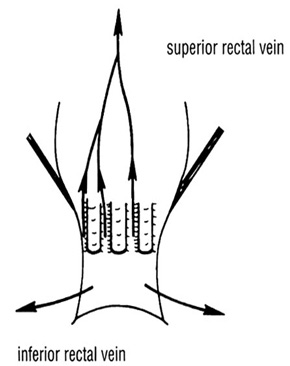
Image:
Richard
Snell,
'Clinical
Anatomy
for
medical
students'
5th
ed.
fig
8.7c
Little,
Brown
&
Co
1995
ISBN
0-316-80135-6
Venous
drainage
above
the
pectinate
line
is
via
the
superior
rectal
vein
(drains
to
portal
system
via
inferior
mesenteric
vein)
and
below
the
pectinate
line
via
the
middle
and
inferior
rectal
veins
(drains
to
systemic
system
via
internal
iliac
vein).
Note
communications
between
these
veins
form
an
important
portal-systemic
anastomosis.
Anal
canal
-
lymph
drainage
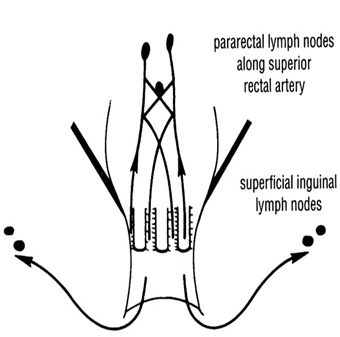
image:
Richard
Snell,
'Clinical
Anatomy
for
medical
students'
5th
ed.
fig
8.7d
Little,
Brown
&
Co
1995
ISBN
0-316-80135-6
Mucosa
above
the
pectinate
line
drains
to
inferior
mesenteric
nodes
and
below
the
pectinate
line
drains
to
superficial
inguinal
nodes
(medial
group).
Thus
if
there
are
nodes
in
the
groin,
either
inflammatory
or
neoplastic
the
anal
region
must
be
examined
Note
this
area
is
both
in
the
midline
and
a
junctional
zone
(between
endoderm
&
ectoderm)
where
lymphatics
communicate.
It
is
therefore
a
significant
watershed
area
of
lymph
drainage.
Diagnosis
of
haemorrhoids
is
made
from
patient
history
of
bleeding
and
confirmed
by
physical
examination
(type
of
bleeding
and
protrusion).
Haemorrhoids
are
typically
3,7,11
o’clock
positions
with
the
patient
viewed
in
the
left
lateral
position.
.
 Image
attribution
:
Image
attribution
:
Maurice
Brygel
©
Melbourne
Hernia
Clinic
2006
Significance
of
type
of
haemorrhoids
Different
treatments
are
available
depending
on
the
type
of
haemorrhoid:
types
1
&
2
conservative
treatment,
injection
or
rubber
band
ligation
types
3
&
4
usually
require
surgery
Examination
 Image
attribution
:
Image
attribution
:
Maurice
Brygel
©
Melbourne
Hernia
Clinic
2007
This
shows
the
haemorrhoids
in
the
3,7,11
o’clock
position.They
are
thrombosed.
The
largest
in
the
left
lateral
position
is
ulcerated.With
surrounding
oedema.
They
are
not
suitable
for
banding
as
below
the
dentate
line.
Surgery
in
severe
cases
may
be
delayed
to
allow
swelling
to
settle.This
makes
surgery
simpler
and
reduces
the
risk
of
removing
too
much
skin
&
mucosa
causing
anal
stenosis.
Examination
involves
inspection,
palpation,
proctoscopy,
sigmoidoscopy.
The
anal
margin
is
inspected
and
the
patient
asked
to
strain.This
may
actually
cause
the
haemorrhoid
to
protrude.Other
protrusions
could
be
a
prolapse
or
polyp.
Rectal
examination
may
feel
the
haemorrhoidal
cushions.You
may
even
be
able
to
prolapse
a
polyp.
With
proctoscopy
you
can
assess
the
haemorrhoids
as
the
patient
strains.
Sigmoidoscopy
will
rule
out
higher
lesions.
Rubber
Band
Ligation
for
Haemorrhoids
Banding
has
many
advantages
over
the
haemorrhoid
operation.
However
not
all
haemorrhoids
are
suitable
for
rubber
band
ligation.
This
is
a
simpler
office
or
room’s
treatment
for
haemorrhoids
as
opposed
to
surgery.
No
anaesthetic
is
required
and
the
patient
is
able
to
go
home
almost
immediately.
There
should
be
minimal
pain
following.
There
is
minimal
time
off
work.
More
than
1
session
may
be
required
for
large
haemorrhoids.
The
main
serious
but
uncommon
complication
is
secondary
haemorrhage,
a
complication
common
for
all
anal
procedures.
With
surgery,
Hospitalization
and
General
anaesthesia
is
usually
required.
The
post
operative
course
is
often
very
painful.
However
permanent
cure
is
usually
achieved.
The
use
of
a
local
anaesthetic
block
or
infiltration
helps
avoid
one
of
the
side
effects
of
acute
retention
of
urine.
This
is
because
there
is
less
pain.
I
actually
perform
many
anal
or
haemorrhoidal
procedures
in
the
office
under
local
anaesthesia
because
patients
cannot
get
into
hospital.

Demonstration
of
rubber
band
application
Haemorrhoids
-
staging
A
guide
to
severity
and
preferred
treatment
Stage
1
-
Bleed,
particularly
at
the
toilet
-
the
blood
may
drip
or
splash
into
the
bowl
or
colour
the
toilet
paper.If
mixed
with
the
stools
suggest
this
is
from
a
higher
lesion.
Stage
2
-
Prolapse
-
usually
with
straining
of
the
bowels.
They
return
inside
spontaneously
Stage
3
-
or
need
to
be
pushed
back
inside.
Stage
4
-
Thrombose
and
prolapse
-
this
is
very
painful
and
the
haemorrhoid
cannot
be
returned
inside
-
not
suitable
for
banding
and
surgery
may
be
required.
Perianal
haematoma
-
A
different
problem
Phenol
in
almond
oil
is
injected
just
above
the
haemorrhoid
through
a
proctoscope.
The
inflammatory
response
occluded
the
veins.
The
main
risks
are
tissue
necrosis,
and
prostatitis
if
injected
into
prostate.
Secondary
haemorrhage
7-10
days
later
may
occur.
Some
prefer
this
to
banding.
Perianal
haematomas
are
quite
a
common,very
painful
condition.
They
may
occur
following
straining
at
the
toilet.
They
are
called
a”
five
day
wonder”
because
they
usually
resolve
within
five
days.
They
occur
because
of
rupture
of
the
perianal
venous
plexus.
A
perianal
hematoma
is
easily
recognized
by
its
position
just
outside
the
anal
verge.
It
is
usually
well
circumscribed
and
has
a
bluish
appearance.
It
is
quite
regular
in
shape
just
like
a
little
marble.
It
is
tender
to
touch.
This
perianal
lump
should
not
be
confused
with
a
thrombosed
intro
external
hemorrhoid.
They
do
sometimes
however
coexist
together.
Attempted
drainage
of
a
thrombosed
Intero
external
hemorrhoid
by
incision
will
only
aggravate
the
problem
so
it
is
important
to
distinguish
the
two.This
is
usually
done
by
looking
at
the
appearance
and
position.

They
can
be
treated
with
analgesia
and
sitz
baths.Creams
or
gels
can
also
be
applied.
For
example
a
2%
lignocaine
jelly.
However
many
do
require
surgery
as
the
symptoms
continue.
They
are
very
painful.
For
this
reason
surgery
is
often
undertaken.
Another
reason
to
operate
is
because
they
rupture
and
bleed
and
thus
become
messy
and
unhygienic.
Anal
tag
-
sentinal
pile
hiding
mid
line
posterior
fissure

At
the
first
visit
a
rectal
examination
with
a
glove
is
performed.
Then
the
bowel
above
the
haemorrhoids
is
examined
with
a
sigmoidoscope
to
exclude
other
causes
of
bleeding
from
the
bowel.
In
patients
over
45
a
colonoscopy
may
need
to
be
arranged
to
ensure
no
other
cause
for
the
bleeding
is
present.
The
surgery
can
be
carried
add
in
the
office
quite
simply
by
those
experienced
at
it.
This
is
done
under
local
anaesthetic
using
lignocaine
with
adrenaline.
The
area
is
infiltrated
directly
with
just
a
few
CC.
A
small
incision
will
allow
the
hematoma
to
be
evacuated.
To
control
any
bleeding
and
to
keep
the
wound
open
a
small
pack
is
inserted.
Suturing
is
not
required.
The
patient
actually
keeps
their
underwear
on
during
the
procedure
so
that
the
dressing
does
not
dislodge
as
they
get
up.
.
A
pad
is
placed
on
the
dressing
to
prevent
any
ooze
and
the
underwear
pulled
up
.The
pain
usually
is
relieved
quickly
although
painkillers
may
be
used
for
a
day
or
two..
.
The
patient
is
told
to
have
a
bath
or
shower
the
following
day.The
pack
falls
out
and
the
wound
heals
spontaneously
by
what
is
termed
healing
by
second
intention.
are
They
instructed
to
apply
pressure
if
there
is
any
unusual
amount
of
bleeding.
Review
is
not
mandatory.
Injecting
the
local
anaesthetic.A
fine
25
gauge
needle
is
used
to
reduce
the
pain.
This
is
not
injected
directly
into
the
haematoma
as
this
causes
further
pain
due
to
increased
tension.
Injection
directly
into
the
overlying
epidermis
gives
immediatea
anesthesia.
Once
the
incision
is
made
further
local
can
be
injected
into
the
depths
of
the
wound.
Incision
This
is
made
in
a
radial
direction
in
the
skin
grace.
Some
would
use
a
cruciate
incision
as
this
does
not
close
as
rapidly.
However
I
believe
this
gives
an
irregular
scar
which
can
be
lumpy
and
sensitive.
|
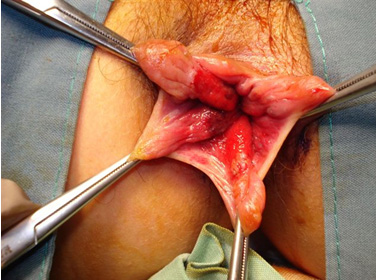
SERIOUS
HAEMORRHOID
PRESENTATIONS
|

Thrombosed
gangrenous
haemorrhoid
with
oedema
The
risk
management
here
is
to:
a)
Establish
a
diagnosis,
b)
Recommend
treatment.
Not
all
haemorrhoids
require
surgical
intervention
and
alternative
treatments
for
each
problem
should
be
offered.
It
should
be
remembered
for
any
anal
procedure
that
the
post-operative
recovery
can
be
very
painful
particularly
if
a
complication
occurs.
Thus
the
patient
needs
to
be
adequately
warned
about
the
possibility
of
pain
and
the
possibility
of
fainting
with
pain
or
due
to
psychological
responses.
Thus
for
any
anorectal
condition
a
diagnoses
can
usually
be
readily
established.
a)
Establish
a
diagnosis,
b)
Recommend
treatment.
Not
all
haemorrhoids
require
surgical
intervention
and
alternative
treatments
for
each
problem
should
be
offered.
It
should
be
remembered
for
any
anal
condition
gentleness
is
required
while
establishing
the
diagnosis.
Also
for
any
procedure
that
the
post-operative
recovery
can
be
very
painful
particularly
if
a
complication
occurs.
Thus
the
patient
needs
to
be
adequately
warned
about
the
possibility
of
pain
and
the
possibility
of
fainting
.Many
haemorrhoid
problems
can
be
treated
surgically
in
the
office.
This
will
be
demonstrated
in
future
in
Brygels
SURGISKILLS.
The
next
issue
will
feature
Anal
Abscess
and
Fistula.
1.
M.
Brygel.
Video
Book
of
Surgery.
2.
Eizenberg
et
al
‘Anatomedia’
©
Anatomedia
Publishing
P/L
Melbourne
2003
CD
ROM.
ISBN
0-734-2691-93.
M.
Brygel.
Ano
Rectal
Condiitons.
CD
ROM.
medi+WORLD
International.
2009
4.
Richard
Snell,
‘Clinical
Anatomy
for
medical
students’
5th
ed.
fig
7.4
Little,
Brown
&
Co
1995
ISBN
0-316-80135-6

