|
Red blood cell supports
in severe clinical conditions in sickle cell
diseases
Mehmet Rami
Helvaci (1)
Nesrin Atci (2)
Orhan Ayyildiz (3)
Orhan Ekrem Muftuoglu (3)
Lesley Pocock (4)
(1) Medical Faculty of the Mustafa Kemal University,
Antakya, Professor of Internal Medicine, M.D.
(2) Medical Faculty of the Mustafa Kemal University,
Antakya, Assistant Professor of Radiology, M.D.
(3) Medical Faculty of the Dicle University,
Diyarbakir, Professor of Internal Medicine,
M.D.
(4) Lesley Pocock, Publisher, medi+WORLD International
Correspondence:
Mehmet Rami Helvaci, M.D.
Medical Faculty of the Mustafa Kemal University,
31100, Serinyol, Antakya, Hatay, TURKEY
Phone: 00-90-326-2291000 (Internal 3399) Fax:
00-90-326-2455654
Email: mramihelvaci@hotmail.com
|
Abstract
Background:
Sickle cell diseases (SCDs) are accelerated
atherosclerotic processes. We tried to
understand whether or not there is a prolonged
survival with the increased number of
red blood cells (RBC) transfusion in the
SCDs.
Methods: As one of the significant
endpoints of the SCDs, cases with chronic
obstructive pulmonary disease (COPD) and
without, were collected into the two groups.
Results: The
study included 428 patients (221 males).
There were 71 patients (16.5%) with COPD.
Mean age was significantly higher in the
COPD group (32.8 versus 29.8 years, P=0.005).
Male ratio was significantly higher in
the COPD group, too (78.8% versus 46.2%,
P<0.001). Smoking (35.2% versus 11.4%,
P<0.001) and alcohol (7.0% versus 1.9%,
P<0.01) were also higher among the
COPD cases. Beside these, priapism (14.0%
versus 3.0%, P<0.001), HCV RNA positivity
(2.7% versus 0.5%, P<0.05), cirrhosis
(8.4% versus 3.3%, P<0.05), leg ulcers
(23.9% versus 12.0%, P<0.01), digital
clubbing (25.3% versus 6.7%, P<0.001),
coronary heart disease (23.9% versus 13.7%,
P<0.05), chronic renal disease (15.4%
versus 7.0%, P<0.01), stroke (16.9%
versus 8.1%, P<0.01), and mean transfused
RBC units in their lives (63.8 versus
33.0, P=0.003) were all higher among the
COPD cases. This was probably due to the
higher number of transfused RBC units;
the mean age of mortality was also higher
in the COPD group, significantly (38.3
versus 30.4 years, P=0.04).
Conclusion:
SCDs are chronic catastrophic processes
on vascular endothelium terminating with
accelerated atherosclerosis induced end-organ
failures in early years of life. RBC supports
in severe clinical conditions probably
prolong survival of the patients.
Key words: Sickle
cell diseases, chronic endothelial damage,
red blood cell support
|
Chronic endothelial damage may be the major
cause of aging and mortality by inducing disseminated
cellular hypoxia all over the body. Much higher
blood pressure (BP) of the afferent vasculature
may be the major underlying cause, and probably
whole afferent vasculature including capillaries
are mainly involved in the process. Some of
the well-known accelerators of the inflammatory
process are physical inactivity, weight gain,
smoking, and alcohol for the development of
irreversible endpoints including obesity, hypertension,
diabetes mellitus, cirrhosis, peripheric artery
disease (PAD), chronic obstructive pulmonary
disease (COPD), chronic renal disease (CRD),
coronary heart disease (CHD), mesenteric ischemia,
osteoporosis, teeth loss, and stroke, all of
which terminate with early aging and mortality.
They were researched under the title of metabolic
syndrome in the literature, extensively (1,
2). Similarly, sickle cell diseases (SCDs) are
chronic catastrophic processes on vascular endothelium
particularly at the capillary level, and terminate
with accelerated atherosclerosis induced end-organ
failures in early years of life. Hemoglobin
S (HbS) causes loss of elastic and biconcave
disc shaped structures of red blood cells (RBCs).
Probably loss of elasticity instead of shape
is the main problem because sickling is rare
in peripheric blood samples of patients with
associated thalassemia minors, and human survival
is not so affected in hereditary spherocytosis
or elliptocytosis. Loss of elasticity is present
in whole lifespan, but exaggerated with increased
metabolic rate of the body. The hard RBCs induced
prolonged endothelial inflammation, edema, and
fibrosis mainly at the capillary level terminate
with cellular hypoxia all over the body (3-5).
Capillary vessels are mainly involved in the
process due to their distribution function for
the hard RBCs. We tried to understand whether
or not there is a prolonged survival with the
increased number of RBC supports in the SCDs
in the present study.
The study was performed in Medical Faculty
of the Mustafa Kemal University between March
2007 and February 2016. All patients with the
SCDs were studied. The SCDs are diagnosed with
the hemoglobin electrophoresis performed via
high performance liquid chromatography (HPLC).
Medical histories including smoking habit, regular
alcohol consumption, painful crises per year,
transfused RBC units in their lives, surgical
operations, priapism, leg ulcers, and stroke
were learnt. Patients with a history of one
pack-year were accepted as smokers, and one
drink-year were accepted as drinkers. A complete
physical examination was performed by the same
internist. Cases with prominent teeth loss (8
or more) were detected. Cases with acute painful
crisis or another inflammatory event were treated
at first, and the laboratory tests and clinical
measurements were performed on the silent phase.
A check up procedure including serum iron, iron
binding capacity, ferritin, creatinine, liver
function tests, markers of hepatitis viruses
A, B, and C and human immunodeficiency virus,
a posterior-anterior chest x-ray film, an electrocardiogram,
a Doppler echocardiogram both to evaluate cardiac
walls and valves and to measure systolic BP
of pulmonary artery, an abdominal ultrasonography,
a venous Doppler ultrasonography of the lower
limbs, a computed tomography of brain, and a
magnetic resonance imaging (MRI) of hips were
performed. Other bones for avascular necrosis
were scanned according to the patients' complaints.
Associated thalassemia minors were detected
with serum iron, iron binding capacity, ferritin,
and hemoglobin electrophoresis performed via
HPLC. The criterion for diagnosis of COPD is
post-bronchodilator forced expiratory volume
in one second/forced vital capacity of less
than 70% (6). Acute chest syndrome (ACS) is
diagnosed clinically with the presence of new
infiltrates on chest x-ray film, fever, cough,
sputum production, dyspnea, or hypoxia (7).
An x-ray film of abdomen in upright position
was taken just in patients with abdominal distention
or discomfort, vomiting, obstipation, or lack
of bowel movement, and ileus was diagnosed with
gaseous distention of isolated segments of bowel,
vomiting, obstipation, cramps, and with the
absence of peristaltic activity on the abdomen.
Systolic BP of the pulmonary artery of 40 mmHg
or higher is accepted as pulmonary hypertension
(8). CRD is diagnosed with a persistent serum
creatinine level of 1.3 mg/dL in males and 1.2
mg/dL in females. Cirrhosis is diagnosed with
physical examination, hepatic function tests,
ultrasonographic results, and tissue sample
in case of indication. Digital clubbing is diagnosed
with the ratio of distal phalangeal diameter
to interphalangeal diameter which is greater
than 1.0, and with the presence of Schamroth's
sign (9, 10). An exercise electrocardiogram
is just performed in cases with an abnormal
electrocardiogram and/or angina pectoris. Coronary
angiography is taken just for the exercise electrocardiogram
positive cases. So CHD was diagnosed either
angiographically or with the Doppler echocardiographic
findings as the movement disorders in the cardiac
walls. Rheumatic heart disease is diagnosed
with the echocardiographic findings, too. Avascular
necrosis of bones is diagnosed by means of MRI
(11). Stroke is diagnosed by the computed tomography
of brain. Ophthalmologic examination was performed
according to the patients' complaints. Eventually
as one of the significant endpoints of the SCDs,
cases with COPD and without were collected into
the two groups, and they were compared in between.
Mann-Whitney U test, Independent-Samples t test,
and comparison of proportions were used as the
methods of statistical analyses.
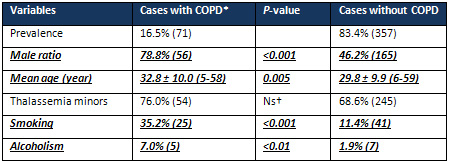
The
study
included
428
patients
with
the
SCDs
(207
females
and
221
males)
during
the
nine-year
follow-up
period.
There
were
71
patients
(16.5%)
with
COPD.
Mean
age
of
the
patients
was
significantly
higher
in
the
COPD
group
(32.8
versus
29.8
years,
P=0.005).
The
male
ratio
was
significantly
higher
in
the
COPD
group,
too
(78.8%
versus
46.2%,
P<0.001).
Smoking
(35.2%
versus
11.4%,
P<0.001)
and
alcohol
consumption
(7.0%
versus
1.9%,
P<0.01)
were
also
higher
among
the
COPD
cases.
Prevalences
of
associated
thalassemia
minors
were
similar
in
both
groups
(76.0%
versus
68.6%
in
the
COPD
group
and
other,
respectively,
P>0.05)
(Table
1).
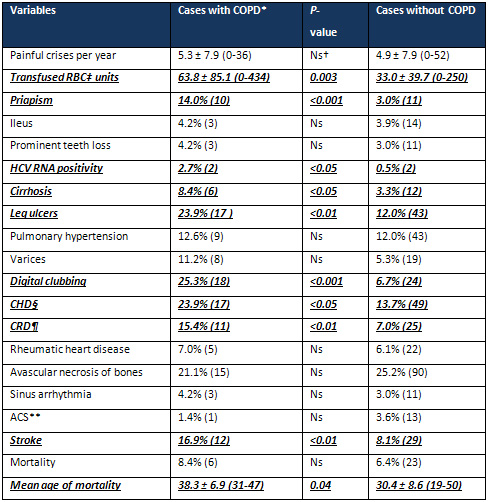
Beside
these,
priapism
(14.0%
versus
3.0%,
P<0.001),
cirrhosis
(8.4%
versus
3.3%,
P<0.05),
leg
ulcers
(23.9%
versus
12.0%,
P<0.01),
digital
clubbing
(25.3%
versus
6.7%,
P<0.001),
CHD
(23.9%
versus
13.7%,
P<0.05),
CRD
(15.4%
versus
7.0%,
P<0.01),
and
stroke
(16.9%
versus
8.1%,
P<0.01)
were
all
higher
in
the
COPD
group.
Additionally,
painful
crises
per
year
(5.3
versus
4.9),
ileus
(4.2%
versus
3.9%),
prominent
teeth
loss
(4.2%
versus
3.0%),
pulmonary
hypertension
(12.6%
versus
12.0%),
varices
(11.2%
versus
5.3%),
rheumatic
heart
disease
(7.0%
versus
6.1%),
sinus
arrhythmia
(4.2%
versus
3.0%),
and
mortality
(8.4%
versus
6.4%)
were
all
higher
among
the
COPD
cases,
too
but
the
differences
were
nonsignificant
probably
due
to
the
small
sample
size
of
the
COPD
group.
Parallel
to
the
above
consequences,
mean
transfused
RBC
units
in
their
lives
were
significantly
higher
among
the
COPD
cases
(63.8
versus
33.0,
P=0.003).
Probably
due
to
the
higher
number
of
transfused
RBC
units
in
their
lives,
the
mean
age
of
mortality
was
significantly
higher
in
the
COPD
group
(38.3
versus
30.4
years,
P=0.04)
(Table
2).
On
the
other
hand,
there
was
one
patient
(1.4%)
with
HBsAg
positivity
in
the
COPD
group
and
4
patients
(1.1%)
among
the
others
(P>0.05),
but
HBV
DNA
was
positive
in
none
of
them
by
polymerase
chain
reaction
(PCR)
method.
Although
antiHCV
positivity
was
similar
in
both
groups
(4.2%
versus
6.1%
of
the
COPD
patients
and
others,
respectively,
P>0.05),
HCV
RNA
positivity
was
significantly
higher
in
the
COPD
group
(2.7%
versus
0.5%
of
the
COPD
group
and
other,
respectively,
P<0.05)
by
PCR.
On
the
other
hand,
there
were
three
patients
with
the
sickle
cell
retinopathy
in
the
group
without
COPD.
Table
1:
Characteristic
features
of
the
study
cases
*Chronic
obstructive
pulmonary
disease
†Nonsignificant
(P>0.05)
Table
2:
Associated
pathologies
of
the
study
cases
 *Chronic
obstructive
pulmonary
disease
†Nonsignificant
(P>0.05)
‡Red
blood
cell
§Coronary
heart
disease
Chronic
renal
disease
**Acute
chest
syndrome
*Chronic
obstructive
pulmonary
disease
†Nonsignificant
(P>0.05)
‡Red
blood
cell
§Coronary
heart
disease
Chronic
renal
disease
**Acute
chest
syndrome
Chronic
endothelial
damage
may
be
the
most
common
type
of
vasculitis,
and
the
leading
cause
of
aging
and
mortality
in
human
beings.
Physical
inactivity,
weight
gain,
smoking,
alcohol,
prolonged
infections,
and
chronic
inflammatory
processes
including
SCDs,
rheumatologic
disorders,
and
cancers
may
accelerate
the
process.
Probably
whole
afferent
vasculature
including
capillaries
are
mainly
involved
in
the
process.
Much
higher
BP
of
the
afferent
vasculature
may
be
the
major
underlying
cause
by
inducing
recurrent
micro-injuries
on
endothelium.
Thus
the
term
of
venosclerosis
is
not
as
famous
as
arteriosclerosis
or
atherosclerosis
in
the
literature.
Secondary
to
the
chronic
endothelial
inflammation,
edema,
and
fibrosis,
vascular
walls
become
thickened,
their
lumens
are
narrowed,
and
they
lose
their
elastic
nature
that
reduces
blood
flow
and
increases
BP
further.
Although
early
withdrawal
of
causative
factors
may
delay
final
consequences,
after
development
of
cirrhosis,
COPD,
CRD,
CHD,
PAD,
or
stroke,
endothelial
changes
cannot
be
reversed
completely
due
to
the
fibrotic
nature
of
them
(12).
SCDs
are
life-threatening
hereditary
disorders
nearly
affecting
100,000
individuals
in
the
United
States
(13).
As
a
difference
from
other
causes
of
chronic
endothelial
damage,
they
probably
keep
vascular
endothelium
particularly
at
the
capillary
level
(14),
since
the
capillary
system
is
the
main
distributor
of
the
hard
RBCs
to
the
tissues.
The
hard
cells
induced
chronic
endothelial
damage,
inflammation,
edema,
and
fibrosis
build
up
an
advanced
atherosclerosis
in
younger
ages
of
the
patients.
As
a
result,
mean
lifespans
of
the
patients
were
48
years
in
females
and
42
years
in
males
in
the
literature
(15),
whereas
they
were
33.6
and
30.8
years
in
the
present
study,
respectively.
The
great
differences
may
be
due
to
delayed
diagnosis
of
the
diseases,
delayed
initiation
of
hydroxyurea
therapy,
and
inadequate
RBC
supports
in
severe
clinical
conditions
in
our
country.
Actually,
RBC
supports
must
be
given
whenever
there
is
evidence
of
clinical
deterioration
in
the
patients
(16,
17).
RBC
supports
decrease
sickle
cell
concentration
in
circulation
and
suppress
bone
marrow
about
the
production
of
abnormal
RBCs.
So
they
decrease
sickling
induced
endothelial
damage
of
organs
in
crises.
According
to
our
nine-year
experience,
simple
and
repeated
transfusions
are
superior
to
RBC
exchange.
First
of
all,
preparation
of
one
or
two
units
of
RBC
suspensions
each
time
rather
than
preparation
of
six
units
or
higher
provides
time
for
clinicians
to
prepare
more
units
by
preventing
sudden
death
of
such
patients.
Secondly,
transfusions
of
one
or
two
units
of
RBC
suspensions
each
time
decreases
the
severity
of
pain
and
relaxes
anxiety
of
the
patients
and
surroundings
in
a
short
period
of
time.
Thirdly,
transfusions
of
lesser
units
of
RBC
suspensions
each
time
by
means
of
simple
transfusions
will
decrease
transfusion-related
complications
in
the
future.
Fourthly,
transfusion
of
RBC
suspensions
in
secondary
health
centers
may
prevent
some
deaths
developed
during
transport
to
tertiary
centers
for
the
exchange.
On
the
other
hand,
longer
lifespan
of
females
in
the
SCDs
(15)
and
longer
overall
survival
of
females
in
the
world
(18)
cannot
be
explained
by
the
atherosclerotic
effects
of
smoking
and
alcohol
alone,
instead
it
may
be
explained
by
physical
power
requiring
role
of
males
that
may
terminate
with
an
exaggerated
sickling
and
atherosclerosis
all
over
the
body
(19).
COPD
is
the
third
leading
cause
of
mortality
with
different
underlying
etiologies
in
the
world
(20).
It
is
an
inflammatory
disorder
mainly
affecting
the
pulmonary
vasculature,
and
smoking,
excess
weight,
and
aging
may
be
the
major
causes.
Regular
alcohol
consumption
may
also
take
place
in
the
inflammatory
process.
For
example,
the
prevalence
of
alcohol
consumption
was
significantly
higher
in
the
COPD
group
(7.0%
versus
1.9%,
P<0.01),
here.
Similarly,
COPD
was
one
of
the
most
frequent
associated
disorders
in
alcohol
dependence
in
another
study
(21).
Additionally,
30-day
readmission
rate
was
higher
in
COPD
patients
with
alcoholism
(22).
Probably
an
accelerated
atherosclerotic
process
is
the
main
structural
background
of
functional
changes
that
are
characteristics
of
COPD.
The
endothelial
process
is
enhanced
with
release
of
various
chemicals
by
inflammatory
cells,
and
terminates
with
endothelial
fibrosis
and
tissue
loss
in
lungs.
Although
COPD
may
mainly
be
an
accelerated
atherosclerotic
process
of
the
pulmonary
vasculature,
there
are
several
reports
about
coexistence
of
disseminated
endothelial
inflammation
all
over
the
body
(23,
24).
For
example,
close
relationships
were
shown
between
COPD,
CHD,
PAD,
and
stroke
(25).
Similarly,
two-thirds
of
mortality
cases
were
caused
by
cardiovascular
diseases
and
lung
cancers
in
smokers
in
a
multi-center
study
(26).
When
the
hospitalizations
were
researched,
the
most
common
causes
were
the
cardiovascular
diseases
again
(26).
In
another
study,
27%
of
all
mortality
was
due
to
the
cardiovascular
causes
in
the
moderate
and
severe
COPD
cases
(27).
Due
to
the
strong
atherosclerotic
natures
of
the
SCDs
and
COPD,
COPD
may
be
one
of
the
terminal
endpoints
of
the
SCDs
due
to
the
higher
prevalence
of
priapism,
cirrhosis,
leg
ulcers,
digital
clubbing,
CHD,
CRD,
and
stroke
in
the
COPD
group,
here.
Painful
crises
are
the
most
disabling
and
nearly
pathognomonic
symptoms
of
the
SCDs.
For
example,
only
11.9%
of
the
study
cases
(9.8%
versus
12.3%
in
the
COPD
and
other
groups,
respectively,
P>0.05)
have
not
had
any
painful
crisis
in
their
lives,
here.
Although
the
crises
may
not
be
life
threatening
directly
(28),
infections
are
the
most
common
precipitating
factors
of
them.
The
patients
are
immunocompromised
due
to
a
variety
of
reasons
including
a
functional
and
anatomic
asplenism,
chronic
endothelial
damage
induced
end-organ
failures,
a
permanent
inflammatory
process
all
over
the
body,
hospitalizations,
transfusions,
and
invasive
procedures.
Because
of
the
deep
immunodeficiency,
simple
infections
may
even
progress
to
sepsis
in
a
short
period
of
time.
Thus
multiorgan
failures
and
mortality
are
not
rare
during
acute
painful
crises
in
them.
Similarly,
RBC
supports
may
provide
adequate
tissue
oxygenation
and
immunity,
and
so
prevent
intractable
pain,
dissemination
of
infections
or
inflammations,
end-organ
failures,
and
mortality
during
surgical
operations,
major
depressions,
and
other
severe
clinical
conditions.
On
the
other
hand,
pain
is
the
result
of
a
yet
poorly
understood
interaction
between
the
hard
cells,
endothelial
cells,
white
blood
cells
(WBC),
and
platelets
(PLT).
The
adverse
effects
of
WBCs
and
PLTs
on
endothelium
are
of
particular
interest.
For
example,
leukocytosis
even
at
the
silent
period
was
an
independent
predictor
of
severity
of
the
SCDs
(29),
and
it
was
associated
with
an
increased
risk
of
stroke
(30).
On
the
other
hand,
leukocytosis
and
thrombocytosis
are
acute
phase
reactants
that
are
also
present
during
the
silent
periods
in
the
SCDs.
They
indicate
presence
of
a
permanent
inflammatory
process
initiating
at
birth.
The
continuous
inflammatory
process
alone
causes
an
additional
accelerated
atherosclerotic
process
and
a
relative
weight
loss
in
the
SCDs
(31).
Occlusions
of
vasculature
of
the
bone
marrow,
bone
infarctions,
releasing
of
inflammatory
mediators,
and
activation
of
afferent
nerves
may
take
a
role
in
the
pathophysiology
of
the
intractable
pains.
Because
of
the
severity
of
pain,
narcotic
analgesics
are
usually
required
to
control
them
(32),
but
according
to
our
practice,
RBC
supports
are
highly
effective
during
severe
crises
both
to
relieve
pain
and
to
prevent
sudden
deaths
secondary
to
the
multiorgan
failures
developed
on
chronic
inflammatory
background
of
the
SCDs.
Probably
parallel
to
severity
of
the
inflammatory
process,
an
asplenism
develops
with
decreased
antibody
production,
prevented
opsonization,
and
reticuloendothelial
dysfunction
due
to
the
repeated
infarctions
and
subsequent
fibrosis
in
early
years
of
life.
Similarly,
the
prevalence
of
autosplenectomy
was
51.6%
(221
cases)
among
the
patients
with
an
average
age
of
30.3
±
10.0
years
(range
5-59),
here.
Terminal
consequence
of
the
asplenism
is
an
increased
risk
of
infections,
particularly
due
to
Streptococcus
pneumoniae,
Haemophilus
influenzae,
and
Neisseria
meningitidis
like
encapsulated
bacteria.
Thus,
infections
particularly
the
pneumococcal
infections
are
common
in
early
childhood,
and
they
are
associated
with
a
high
mortality
rate.
The
causes
of
mortality
were
infections
in
56%
of
infants
in
a
previous
study
(29).
In
another
study,
the
peak
incidence
of
mortality
occured
between
1
to
3
years
of
age
in
children,
and
the
deaths
were
predominantly
caused
by
pneumococcal
sepsis
in
patients
less
than
20
years
of
age
(33).
According
to
our
nine-year
experiences
in
adults,
patients
even
who
appear
relatively
fit
are
susceptible
to
sepsis,
multiorgan
failures,
and
sudden
death
during
acute
painful
crises
due
to
the
deep
immunosuppression
in
them.
ACS
is
responsible
for
considerable
mortality,
particularly
during
the
childhood
in
the
SCDs
(34).
It
occurs
most
often
as
a
single
episode,
and
a
past
history
is
associated
with
an
early
mortality
(34).
Similarly,
all
of
14
cases
with
the
ACS
had
only
a
single
episode,
and
two
of
them
in
the
group
without
COPD
were
fatal
in
spite
of
rigorous
RBC,
ventilation,
and
antibiotic
supports
in
the
present
study.
The
remaining
12
patients
are
still
alive
without
a
recurrence
at
the
end
of
the
nine-year
follow-up
period.
ACS
is
the
most
common
between
the
ages
of
2
to
4
years,
and
its
incidence
decreases
with
age
(35).
Parallel
to
the
knowledge,
its
incidence
was
only
3.2%
among
the
patients
with
an
average
age
of
30.3
years,
here.
The
decreased
incidence
with
aging
may
be
due
to
a
high
mortality
during
the
first
episode
and/or
an
acquired
immunity
against
various
antigens
with
aging.
On
the
other
hand,
ACS
may
also
show
inborn
severity
of
the
SCDs.
For
example,
its
incidence
is
higher
in
severe
cases
such
as
cases
with
sickle
cell
anemia
(HbSS)
and
a
higher
WBC
count
(34,
35).
Probably,
ACS
is
a
complex
event,
and
the
terminology
of
'ACS'
does
not
indicate
a
definite
diagnosis
but
reflects
clinical
difficulty
of
defining
a
distinct
etiology
in
the
majority
of
such
episodes.
One
of
the
major
clinical
problems
lies
in
distinguishing
between
infection
and
infarction,
and
in
establishing
clinical
significance
of
fat
embolism.
For
example,
ACS
did
not
show
an
infectious
etiology
in
66%
of
episodes
in
the
above
studies
(34,
35).
Similarly,
12
of
27
episodes
of
ACS
had
evidence
of
fat
embolism
as
the
cause
in
another
study
(36).
But
according
to
our
experiences,
the
increased
metabolic
rate
during
severe
infections
may
terminate
with
the
ACS.
In
other
words,
ACS
may
be
characterized
by
the
hard
RBCs-induced
disseminated
endothelial
damage
and
fat
embolism
at
the
capillary
level.
A
preliminary
result
from
the
Multi-Institutional
Study
of
Hydroxyurea
in
the
SCDs
(37)
indicating
a
significant
reduction
of
ACS
episodes
with
hydroxyurea
suggests
that
a
substantial
number
of
episodes
are
secondary
to
the
endothelial
inflammation
and
edema
at
the
capillary
level.
Similarly,
we
strongly
recommend
hydroxyurea
therapy
for
all
patients
at
any
age
that
may
also
be
a
cause
of
the
low
incidence
of
ACS
among
our
follow-up
cases,
here.
Hydroxyurea
is
the
only
drug
that
was
approved
by
Food
and
Drug
Administration
for
the
treatment
of
SCDs
(13).
It
is
an
oral,
cheap,
safe,
and
highly
effective
drug
for
the
SCDs
that
blocks
cell
division
by
suppressing
formation
of
deoxyribonucleotides
which
are
building
blocks
of
DNA
(13).
Its
main
action
may
be
suppression
of
hyperproliferative
WBCs
and
PLTs
in
the
SCDs
(14).
Although
presence
of
a
continuous
damage
of
hard
RBCs
on
capillary
endothelium,
severity
of
the
destructive
process
is
probably
exaggerated
by
the
patients'
own
WBCs
and
PLTs
as
in
the
autoimmune
disorders
(14).
Similarly,
lower
WBC
counts
were
associated
with
lower
crises
rates,
and
if
a
tissue
infarct
occurs,
lower
WBC
counts
may
decrease
severity
of
pain
and
tissue
damage
(38).
According
to
our
experiences,
hydroxyurea
is
an
effective
drug
for
prevention
or
delay
of
terminal
consequences
of
the
SCDs
if
it
is
initiated
in
early
years
of
life,
but
it
may
be
difficult
due
to
the
excessive
fibrosis
around
the
capillary
walls
in
nearly
all
organs
later
in
life.
As
a
conclusion,
SCDs
are
chronic
catastrophic
processes
on
vascular
endothelium
particularly
at
the
capillary
level,
and
terminate
with
accelerated
atherosclerosis
induced
end-organ
failures
in
early
years
of
life.
RBC
supports
in
severe
clinical
conditions
probably
prolong
the
survival
of
patients.
1.
Eckel
RH,
Grundy
SM,
Zimmet
PZ.
The
metabolic
syndrome.
Lancet
2005;
365:
1415-1428.
2.
Helvaci
MR,
Kaya
H,
Sevinc
A,
Camci
C.
Body
weight
and
white
coat
hypertension.
Pak
J
Med
Sci
2009;
25:
6:
916-921.
3.
Helvaci
MR,
Gokce
C,
Davran
R,
Acipayam
C,
Akkucuk
S,
Ugur
M.
Tonsilectomy
in
sickle
cell
diseases.
Int
J
Clin
Exp
Med
2015;
8:
4586-4590.
4.
Helvaci
MR,
Gokce
C,
Davran
R,
Akkucuk
S,
Ugur
M,
Oruc
C.
Mortal
quintet
of
sickle
cell
diseases.
Int
J
Clin
Exp
Med
2015;
8:
11442-11448.
5.
Helvaci
MR,
Gokce
C,
Davarci
M,
Sahan
M,
Hakimoglu
S,
Coskun
M.
Chronic
endothelial
inflammation
and
priapism
in
sickle
cell
diseases.
Int
J
Clin
Exp
Med
2016;
(in
press).
6.
Global
strategy
for
the
diagnosis,
management
and
prevention
of
chronic
obstructive
pulmonary
disease
2010.
Global
initiative
for
chronic
obstructive
lung
disease
(GOLD).
7.
Castro
O,
Brambilla
DJ,
Thorington
B,
Reindorf
CA,
Scott
RB,
Gillette
P,
et
al.
The
acute
chest
syndrome
in
sickle
cell
disease:
incidence
and
risk
factors.
The
Cooperative
Study
of
Sickle
Cell
Disease.
Blood
1994;
84:
643-649.
8.
Fisher
MR,
Forfia
PR,
Chamera
E,
Housten-Harris
T,
Champion
HC,
Girgis
RE,
et
al.
Accuracy
of
Doppler
echocardiography
in
the
hemodynamic
assessment
of
pulmonary
hypertension.
Am
J
Respir
Crit
Care
Med
2009;
179:
615-621.
9.
Vandemergel
X,
Renneboog
B.
Prevalence,
aetiologies
and
significance
of
clubbing
in
a
department
of
general
internal
medicine.
Eur
J
Intern
Med
2008;
19:
325-329.
10.
Schamroth
L.
Personal
experience.
S
Afr
Med
J
1976;
50:
297-300.
11.
Mankad
VN,
Williams
JP,
Harpen
MD,
Manci
E,
Longenecker
G,
Moore
RB,
et
al.
Magnetic
resonance
imaging
of
bone
marrow
in
sickle
cell
disease:
clinical,
hematologic,
and
pathologic
correlations.
Blood
1990;
75:
274-283.
12.
Helvaci
MR,
Aydin
LY,
Aydin
Y.
Digital
clubbing
may
be
an
indicator
of
systemic
atherosclerosis
even
at
microvascular
level.
HealthMED
2012;
6:
3977-3981.
13.
Yawn
BP,
Buchanan
GR,
Afenyi-Annan
AN,
Ballas
SK,
Hassell
KL,
James
AH,
et
al.
Management
of
sickle
cell
disease:
summary
of
the
2014
evidence-based
report
by
expert
panel
members.
JAMA
2014;
312:
1033-1048.
14.
Helvaci
MR,
Aydin
Y,
Ayyildiz
O.
Hydroxyurea
may
prolong
survival
of
sickle
cell
patients
by
decreasing
frequency
of
painful
crises.
HealthMED
2013;
7:
2327-2332.
15.
Platt
OS,
Brambilla
DJ,
Rosse
WF,
Milner
PF,
Castro
O,
Steinberg
MH,
et
al.
Mortality
in
sickle
cell
disease.
Life
expectancy
and
risk
factors
for
early
death.
N
Engl
J
Med
1994;
330:
1639-1644.
16.
Charache
S,
Scott
JC,
Charache
P.
''Acute
chest
syndrome''
in
adults
with
sickle
cell
anemia.
Microbiology,
treatment,
and
prevention.
Arch
Intern
Med
1979;
139:
67-69.
17.
Davies
SC,
Luce
PJ,
Win
AA,
Riordan
JF,
Brozovic
M.
Acute
chest
syndrome
in
sickle-cell
disease.
Lancet
1984;
1:
36-38.
18.
Mathers
CD,
Sadana
R,
Salomon
JA,
Murray
CJ,
Lopez
AD.
Healthy
life
expectancy
in
191
countries,
1999.
Lancet
2001;
357:
1685-1691.
19.
Helvaci
MR,
Ayyildiz
O,
Gundogdu
M.
Gender
differences
in
severity
of
sickle
cell
diseases
in
non-smokers.
Pak
J
Med
Sci
2013;
29:
1050-1054.
20.
Rennard
SI,
Drummond
MB.
Early
chronic
obstructive
pulmonary
disease:
definition,
assessment,
and
prevention.
Lancet
2015;
385:
1778-1788.
21.
Schoepf
D,
Heun
R.
Alcohol
dependence
and
physical
comorbidity:
Increased
prevalence
but
reduced
relevance
of
individual
comorbidities
for
hospital-based
mortality
during
a
12.5-year
observation
period
in
general
hospital
admissions
in
urban
North-West
England.
Eur
Psychiatry
2015;
30:
459-468.
22.
Singh
G,
Zhang
W,
Kuo
YF,
Sharma
G.
Association
of
Psychological
Disorders
With
30-Day
Readmission
Rates
in
Patients
With
COPD.
Chest
2016;
149:
905-915.
23.
Danesh
J,
Collins
R,
Appleby
P,
Peto
R.
Association
of
fibrinogen,
C-reactive
protein,
albumin,
or
leukocyte
count
with
coronary
heart
disease:
meta-analyses
of
prospective
studies.
JAMA
1998;
279:
1477-1482.
24.
Mannino
DM,
Watt
G,
Hole
D,
Gillis
C,
Hart
C,
McConnachie
A,
et
al.
The
natural
history
of
chronic
obstructive
pulmonary
disease.
Eur
Respir
J
2006;
27:
627-643.
25.
Mapel
DW,
Hurley
JS,
Frost
FJ,
Petersen
HV,
Picchi
MA,
Coultas
DB.
Health
care
utilization
in
chronic
obstructive
pulmonary
disease.
A
case-control
study
in
a
health
maintenance
organization.
Arch
Intern
Med
2000;
160:
2653-2658.
26.
Anthonisen
NR,
Connett
JE,
Enright
PL,
Manfreda
J;
Lung
Health
Study
Research
Group.
Hospitalizations
and
mortality
in
the
Lung
Health
Study.
Am
J
Respir
Crit
Care
Med
2002;
166:
333-339.
27.
McGarvey
LP,
John
M,
Anderson
JA,
Zvarich
M,
Wise
RA;
TORCH
Clinical
Endpoint
Committee.
Ascertainment
of
cause-specific
mortality
in
COPD:
operations
of
the
TORCH
Clinical
Endpoint
Committee.
Thorax
2007;
62:
411-415.
28.
Parfrey
NA,
Moore
W,
Hutchins
GM.
Is
pain
crisis
a
cause
of
death
in
sickle
cell
disease?
Am
J
Clin
Pathol
1985;
84:
209-212.
29.
Miller
ST,
Sleeper
LA,
Pegelow
CH,
Enos
LE,
Wang
WC,
Weiner
SJ,
et
al.
Prediction
of
adverse
outcomes
in
children
with
sickle
cell
disease.
N
Engl
J
Med
2000;
342:
83-89.
30.
Balkaran
B,
Char
G,
Morris
JS,
Thomas
PW,
Serjeant
BE,
Serjeant
GR.
Stroke
in
a
cohort
of
patients
with
homozygous
sickle
cell
disease.
J
Pediatr
1992;
120:
360-366.
31.
Helvaci
MR,
Kaya
H.
Effect
of
sickle
cell
diseases
on
height
and
weight.
Pak
J
Med
Sci
2011;
27:
361-364.
32.
Cole
TB,
Sprinkle
RH,
Smith
SJ,
Buchanan
GR.
Intravenous
narcotic
therapy
for
children
with
severe
sickle
cell
pain
crisis.
Am
J
Dis
Child
1986;
140:
1255-1259.
33.
Leikin
SL,
Gallagher
D,
Kinney
TR,
Sloane
D,
Klug
P,
Rida
W.
Mortality
in
children
and
adolescents
with
sickle
cell
disease.
Cooperative
Study
of
Sickle
Cell
Disease.
Pediatrics
1989;
84:
500-508.
34.
Poncz
M,
Kane
E,
Gill
FM.
Acute
chest
syndrome
in
sickle
cell
disease:
etiology
and
clinical
correlates.
J
Pediatr
1985;
107:
861-866.
35.
Sprinkle
RH,
Cole
T,
Smith
S,
Buchanan
GR.
Acute
chest
syndrome
in
children
with
sickle
cell
disease.
A
retrospective
analysis
of
100
hospitalized
cases.
Am
J
Pediatr
Hematol
Oncol
1986;
8:
105-110.
36.
Vichinsky
E,
Williams
R,
Das
M,
Earles
AN,
Lewis
N,
Adler
A,
et
al.
Pulmonary
fat
embolism:
a
distinct
cause
of
severe
acute
chest
syndrome
in
sickle
cell
anemia.
Blood
1994;
83:
3107-3112.
37.
Charache
S,
Terrin
ML,
Moore
RD,
Dover
GJ,
Barton
FB,
Eckert
SV,
et
al.
Effect
of
hydroxyurea
on
the
frequency
of
painful
crises
in
sickle
cell
anemia.
Investigators
of
the
Multicenter
Study
of
Hydroxyurea
in
Sickle
Cell
Anemia.
N
Engl
J
Med
1995;
332:
1317-1322.
38.
Charache
S.
Mechanism
of
action
of
hydroxyurea
in
the
management
of
sickle
cell
anemia
in
adults.
Semin
Hematol
1997;
34:
15-21.
|

