|
Is Sleep Apnea Worse
in the Winter?
Mustafa Yilmaz
(1)
Nigar Yilmaz (2)
Dilek Aslan Ozturk (1)
Ercan Baldemir (3)
Gülser Karadaban Emir (1)
Murat Sahan (4)
Yasemin Unal (1)
Ayse Sözen (1)
Gülnihal Kutlu (1)
(1) Mugla Sitki Kocman University, Faculty
of Medicine, Department of Neurology, Mugla,
Turkey
(2) Mugla Sitki Kocman University, Faculty of
Medicine, Department of Biochemistry, Mugla,
Turkey
(3) Mugla Sitki Kocman University, Faculty of
Medicine, Department of Biostatistics, Mugla,
Turkey
(4) Mugla Sitki Kocman University, Faculty of
Medicine, Department of Otolaryngology, Mugla,
Turkey
Correspondence:
Mustafa Yilmaz
Mugla Sitki Kocman University,
Faculty of Medicine,
Department of Neurology, Mugla, Turkey
Email: mustafayilmaz@mu.edu.tr
|
Abstract
Objectives: The
present study aimed to investigate the
seasonal variability of AHI values among
patients with sleep apnea.
Patients and Methods:
In order to conduct the retrospective
study, we accepted 304 patients (223 male
and 81 female) between May 2014 to May
2015 into our study at Mugla Sitki Koçman
University Medical faculty of sleep disorders
clinic. Patients were divided into four
groups according to the timing of the
PSG: winter, spring, summer, and autumn.
Results: We
reviewed the records of patients, including
their PSGs, and found that their AHI values
were comparable across seasons. The average
AHI value for males was 34.95±
29.95 and 21.88±2.76 for females;
we observed no significant statistical
difference among the four groups (both
males and females) in terms of AHI.
Conclusion:
Although patient complaints increased
due to exacerbation of diseases such as
asthma and allergic rhinitis in the winter,
this study did not reflect a significant
change in AHI values. Therefore, PSG examinations
do not need to be repeated in different
seasons.
Keywords: sleep
apnea, seasonal variation
|
Obstructive sleep apnea syndrome (OSAS) is
the most widely suffered sleep disorder after
insomnia and is increasingly common due to the
prevalence of obesity. It describes a situation
in which breathing is briefly and repeatedly
interrupted for at least ten seconds, resulting
in a reduction of blood oxygen levels [1,2].
This occurs when the muscles in the back of
the throat fail to keep the airway open, despite
efforts to breathe [3]. Obstructive sleep apnea
can be caused by many factors, such as adenotonsillar
hypertrophy, allergies and viral respiratory
infections [4]. Furthermore, the prevalence
of sleep apnea increases due to allergic rhinitis
and asthma [5]. As the seasons change, sleep
patterns change, and allergic rhinitis and asthma
are more common in the spring [6].
Polysomnography (PSG), a type of sleep study,
is a multi-parametric test used to examine eye
movements, muscle-brain-heart activity, oxygen
saturation, position and nasal flow during sleep
[7]. The apnea-hypopnea index (AHI) is the most
common means to measure sleep apnea, recording
the number of apneas or hypopneas per hour of
sleep. A person's AHI is classified as mild-moderate
or severe [8]. In this study, we aimed to determine
and compare patients' AHI values, based on PSG
tests, over four seasons, independent of age,
sex, body mass index (BMI) and chronic obstructive
pulmonary disease (COPD) status.
Study Population
In order to conduct the retrospective examination,
we accepted 304 (223 male and 81 female) patients
between May 2014 to May 2015 into our study
at Mugla S?tk? Kocman University Medical faculty
of sleep disorders clinic. We reviewed these
patients' records, including PSG results, and
participants were divided into four groups according
to the timing of the PSG: winter, spring, summer,
and autumn. We ensured that the groups were
similar in regards to age, sex and body mass
index (BMI). In our study, the exclusion criteria
included patients with chronic obstructive pulmonary
disease (COPD). The patients' AHI values were
compared across seasons. The study protocol
has been approved by the Ethics Committee of
the University.
Polysomnography
All patients underwent technician-attended whole-night
polysomnography with EMBLA S4500 equipment in
the sleep laboratory of our hospital. Polysomnography
recordings were obtained between 10:00 pm and
06:00 am (8 hours). Six-channel electroencephalography
(two each: occipital, central, and frontal),
right and left electrooculography, electrocardiography,
chin and right and left tibialis muscle electromyography,
oronasal pressure, thoracal and abdominal respiratory
efforts, pulse oximetry, position, and snoring
sound were recorded. The polysomnographic data
were scored manually by a certified and experienced
physician in accordance with the American Academy
of Sleep Medicine Manual for Scoring Sleep and
Associated Events, Version 2 [9]. Apnea was
scored when there was a drop in the peak signal
excursion by > 90% of pre-event baseline
and the duration of the > 90% drop
in sensor signal was > 10 s. Hypopnea
was scored when the peak signal excursions dropped
by > 30% of pre-event baseline for
> 10 s in association with either
> 3% arterial oxygen desaturation
or an arousal. The AHI was calculated by dividing
the number of apnea/hypopnea events by the number
of hours of sleep. Oxygen desaturation index
3 (ODI3) was calculated by dividing the number
of 3% drops in oxygen saturation by the number
of hours of sleep. The minimum oxygen saturation
was noted.
Statistical Analysis
The data were processed and analyzed using SPSS-18
for Windows, Fisher's Exact Test, Pearson Correlations,
and Pearson's Chi-Square test; logistic regression
was used for the comparison of categorical and
scale variables, where p<0.05 was considered
to be statistically significant. Among the groups,
variables that were found to be statistically
significant and variables that are not conceptually
compatible were added to the logistic regression
model.
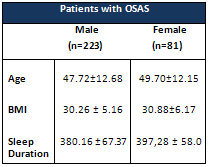
A
total
population
of
304
patients
(223
male
and
81
female)
with
mean
ages
of
47.72
±
12.68
in
males
and
49.70±12.15
in
females
was
studied.
Mean
BMI
was
30.26
±
5.16
in
males
and
30.88±6.17
in
females
(Table
1).
Mean
age,
sex
and
BMI
did
not
differ
among
the
four
groups
Total
sleep
duration
was
380.16
±
67.37
in
males
and
397,28
±
58.0
in
females
(p=0.0501).
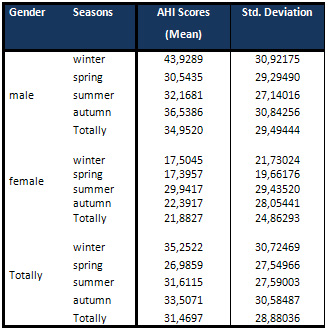
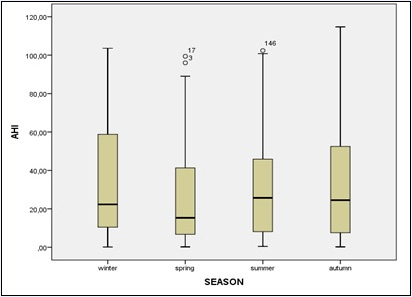
We
found
that
one
season
did
not
differ
from
the
others,
although
patient
AHIs
were
lowest
in
the
spring
and
highest
in
the
winter
(Table
2,
Figure
1).
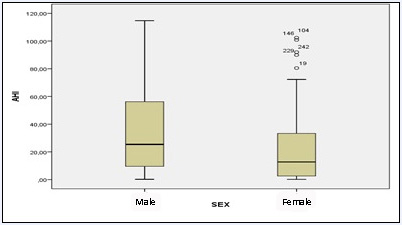
AHIs
were
highest
in
male
patients
with
sleep
apnea
than
female
patients
with
sleep
apnea
(Figure
2).
Table
1
Table
2
Figure
1
Figure
2
In
the
present
study,
we
have
shown
that
patients
with
OSAS
are
not
affected
by
the
seasons.
Although
not
statistically
significant,
we
found
that
AHIs
were
lowest
in
the
spring
and
highest
in
the
winter.
This
runs
contrary
to
some
evidence
in
the
literature
indicating
that
patients
with
OSAS
are
affected
by
the
seasons
[10-12],
although
other
sources
have
shown
that
patients
with
OSAS
are
not
affected
by
the
seasons.
For
instance,
Dempsey
demonstrated
that
airway
infections
and
weather
could
have
an
effect
on
sleep
apnea,
but
that
the
changes
across
the
seasons
had
little
effect
on
AHI
values
[13],
while
Cassol
reported
that
more
sleep
disorder
breathing
events
occurred
in
winter
than
in
other
seasons.
They
observed
that
people
stopped
breathing
more
than
30
times
an
hour
in
the
colder
months
[14].
However,
these
differences
may
be
associated
with
geographic
location.
The
fact
that
many
of
these
researchers
are
from
Brazil
and
the
USA
could
have
affected
their
results.
Our
studies
were
conducted
in
Mu?la,
but
the
same
study
may
yield
different
results
in
another
province.
Although
inflammation
and
oxidative
stress
are
important
in
the
pathophysiology
of
OSAS,
the
relationship
between
inflammation
remains
poorly
understood.
Many
factors
affect
the
airway
of
a
person
with
obstructive
sleep
apnea
syndrome.
For
example,
atmosphere
and
sun
cycles
can
play
a
significant
role
in
sleep
quality
[15].
Changes
in
seasons
also
affect
the
issue
in
different
ways.
Additionally,
Kalra
et
al.
found
a
high
prevalence
of
snoring
in
young
women
with
atopy
and
a
significant
association
with
asthma
[11].
Similar
studies
have
also
shown
that
asthma
is
a
frequent
comorbidity
in
patients
with
OSAS
(12).
Similarly,
Kalpaklioglu
et
al.
reported
that
allergic
rhinitis
is
a
risk
factor
for
a
high
apnea-hypopnea
index,
and
after
rhinitis
treatment,
a
patient's
AHI
and
Epworth
Sleepiness
Scale
(ESS)
scores
will
be
reduced.
They
observed
the
most
significant
difference
in
a
group
treated
with
nasal
steroid
+
antihistamine
compared
to
the
control
group
[16].
Several
types
of
patients
were
included
in
this
study,
although
ensuring
similarity
of
age,
sex
and
BMI
may
be
considered
one
of
its
weaknesses.
Here,
using
the
same
patients'
PSG
evaluation
in
different
seasons
would
have
been
better.
However,
this
was
not
attempted,
as
it
was
not
covered
by
the
study
approval.
In
addition,
patients
who
do
not
suffer
from
asthma
and
allergic
rhinitis
may
be
enrolled
as
a
not
statistical
difference.
At
that
time
it
could
not
be
a
generalization.
Allergic
rhinitis
is
a
common
disease
in
childhood
[17],
so
if
the
study
had
been
done
in
this
age
group,
the
AHI
index
would
have
been
higher
in
the
winter.
Furthermore,
we
did
not
evaluate
the
complaints
of
the
patients
in
this
study.
If
we
had
evaluated
their
complaints
by
the
subjective
ESS
test,
results
may
have
been
more
meaningful
or
useful.
In
the
light
of
the
data
obtained
from
this
study,
we
found
that
seasons
did
not
contribute
to
significant
changes
in
AHI
values.
Therefore,
examination
of
PSG
does
not
need
to
be
repeated
in
different
seasons,
especially
among
the
elderly
and
those
without
asthma
and
allergic
rhinitis.
1.Chokroverty
S.
Clinical
Companion
to
Sleep
Disorders
Medicine.
2nd
ed.
Oxford,
England:
Butterworth-Heinemann
Publishers;
2000
2.Crummy
F,
Piper
AJ,
Naughton
MT.
Obesity
and
the
lung:
Obesity
and
sleep
disordered
breathing.Thorax.
2008;63:738-46
3.Young
T,
Finn
L,
Kim
H.
Nasal
obstruction
as
a
risk
factor
for
sleep
disordered
breathing.
J
Allergy
Clin
Immunol.
1997;99:757-762
4.Kramer
MF,
de
la
Chaux
R,
Fintelmann
R,
Rasp
G.
NARES:
a
risk
factor
for
obstructive
sleep
apnea?
Am
J
Otolaryngol.
2004;25:173-177
5.Staevska
MT,
Mandajieva
MA,
Dimitrov
VD.
Rhinitis
and
sleep
apnea.
Curr
Allergy
Asthma
Rep.
2004;4(3):193-9
6.Skoner
DP.
Allergic
rhinitis:
Definition,
epidemiology,
pathophysiology,
detection,
and
diagnosis.
J
Allergy
Clin
Immunol.
2001;
108:2-8.
7.The
American
Academy
of
Sleep
Medicine
Inter-scorer
Reliability
Program:
Sleep
Stage
Scoring,
Richard
S.
Rosenburg,
Steven
van
Hout,
J
Clin
Sleep
Med.
2013;
9(1):
81-87
8.Olson
EJ,
Moore
WR,
Morgenthaler
TI,
Gay
PC,
Staats
BA.
Obstructive
sleep
apnoea
hypopnoea
syndrome.
Mayo
Clin
Proc.
2003;78:1545-52
9.Berry
RB,
Brooks
R,
Gamaldo
CE,
Harding
SM,
Lloyd
RM,
Marcus
CL,
Vaughn
BV,
for
the
American
Academy
of
Sleep
Medicine
(2014)
The
AASM
Manual
for
the
Scoring
of
Sleep
and
Associated
Events:
Rules,
Terminology
and
Technical
Specifications,
Version
2.0.3.
Accessed
1
July
2015
10.
Kalra
M,
Biagini
J,
Bernstein
D,
Stanforth
S,
Burkle
J,
Cohen
A,
LeMasters
G,
Ann
Allergy
Asthma
Immunol.
Effect
of
asthma
on
the
risk
of
obstructive
sleep
apnea
syndrome
in
atopic
women
2006
Aug;
97(2):
231-235.
11.
Larsson
LG,
Lindberg
A,
Franklin
KA,
et
al.
Symptoms
related
to
obstructive
sleep
apnoea
are
common
in
subjects
with
asthma,
chronic
bronchitis
and
rhinitis
in
a
general
population.
Respir
Med.
2001;95:423-429.
12.Dempsey
JA,
Veasey
SC,
Morgan
BJ,
O'Donnell
CP.
Pathophysiology
of
sleep
apnea.
Physiol
Rev.
2010;90(1):47-112.
13.Cassol
CM,
Martinez
D,
da
Silva
FA,
Fischer
MK,
Lenz
Mdo
C,
Bós
ÂJ.
Is
sleep
apnea
a
winter
disease?:
meteorologic
and
sleep
laboratory
evidence
collected
over
1
decade.
Chest.
2012;142(6):1499-507
14.Kent
BD,
Ryan
S,
McNicholas
WT
(2011)
Obstructive
sleep
apnea
and
inflammation:
relationship
to
cardiovascular
co-morbidity.
Respir
Physiol
Neurobiol
178(3):475-81.
15.Hatipoglu
U,
Rubinstein
I.
Inflammation
and
Obstructive
Sleep
Apnea
Syndrome
Pathogenesis:
A
Working
Hypothesis
,
Respiration
2003;70:665-671
16.Kalpaklio?lu
AF,
Kavut
AB,
Ekici
M.
Allergic
and
nonallergic
rhinitis:
the
threat
for
obstructive
sleep
apnea.
Ann
Allergy
Asthma
Immunol.
2009;103(1):20-5.
17.Wenzel
S.
Severe
asthma
in
adults.
Am
J
Respir
Crit
Care
Med.
2005;172:149-60
|

