|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................
|
Original
Contribution/Clinical Investigation
|
|

|
<-- Middle East / South Asia Regional
-->
Barriers,
Challenges and Way Forward for Implementation
of Person Centered Care Model of Patient and
Physician Consultation: A Survey of Patients’
Perspective from Eastern Mediterranean Countries
[pdf version]
Waris Qidwai, Kashmira Nanji, Tawfik A M Khoja,
Salman Rawaf, Nabil Yasin Al Kurashi, Faisal
Alnasir, Mohammed Ali Al Shafaee, Mariam Al
Shetti, Muntazar Bashir,
Nagwa Eid Sobhy Saad, Sanaa Alkaisi, Wafa Halasa,
Huda Al-Duwaisan, Amal Al-Ali
<-- Jordan -->
Passive
Smoking and Pregnancy Outcome
[pdf version]
Tarek Athamneh, Sultan Qudah, Mahmoud Mashaqbeh,
Sumaya Ali Njadat,
Mohammed Khderat
|
|
........................................................ |
Medicine and Society
........................................................
Education and training
........................................................
Continuing Professional Development
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| April/May 2015
- Volume 13 Issue 3 |
|
Passive
Smoking and Pregnancy Outcome
Tarek Athamneh
(1)
Sultan Qudah (1)
Mahmoud Mashaqbeh
(1)
Sumaya Ali Njadat
(2)
Mohammed Khderat (3)
(1) Specialist, Department of Obstetrics and
Gynecology
Royal Medical Services, Jordan
(2) B.Sc, Department of Pharmacy
Royal Medical Services, Jordan
(3) Specialist, Department of Medicine
Royal Medical Services, Jordan
Correspondence:
Sultan Qudah
Specialist, Department of Obstetrics and Gynecology
Royal Medical Services, Jordan
Email: sultanqudah@yahoo.com
|
Abstract
Objective:
To evaluate the association between
passive smoking and adverse reproductive
effects or pregnancy outcomes among Jordanian
pregnant women.
Material and Methods: This was
a retrospective study which was conducted
at Prince Rashid Ben Alhasan hospital
between 2011 and 2013. Total samples of
4125 newborns were included in the study.
The demographic characteristics of these
newborns included: gestational age, gender,
birth weight, congenital anomaly, mode
of delivery and admission to NICU. Maternal
characteristics of Jordanian women according
to passive smoking included: age, parity,
weight, and income.
Results: Pregnancy outcome for
Jordanian women according to passive smoking
status indicated that passive smoking
is related with stillbirth with an incidence
of 1.0%, low birth weight in 11.9%, pre-term
delivery in 12.5%, congenital anomaly
in 1.6%, caesarean delivery in 23.7% and
need for admission in NICU in 35.4%. The
result indicated that exposure to passive
smoking during pregnancy had adverse effects
on low birth weight, admission to NICU,
and need for antibiotic significantly,
p- value <.0005.
Conclusion: Exposure to passive
smoking during pregnancy had adverse effects
on pregnancy outcome. Adverse reproductive
effects are serious and costly health
problems that have a huge impact on morbidity
and mortality rate in all societies.
Key words: passive smoking, pregnancy,
pregnancy outcome.
|
Cigarette smoking either as active or passive
smoking is a major public health concern and
considered as the greatest preventable cause
of illness and premature death in our society
(1). Worldwide, it is estimated that the number
of women who are smokers will be trebled over
the next generation (2). In developed countries
such as the United States, the prevalence of
cigarette smoking among pregnant women declined
from 25 % in 1980 to reach 12 % in 2000, while
the reverse is occuring in developing countries(3).
Unfortunately, lack of studies were found in
Jordan to investigate cigarette smoking behaviors
during pregnancy.
Indeed, there is growing and greater evidence
surrounding potential adverse reproductive health
effects and pregnancy outcomes resulting from
exposure to either passive or active smoking(4).
However a lot of studies demonstrated the adverse
effect of active cigarette smoking on pregnancy
outcome including low birth weight, pre-term
birth, still birth, spontaneous abortion and
fetal growth restriction(5,6,7,8) at the same
time few studies have found an association between
active smoking and congenital malformation(9).
In fact, a few studies investigated the associations
between passive smoking and adverse reproductive
effects or pregnancy outcomes. Passive smoking
is identified either as main stream or side
stream. Main stream smoking is defined as tobacco
smoke generated during puff-drawing in the burning
cone of a tobacco product, which then travels
through the unburnt tobacco and is inhaled directly
by the smoker(10); while side stream smoking
is defined as a combination of smoke emitted
into the air during the burning of a tobacco
product between puffs, smoke escaping into the
surrounding air during puffs and smoke components
that diffuse through cigarette paper (10).
The majority of passive smoking is in the form
of side stream smoking generated from the burning
end of a lighted cigarette, whereas the remainder
is composed of main stream smoking exhaled by
individuals actively smoking.
In all, women who have exposure to cigarette
smoking were posed a greater danger not only
to their own reproductive health, but also to
their unborn child if they are exposed during
pregnancy. However, cigarette smoke constituents,
including mutagenic, neurotoxic, and fetotoxic
agents can pass through the placenta and are
detected in the urine of newborns (11).
Indeed, adverse reproductive effects are serious
and costly health problems that have huge impact
on morbidity and mortality rate in all societies.
However, few recent studies have investigated
the association between passive smoking and
adverse reproductive effects or pregnancy outcomes.
Globally, little is known about the associations
between passive smoking and reproductive effects
or pregnancy outcomes. In Jordan lack of studies
have investigated this health problem too, so
the purpose of this study is to evaluate the
association between passive smoking and adverse
reproductive effects or pregnancy outcomes among
Jordanian pregnant women.
This
was
a
retrospective
study
which
was
conducted
at
Prince
Rashid
Ben
Alhasan
hospital
between
2011
and
2013.
Total
samples
of
4125
newborns
were
included
in
the
study
with
the
majority
aged
between
21-
29
weeks;
newborn
were
categorized
to
five
age
groups
which
ranged
from
less
than
20
weeks
to
more
than
40
weeks.
The
demographic
characteristics
of
these
newborns
included:
gestational
age,
gender,
birth
weight,
congenital
anomaly,
mode
of
delivery
and
admission
to
NICU.
Maternal
characteristics
of
Jordanian
women
according
to
passive
smoking
included:
age,
parity,
Body
Mass
Index,
resident
area,
income,
occupation,
and
education
as
shown
in
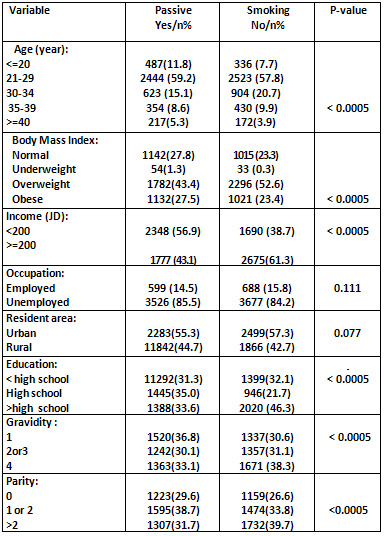
Table
1.
Table
1:
Socio-demographic
and
maternal
characteristics
of
Jordanian
women
according
to
passive
smoking
status
Analysis
of
the
distribution
of
participants
according
to
gender
revealed
that
male
newborns
represented
49.6%
of
the
participants,
while
female
newborns
represented
50.4%.
Pregnancy
outcome
for
Jordanian
women
according
to
passive
smoking
status
indicated
that
passive
smoking
is
related
with
stillbirth
with
an
incidence
of
1.0%,
low
birth
weight
in
11.9%,
pre-term
delivery
in
12.5%,
congenital
anomaly
in
1.6%,
caesarean
delivery
in
23.7%
and
need
for
admission
in
NICU
in
35.4%.
Pregnancy
and
outcome
for
Jordanian
women
according
to
passive
smoking
status
indicated
that
passive
smoking
is
related
with
Still
birth,
Low
birth
weight,
Pre-term
delivery,
Need
of
an
infant
for
treatment
by
antibiotic,
Need
for
admission
in
NICU,
and
Caesarean
significantly
as
shown
in
Table
2.
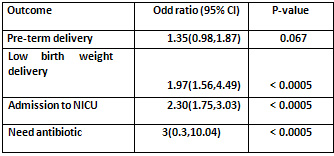
Adjusted
for
age,
weight,
height,
job,
residency,
education,
mother
blood
group,
gravidity,
parity,
history
of
abortion,
history
of
chronic
pain,
family
history
of
low
birth
weight,
history
of
prematurity,
onset
of
antenatal
visit,
plan
for
pregnancy,
happiness,
drug
pregnancy,
use
of
medication
during
pregnancy,
gum
bleeding
during
pregnancy,
coffee
drinking,
urinary
tract
infection,
inter
pregnancy
interval,
and
gender,
the
result
indicated
that
exposure
to
passive
smoking
during
pregnancy
had
adverse
effects
on
low
birth
weight,
admission
to
NICU,
and
need
antibiotic
significantly
p-
value
<.0005
as
shown
in
Table
3.
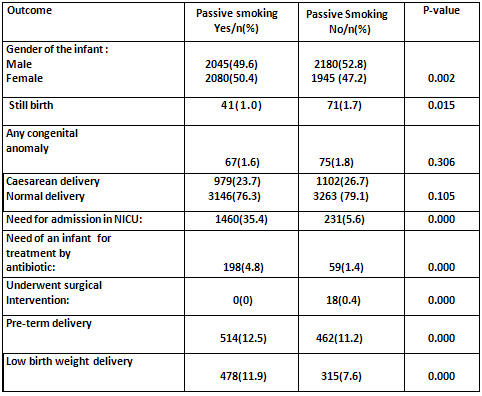
Table
2:
Pregnancy
and
outcome
for
Jordanian
women
according
to
passive
smoking
status
Table
3:
Multivariate
analysis
of
the
difference
in
adverse
pregnancy
outcome
between
passive
smokers
and
non
smoker
Cigarette
smoking
contains
more
than
2.500
chemicals;
these
chemicals
are
harmful
to
the
developing
baby(12).
Both
nicotine
and
carbon
monoxide
are
believed
to
play
a
role
in
causing
adverse
pregnancy
outcomes.
Most
recent
studies
reported
that
carbon
monoxide
and
dioxide
decrease
availability
of
oxygen
which
are
the
primary
substance
responsible
for
fetal
adverse
effect(13).
However,
exposure
to
cigarette
smoking
during
pregnancy
via
active
or
passive
routes
is
believed
to
be
a
strong
risk
factor
for
pre-term
birth
and
low
birth
weight.
There
is
growing
concern
surrounding
potential
adverse
reproductive
health
effects
and
pregnancy
outcomes
resulting
from
passive
smoking
(14).
Passive
smoking
for
pregnant
women
can
possess
significant
health
risks
to
the
mother,
infant,
and
it
is
associated
with
numerous
avoidable
health
risks
to
infant
such
as
risk
for
low
birth
weight
is
doubled,
small
for
gestational
age,
and
prenatal
death.
Indeed,
a
recent
study
conducted
in
Canada
examined
the
adverse
effects
of
cigarette
smoking
among
225
women
undergoing
IVF
in
Canadian
reproductive
clinic
between
2003
and
2004.
The
finding
showed
significant
lower
implantation
rates
and
pregnancy
rates
were
found
among
both
active
and
passive
smokers
compared
with
non-smokers.
However,
passive
smoking
among
the
women
in
the
study
was
measured
only
by
the
self-reported(14).
Furthermore,
a
study
conducted
by
Meeker
and
colleagues
(2006),
used
multivariate
design
for
921
women
undergoing
assisted
reproductive
technologies
to
assess
relationship
between
maternal
exposure
to
second
hand
tobacco
smoke
and
adverse
pregnancy
outcomes.
The
result
indicated
that
the
infant
in
utero
of
female
exposure
to
second
hand
tobacco
smoke
may
increase
risk
for
spontaneous
abortion(15).
In
Asia,
one
recent
study
examined
the
association
between
maternal
smoking
and
pregnancy
loss
among
526
non-smoking
Chinese
females.
However,
the
result
indicated
increased
odds
of
early
pregnancy
loss
among
women
with
husbands
who
smoked
more
than
20
cigarettes
per
day(16).
This
study
emphasized
on
the
result
obtained
by
another
study
conducted
in
California
among
3000
pregnant
women
with
exposure
to
second
hand
tobacco
smoke.
However,
the
finding
showed
an
increased
risk
of
spontaneous
abortion
among
mothers
who
were
exposed
to
tobacco
smoke
for
one
hour
or
more
per
day(17).
Another
adverse
effect
of
passive
cigarette
smoking
was
reported
by
Hunke
and
their
colleagues
in
(1999);
they
conducted
a
study
to
evaluate
the
effect
of
environmental
tobacco
smoke
on
the
risk
of
pre-term
delivery
and
small
for
gestational
age
in
central
Poland
with
a
randomly
selected
population
of
1751
women
who
gave
birth
between
June
1996
and
May
1997
and
based
on
a
structured
interview.
The
result
showed
that
95
of
the
passive
smoking
women
delivered
before
37
weeks
of
pregnancy
and
111
passive
smoking
mothers
delivered
babies
with
birth
weight
below
the
10
%
of
the
standard
curves
for
central
Poland(18).
The
questions
that
emerged
in
the
previous
studies
is
whether
these
associations
differ
by
maternal
age.
However,
Ahluwalia
et
al.
(1999)
examined
the
association
between
exposure
to
environmental
tobacco
smoke
during
pregnancy
and
birth
weight,
prematurely
and
small
for
gestational
age
and
to
determine
whether
these
associations
differed
by
maternal
age.
They
found
that
the
mean
adjusted
birth
weight
among
infants
of
non-smoking
mothers
age
30
years
or
older
was
90
gm
less
than
infants
not
exposed;
similarly,
were
the
risk
of
low
birth
weight
(odds
ratio
=
2.42,
95%
confidence
interval
1.51-3.87)
and
pre-term
-delivery
(odds
ratio
=
1.88,
95%
confidence
interval
1.22-2.88).
These
finding
indicated
that
the
association
between
environmental
tobacco
smoke
exposure
and
adverse
pregnancy
outcomes
appears
to
be
modified
by
maternal
age(19).
On
the
other
hand,
a
study
was
conducted
among
mothers
at
delivery
and
neonates
in
Inchon,
which
included
81
mothers
exposed
to
tobacco
smoke,
to
examine
the
association
between
environmental
pollutants
with
smoking
and
utero
developmental
damage.
The
result
indicated
that
oxidative
damage
in
newborns
is
affected
by
mothers
exposure
to
environmental
tobacco
smoke,
and
the
findings
strongly
show
the
need
for
smoking
cessation
among
household
members
during
pregnancy(20).
One
random
sample
study
found
in
our
literature
used
a
cross-sectional
design
in
stratified
random
sample
study,
in
the
city
of
Espooin
in
1991.
The
researcher
examined
pregnancy
outcomes
among
nonsmoking
pregnant
women
exposed
to
environmental
tobacco.
The
result
indicated
there
was
a
trend
of
risk
of
low
birth
weight
and
pre-term
delivery
related
to
maternal
exposure
to
environmental
tobacco
smoke(21).
1-
Ministry
of
Health
(MOH).
Annual
statistical
report
Jordan,
[Online]
[Accessed
2006
November).
Available
from
URL
www.moh.gov.jo.
Last
accessed
1
November
2006.
2-
Surgeon
general
report,
women
and
smoking.
(2001).
Retrieved
from:
http://www.cdc.goy,/to
baceo/sgr.
3-
Canttingius
S.
(2004).
The
epidemiology
of
smoking
during
pregnancy:
smoking
prevalence,
maternal
characteristics,
and
pregnancy
outcomes,
nicotine
and
tobacco
research;
6
:(2):125-140.
4-
Wu
T.
et
al
(2007).
Passive
smoking,
metabolic
gene
polymorphisms,
and
infant
birth
weight
in
prospective
cohort
study
of
Chinese,
American
journal
of
epidemiology,
166:
(3),313-327.
5-
Mathews
Y.
(2001).
Smoking
during
pregnancy
in
the
1990s.
Natl
Vital
Stat
Rep.
49:1-14.
6-
Kelly
Y.
et
al.
(1995).
Maternal
asthma,
premature
birth
and
the
risk
of
respiratory
morbidity
in
schoolchildren
in
Merseyside.
Thorax:
50:525-530.
7-
Hogberg
L.
&
Canttingius
S.
(2007).
The
influence
of
maternal'
smoking
habit
on
the
risk
of
subsequence
of
still
birth,
is
there
a
causal
relation?
BJOB:
114:699-704.
8-
Ohmi
H,
Hiiook
K,
&
Moohizuki
J.
(2002).
Fetal
and
the
timing
of
exposure
to
maternal
smoking.
Pediatric
Int;
44:55-59.
9-
Deplisheh
A.
et
al,
(2007).
Population
attributable
risk
for
adverse
pregnancy
outcomes
related
to
smoking
in
adolescent
and
adults.
Public
health;
do:
lC
10-T016.
10-
Jaakkola
N.
(2002).
Passive
smoking
during
pregnancy
and
early
childhood
occurrence,
determinants,
health
effect
and
prevention,
department
of
public
health
university
of
Helsinki.
11-
Kalinka
JL
(1999).
Passive
smoking
and
pregnancy
outcome
in
central
Poland,
human
and
experimental
toxicology,
18:
(4),
265-271.
12-
Pletsch
P.
&
Morqn
S.
(2002).
Smoke
free
families:
A
tobacco
control
program
for
pregnant
women.
JOGIN;
31
:(1):
39-46.
13-
Anderson
M,
Johnson
D,
&
Batal
H.
(2005).
Sudden
infant
Death
Syndrome
and
prenatal
maternal
smoking:
BMC
Medicine
3:4doi:10.
1186/1741-7015-3.
14-
Pirkle
J,
Bernert
J,
Caudill
S,
Sosnoff
C,
&
Pechacek
T
(2006).
Trends
in
the
exposure
of
nonsmokers
in
the
U.S.
population
to
second
hand
smoke:
1988-2002.
Environ
Health
Perspect;
114:853-858.
15-
Meeker
J,
Misser
S,
Cramer
D,
&
Hauser
J,
(2006).
Maternal
exposure
to
second
and
tobacco
smoke
and
pregnancy
outcome
among
couple
undergoing
assisted
reproduction,
human
reproductive,
22:
(2)
337-345.
16-
Venners
S,
Wang
X,
Chen
C,
Wang
L,
Chen
D,
&
Guang
W
et
al.
(2004).
Paternal
smoking
and
pregnancy
loss:
a
prospective
study
using
a
biomarker
of
pregnancy.
Am
J
Epidemiol;159:993-100t.
17-
Windham
G,
Swan
S,
Fenster
L
(1992).
Parental
cigarette
smoking
and
the
risk
of
spontaneous
abortion.
Am
Epidemiol;
135:1394-1403.
18-
Hanke
W.,
KaBinka
J.,
Florek
E.,
&
Sobala
W.
(1999).
Passive
smoking
and
pregnancy
outcome
in
central
Poland.
Department
of
Environmental
and
Occupational
Epidemiology
:4:
265-271.
19-
Ahluwalia
B.,
Grummer
L.,
&
Scanlon
K.,
(1997).
Exposure
to
environmental
tobacco
smoke
and
birth
outcome:
increased
effects
on
pregnant
women
aged
30
years
or
older,
American
journal
of
epidemiology,
146,42-47.
20-
Hong
Y
et
al,
(2001).
Maternal
genetic
effect
on
neonatal
susceptibility
to
oxidative
damage
from
environmental
tobacco
smoke,
journal
of
the
national
cancer
institute;
93:
(8):
45-
47.
21-
Wilcox
A
(2001).
The
importance
and
unimportance
of
birth
weight.
In
J
Epidemiol.
30:1233-41.
|
|
.................................................................................................................

|
| |
|

