Barriers,
Challenges and Way Forward for Implementation
of Person Centered Care Model of Patient and Physician
Consultation: A Survey of Patients' Perspective
from Eastern Mediterranean Countries
Waris Qidwai (1)
Kashmira Nanji
(1)
Tawfik A M Khoja
(2)
Salman Rawaf
(3)
Nabil Yasin Al Kurashi
(4)
Faisal Alnasir
(5)
Mohammed Ali Al Shafaee (6)
Mariam Al Shetti
(7)
Muntazar Bashir
(8)
Nagwa Eid Sobhy Saad
(9)
Sanaa Alkaisi
(10)
Wafa Halasa
(11)
Huda Al-Duwaisan
(12)
Amal Al-Ali
(13)
(1) Department
of Family Medicine, Aga Khan University, Karachi,
Pakistan
(2) Director General, Executive Board, Health
Ministers' Council for Cooperation
Council States
(3) Professor of Public Health, Director, WHO
Collaborating Centre, Department of
Primary Care and Public Health, School of Public
Health, Faculty of Medicine
Imperial College London, UK
(4) University of Dammam, Saudi Arabia
(5) Department of Family & Community Medicine,
Arabian Gulf University, Bahrain
(6) Vice Dean for Clinical Affairs, Oman Medical
College, Sultanate of Oman
(7) Family Physician, Bahrain
(8) Department of Family Medicine, King Faisal
Specialist Hospital and Research Centre, Jeddah,
Saudi Arabia
(9) Department of Family Medicine, Cairo University,
Egypt
(10) Senior Specialist Family Physician, Baghdad,
Iraq
(11) Family Physician, Amman, Jordan
(12) Head of the Primary Health Care Faculty
at the Kuwait Institution for Medical Specialization.
(13) Assistant Program Director in Family Medicine
Residency Program-Qatar.
Correspondence:
Dr. Waris Qidwai
Professor and Chairman,
Department of Family Medicine, Aga Khan University
Stadium Road, P.O. Box: 3500, Karachi 74800,
Pakistan
Fax: (9221) 3493-4294, 3493-2095
Email:
waris.qidwai@aku.edu;
warisqidwaikarachi@yahoo.com
|
Abstract
Background: Person-Centered Care
(PCC) is now considered a mandatory approach
in Patient-Physician consultation. The
aim of the study was to identify patients'
perception regarding barriers and possible
remedies for implementation of PCC in
Eastern Mediterranean Region (EMR).
Methods: A cross-sectional multi-country
study was conducted in six countries of
EMR during May 2014 to October 2014. Expert
Family Physicians from each country were
identified and asked to participate in
the study. The Family Physicians then
recruited Patients from their own clinics
(>18 years). Data analysis was performed
on SPSS 19 and results are reported in
the form of proportions, odds ratios and
95% confidence intervals.
Results: A total of 234 patients
were recruited, 60.6% were aged between
20 to 30 years and 36.3% of them were
males. 56% of the patients preferred Person-Centered
Care model for patient-physician consultation.
The major barriers identified by patients
in its implementing were; time constraints
(73.9%, OR: 1.5; 95% CI: 0.86-2.78), doctors
desire to control patient (OR: 2.6; 95%
CI: 1.55-4.49), cultural and religious
reasons (52.1%), increased cost (50.9%).
Patients responded that increased cost
related to Person-Centered Care practice
would be acceptable (58.1%), if increase
proved to be in the interest of better
health and care outcomes (40.6%).
Conclusion: Person-Centered Care
(PCC) is associated with significant barriers
in its implementation in Eastern Mediterranean
Region. These barriers can be overcome
in the interest of better health and care
related outcomes.
Key words:
Person-Centered Care, Physician-Patient
Consultation, Primary Healthcare, Eastern
Mediterranean Region.
|
Person-Centered Care (PCC) and its application
in patient/physician consultation is considered
a mandatory approach in some health systems
and is gaining popularity. It is the focus on
Patients and their needs along with placing
them at center point of Patient-Physician Consultation,
which has made its place indispensible in health
care delivery with better health outcomes. It
offers a much needed platform for agreement
on intervention and treatment plans between
Patients and their physicians, and it improves
Patient satisfaction and health care related
outcomes.(1, 2)
Despite proven benefits of Person Centered Care
(PCC), significant challenges still persist
in its implementation across the globe. Its
integration into clinical practice is often
found to be patchy and inconsistent even in
developed countries.(1, 3)
The situation in Eastern Mediterranean Region
(EMR) is no different. A recently conducted
multi-country, cross-sectional study across
six countries of EMR found that 36% of the patients
and 62.6% of physicians preferred a person-centered
model of medical care. (4) Better acceptability
of this model among physicians, in comparison
to patients, is most likely due to incorporation
of PCC model of patient/physician consultation
in training programs for physicians.
There is scientific evidence to suggest that
significant barriers exist in the implementation
of PPC model in clinical practice even in developed
countries and there are ways in which these
barriers and challenges can be overcome. (5)
This information provides us with the guide
to enforce this model in EMR.
Several evidence based barriers and challenges
to PCC implementation in clinical practice have
been identified.(6) Time constraint is an identified
barrier since PCC model takes more time to practice.
In order to expect a patient to make informed
decisions about a treatment, it is necessary
that the condition is explained in simple and
understandable language. Weakening of professional
power with staff experiencing reduction in professional
status, compromise in decision making power
and in autonomy to practice, are considered
other significant challenges for enforcement
of PCC model of patient/physician consultation
in clinical practice.(7)
The decision-making process by clinicians using
synthesized approaches must involve the patient.
It also reduces errors. (Figure 1)
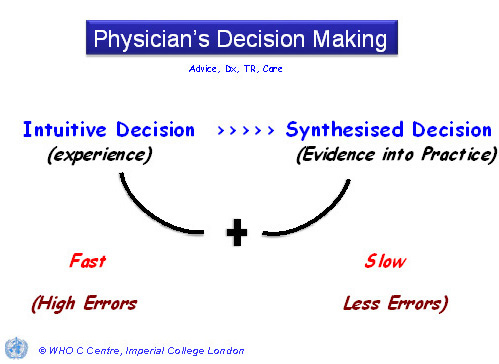
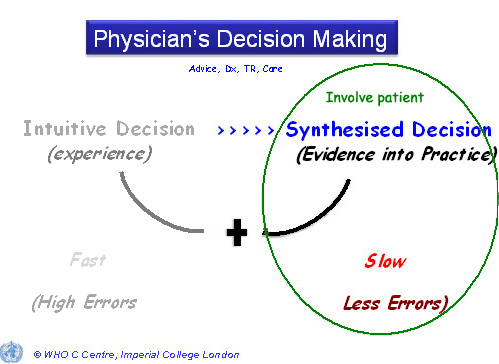
Figure 1: Decision making in Patient-Physician
Consultation
Lack of clarity exists about what constitutes
PCC, making it more difficult to practice and
to explain to patients.(7, 8) Its implementation
is even more challenging among patients with
communication difficulties (language barrier
or learning difficulties). Institutional policies
and non-conducive physical environments of care
make practice of Person Centered Care a challenging
task to practice.(9)
A need was established to look at barriers,
challenges and way forward for implementation
of PCC model of patient and physician consultation
within EMR Countries.
Study Setting:
This cross-sectional study
was conducted across six
countries (Iraq, Saudi
Arabia, Jordan, Egypt,
Bahrain and Pakistan)
of the EMR, from May 2014
to September 2014. These
countries were selected
to obtain patient's perception
on PCC, from diverse cultures
and socio-economic backgrounds.
Selection of Patients:
Family Physicians from
different countries were
invited to participate
in the study. They were
informed about the study
protocol and requested
to recruit patients coming
to their clinics, older
than 18 years and with
one or more presenting
problems. Patients were
excluded if they were
too ill to answer questions,
were agitated or in severe
pain.
Informed Consent:
Written informed consent
was obtained from all
participants after explaining
about the study protocol.
The study was conducted
in accordance with the
Helsinki Declaration.
Study tools:
A questionnaire was formulated
after compiling important
domains of PCC through
extensive Medline search
and by taking suggestions
from experts in the field.
The questionnaire focused
on the barriers (increased
cost, time constraints,
religious & cultural
barriers) of implementing
PCC, as perceived by the
patients. The questionnaire
was also translated in
Arabic, being a common
language in the region.
The questionnaire was
then pre-tested and ambiguities
were removed. The questionnaire
was composed of 2 sections:
The first section was
composed of demographic
details of the participants
while the second section
had questions on barriers
and their possible remedies.
Data analysis
Sample Size:
Data analysis was conducted
using Statistical Package
for Social Sciences (SPSS)
version 19. A post hoc
analysis generated a power
of 80% when 234 patients
were selected at 5% level
of significance.
Analysis:
Descriptive and inferential
statistics were performed.
Descriptive analysis was
conducted by obtaining
frequencies of all the
variables. Later, Logistic
regression analysis was
performed to identify
the barriers associated
with implementation of
PCC in EMR. Univariate
analysis was done to obtain
the independent effects
of barriers on preference
of PCC by patients. Since
none of the variables
were found to be significant
at the Univariate level,
therefore, multivariate
regression was not performed.
The results were reported
in the form of proportions,
unadjusted odds ratio
along with their 95% confidence
interval. Throughout the
analysis a P value of
< 0.05 was considered
statistically significant.
A total of 280 patients
were approached. 234
patients consented to
participate in the study,
yielding a response
rate of 83.5% (234/280).
About 60.6% of the patients
were between 20 to 30
years and the majority
of the patients were
females (63.7%). Over
half of the population
had more than 10 years
of schooling and 41.1%
were unemployed. Approximately
18% of the patients
were recruited from
Egypt (Table 1).
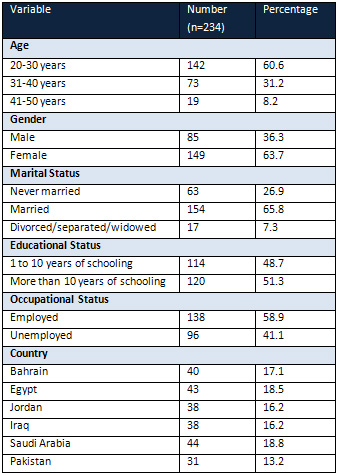
Table 1: Baseline
characteristics of Study
Participants
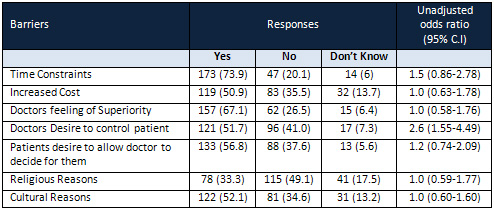
Table 2: Barriers in
Implementing Person
Centered Care in Eastern
Mediterranean Region
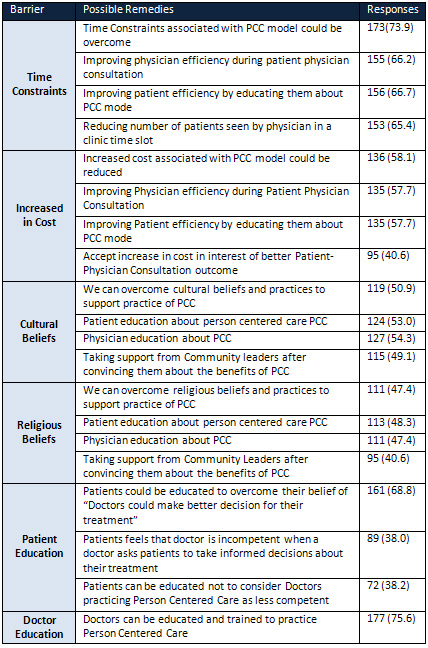
Table 3: Possible solutions
for overcoming barriers
to implement Person
Centered Care (PCC)
in Eastern Mediterranean
Region (EMR)
Barriers for implementation
of Person Centered Care
in EMR are presented
in Table (2). Slightly
under three quarters
of the patients believed
that time constraints
are a major barrier
(73.9%, OR: 1.5; 95%
CI: 0.86-2.78). This
is followed by doctors
feeling of being superior
(67.1%, OR: 1.0; 95%
CI: 0.58-1.76), doctors
desire to control patient
(OR:2.6; 95% CI: 1.55-4.49),
patients desire to allow
doctors to decide for
them (56.8%), cultural
reasons (52.1%), increased
cost (50.9%) and religious
reasons (33.3%).
Table (3) describes
the possible remedies
for overcoming barriers
to implementation of
PCC in the region. A
similar proportion of
patients responded that
time constraints associated
with PCC can be overcome
by improving physician
efficiency during patient
physician consultation
(66.2%), by improving
patient efficiency by
educating them about
the PCC model (66.7%)
and reducing number
of patients seen by
physician in a clinic
time slot (65.4%).
Patients responded that
increased cost related
to practice of PCC could
be reduced (58.1%) by
accepting increase in
cost in interest of
better patient outcomes
(40.6%). Half of the
patients recommended
that to overcome cultural
beliefs and practices
that hinder the practice
of PCC; support can
be taken from community
leaders after explaining
to them the benefits
of PCC.
Three quarters of the
patients responded that
doctors needs to be
educated and trained
to practice PCC during
patient-physician consultation.
Figure 2 depicts that
56% of the patients
preferred PCC model
for patient-physician
consultation in the
region.
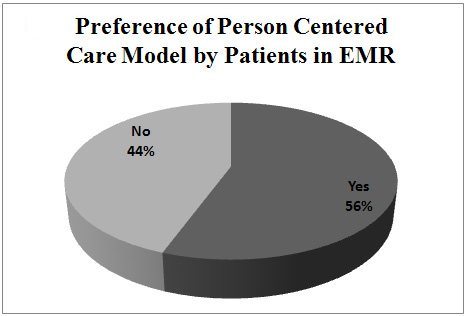
Figure 2
This
is
perhaps
the
first
study
from
EMR
that
has
looked
at
PCC
from
the
Patient's
perspective
in
the
context
of
challenges,
barriers
and
way
forward.
The
sample
is
of
a
reasonable
size
even
though
it
covers
younger
people
and
particularly
more
women.
Most
of
the
study
participants
were
fairly
educated
yet
stated
to
be
unemployed,
being
housewives
and
looking
after
their
families.
Despite
these
shortcomings,
the
findings
are
relevant
and
have
practical
implications.
It
is
heartening
to
note
that
more
than
half
of
the
respondents
favor
implementation
of
person
centered
model
for
patient
physicians'
consultation
in
the
region.
A
study
conducted
in
the
region
on
patients
and
physicians
perceptions
regarding
PCC
also
found
support
for
PCC
model
among
more
than
50%
of
respondents.(4)
It
is
not
a
surprise
to
note
that
"time
constraint"
has
come
out
as
a
barrier
for
implementation
of
PCC
in
the
region,
and
this
is
possibly
because
of
several
reasons.
In
order
to
implement
PCC
model
for
patient-physician
consultation,
it
will
be
necessary
to
make
the
patient
the
focus
of
consultation
through
empowering
them.
The
patient
will
have
to
be
informed
about
his
or
her
condition
and
available
evidence
based
choices
in
enough
detail
and
simple
understandable
language,
to
enable
him
or
her
to
reach
meaningful
decisions.
All
these
measures
increase
patient-physician
consultation
time
and
costs
that
can
be
curtailed.
"Increased
cost"
is
another
related
barrier
for
implementation
of
this
model
of
Patient-physician
consultation,
and
has
come
out
strongly
in
this
study.
There
is
evidence
to
suggest
that
with
proper
planning
and
execution,
additional
costs
associated
with
Person-Centered
model
of
care
can
be
reduced.
(10,
11)
There
is
evidence
that
with
proper
implementation
of
PCC
model,
patient-physician
costs
can
be
cut
in
the
long
run.(12,
13)
It
is
not
surprising
that
patients
consider
it
worthwhile
to
invest
time
and
cost
to
empower
Patients
and
implement
person
centered
model
for
patient-physician
Consultation.
Improving
physician's
efficiency
and
educating
both
patient
and
physicians
about
the
process
for
this
model
of
consultation
will
reduce
time
and
cost
required
for
this
type
of
clinical
encounter.
It
is
interesting
to
note
that
Patients
consider
a
physicians'
desire
to
control
patient-physician
consultation
and
their
feeling
of
being
superior,
(14,
15)
as
a
barrier
to
implement
person
centered
model
for
patient-physician
consultation.
Another
related
barrier
identified
in
this
study
is
the
desire
of
patients
for
physicians
to
decide
for
them.(15)
Such
barriers
can
be
removed
by
educating
both
patients
and
physicians
that
they
are
equal
partners
in
the
consultation
and
that
the
benefits
of
having
the
patient
as
the
focus
of
the
encounter
are
not
only
beneficial
for
health
related
outcomes,
it
does
not
compromise
the
respect
that
they
have
and
enjoy
during
the
Consultation
process
as
equal
human
beings.
Cultural
and
religious
reasons(16,
17)
have
been
quoted
as
barriers
to
implementation
of
person
centered
model
for
patient-physician
consultation.
In
some
societies,
physicians
have
been
and
still
are
considered
'next
to
God'.(15)
Patients
are
unfortunately
not
considered
capable
of
making
health
care
related
decisions
in
our
society.
A
physician
has
traditionally
and
historically
enjoyed
tremendous
respect
and
a
patient
has
been
a
passive
recipient
of
medical
care
given
by
a
physician.
Against
this
background,
introduction
of
patient-physician
model
of
consultation
that
puts
the
entire
focus
on
the
patient
has
been
and
continues
to
be
a
challenge.
Respondents
have
suggested
that
community
leaders
can
be
asked
to
support
this
model
and
education
of
both
patients
and
physicians
with
regards
to
it
can
help
overcome
cultural
as
well
as
religious
barriers
for
its
implementation.
PCC
is
associated
with
significant
barriers
in
its
implementation
in
EMR.
These
barriers
can
be
overcome
in
the
interest
of
better
health
care
related
outcomes.
It
is
the
responsibility
of
all
stakeholders
and
health
care
providers
to
ensure
that
barriers
are
removed
and
practice
of
person
centered
model
of
patient-physician
consultation
is
enforced
in
EMR.
We
are
thankful
to
the
study
participants
(patients
and
physicians),
management
and
staff
of
all
of
the
hospitals/clinics
in
EMR
for
their
support
and
help
throughout
the
data
collection
period.
1.
Ekman
I,
Swedberg
K,
Taft
C,
Lindseth
A,
Norberg
A,
Brink
E,
et
al.
Person-centered
care
-
ready
for
prime
time.
Eur
J
Cardiovasc
Nurs.
2011;
10(4):248-51.
2.
Longworth,
D.
L.
Accountable
Care
Organizations,
the
Patient-Centered
Medical
Home,
and
Health
Care
Reform:
What
Does
It
All
Mean?
Cleveland
Clinic
Journal
of
Medicine
2011,
78(9),
571-582.
3.
Mezzich
JE,
Snaedal
J,
van
Weel
C,
Botbol
M,
Salloum
IM
(2011):
Introduction
to
Person-centered
Medicine:
From
Concepts
to
Practice.
Journal
of
Evaluation
in
Clinical
Practice
17:
330-332.
4.
Qidwai
W,
Nanji
K,
Khoja
T
A
M,
Rawaf
S,
Al
Kurashi
N
Y,
Alnasir
F,
Shafaee
M
A,
Shetti
M
A,
,
Bashir
M,
Saad
N
E
S,
Alkaisi
S
and
Halasa
W.
Are
we
ready
for
a
person-centered
care
model
for
patient-physician
consultation?
A
survey
from
family
physicians
and
their
patients
of
East
Mediterranean
Region.
European
Journal
for
Person
Centered
Healthcare
2013.
Vol.
1
Issue
2
pages
394-404.
5.
Ruggiano
N,
Edvardsson
D.
Person-centeredness
in
home-
and
community-based
long-term
care:
current
challenges
and
new
directions.
Soc
Work
Health
Care.
2013;
52(9):846-61.
6.
Kelly
J.
Barriers
to
achieving
patient-centered
care
in
Ireland.
Dimens
Crit
Care
Nurs.
2007;26(1):29-34
7.
Lutz,
BJ,
&
Bowers,
BJ,
'Patient-centred
care:
understanding
its
interpretation
and
implementation
in
health
care',
Scholarly
Inquiry
for
Nursing
Practice,
2000
vol.
14,
no.
2,
pp.
165-83.
8.
Mead,
N,
&
Bower,
P,
'Patient-centeredness:
a
conceptual
framework
and
review
of
the
empirical
literature',
Social
Science
and
Medicine
2000,
vol.
51,
no.
7,
pp.
1087-110.
9.
A
Victorian
Government
Initiative.
National
Ageing
Research
Institute.
What
is
person
centered
care?
A
literature
review.
[Internet]
2006.
[Cited
Jan
14,
2015]
Page
1.
Available
from:
http://www.mednwh.unimelb.edu.au/pchc/downloads/PCHC_literature_review.pdf
10.
Rosenberg
CN,
Peele
P,
Keyser
D,
McAnallen
S,
Holder
D.
Results
from
a
patient-centered
medical
home
pilot
at
UPMC
Health
Plan
hold
lessons
for
broader
adoption
of
the
model.
Health
Aff
(Millwood).
2012;
31(11):2423-31
11.
Fishman
PA,
Johnson
EA,
Coleman
K,
Larson
EB,
Hsu
C,
Ross
TR
et
al.
Impact
on
seniors
of
the
patient-centered
medical
home:
evidence
from
a
pilot
study.
Gerontologist.
2012;
52(5):703-11
12.
The
Medical
Home.
The
Person
Centered
Health
System
and
the
Medical
Home.
[Internet]
2015.
[Cited
Feb
3,
2015]
Available
from:
http://medicalhome.org.au/the-person-centred-health-system-and-the-medical-home/
13.
Hansson
E,
Ekman
I,
Swedberg
K,
Wolf
A,
Dudas
K,
Ehlers
L,
et
al.
Person-centered
care
for
patients
with
chronic
heart
failure
-
a
cost-utility
analysis.
Eur
J
Cardiovasc
Nurs.
2015.
14.
Mansfield
CJ,
Mitchell
J,
King
DE.
The
doctor
as
God's
mechanic?
Beliefs
in
the
Southeastern
United
States.
Soc
Sci
Med.
2002;
54(3):399-409.
15.
Qidwai
W.
Paternalistic
Model
of
Medical
Practice.
J
Coll
Physicians
Surg
Pak.
2003
May.
13(05):
296
16.
Jaikrit
Bhutani,
Sukriti
Bhutani,
and
Jai
Kumar.
Achieving
patient
centered
care:
Communication
and
cultural
competence.
Indian
J
Endocrinol
Metab.
2013;
17(1):
187-188.
17.
Epner
DE,
Baile
WF.
Patient-centered
care:
the
key
to
cultural
competence.
Ann
Oncol.
2012
Apr;
23
|

