Analyzing
the Medical and Non-medical aspects of Medical
Consultation in the city of Visakhapatnam
Supriti Agarwal (1)
Sonia Singh (2)
(1) Dr Supriti
Agarwal, Assistant Professor,
Amity University, Noida, India
(2) Dr. Sonia Singh, Assistant Professor
Al Dar University College
Dubai, United Arab Emirates
Correspondence:
Dr Supriti Agarwal
Assistant Professor,
Amity University, Noida, India
Zip- 201313
Email:
sagrawal2@amity.edu
|
Abstract
The Indian healthcare industry has the
potential to reach $ 280 billion by 2020
(KPMG Report) reflecting a compounded
growth of 17-18%. Indian health care is
witnessing a huge change in the form of
disease profile. Currently, 34% of death
is happening due to infectious disease
and 53% of death is due to lifestyle diseases.
In spite of the technological advancement
in medical sciences, diseases are engulfing
human life. It creates a perplexed situation.
The patient enters a medical practitioners'
chamber with a high hope at the appointed
time, but this consultation session is
both a meaningful or superficial interaction.
It is indeed a situation of dilemma
.
This case highlights the dilemma that
exists in the medical practitioner's chamber
related to patient interaction. Basically,
consultation session in the medical practitioners'
chamber varies from one patient to another.
There are various reasons for this variation.
Maybe the patient is a first timer or
the patient is accompanied by an attendant
or the presence of a pharmaceutical manager
in medical practitioner's chamber is creating
the difference. It can be also due to
change in disease profile (infectious
or lifestyle related). The public sector
is keenly participating in the treatment
of communicable diseases and the private
sector is trying for lifestyle related
diseases.
This case study is an observational study
conducted at Visakhapatnam (port city
in Andhra Pradesh). Visakhapatnam has
been a centre of pharmaceutical companies
from the last one decade. Three specialties
(Cardiologist, diabetologist and Oncologist)
were selected. Different situations were
recorded and analyzed in these consulting
sessions through observational schedule.
Results indicated there are many reasons
for the uniqueness. It can be used as
training materials to the medical representatives
as they get to know what exactly is happening
in the chamber and helps them in preparing
for their meeting with the doctors.
Key words: Medical consultation
session, Doctor-patient interaction, Pharmaceutical
marketing strategies, medical practitioners.
|
|
A TYPICAL SCENE FROM A MEDICAL CONSULTATION
... |
The patient
I had taken two hour break from my office
for routine sugar check up. Although my reports
were ok, still I am little bit worried. Two
days back I lost my colleague, who was only
34 year old. He was also diabetic and succumbed
to fatal heart attack. I started to enquire
about the extent of diabetes from my fellow
patients. Some were very hopeful and some were
depressed. I was really very much in a dilemma.
What is my future? This question had perturbed
me so much, that I started viewing my watch.
Now, this waiting time was troubling me a lot.
Just then the receptionist called my name. Finally,
I entered the doctor's clinic…….I
showed him my reports. Doctor congratulated
me for my good control on sugar level and enquired
about exercise schedule. I assured him about
the regularity of exercise schedule. He listened
and started writing prescriptions. I thought
I should ask about a few more doubts, but his
speed of writing the prescription was a clear
cut signal that my time is up. Or perhaps I'll
ask next time.
The doctor
I'm a leading Endocrinologist consulting
in a leading hospital… yet another busy
day. It's 12.00 pm. Seventh patient comes in,
clearly upset and angry, as he was waiting for
more than one hour after his appointment time.
I am aware they book multiple patients at the
same time, but what can I do about that? Anyway,
I felt sorry for him but really can't do much,
as consultation time will be over by 1.00 pm
and nine more patients are in the queue. I started
enquiring about his sugar level and gave a few
general instructions in a hurry. He didn't get
himself diagnosed as he required a few tests;
therefore I didn't change any medicine and asked
him to visit me again with the test reports.
The patient seemed to be in gloomy state which
made me think that he wouldn't comply with my
instructions. I tried to make him cheerful at
the end , but it was in vain.
Epilogue: This was a typical situation
happening during medical consultation. Nobody
wants to fall ill, but, still one had to visit
a doctor's clinic. Thankfully, nowadays a doctor's
consultation chambers infuse a feel good factor
in the patient's mind. Still! Illness had a
negative impact on both the physical and mental
status of the patient. Certainly, modern lifestyles
have resulted in a variety of ailments. A recent
report of WHO highlighted that lifestyle diseases
accounted for 5.2 million (50.5%) of the 10.3
million deaths in India (2005) compared to 35
million (60.3%) of 58 million deaths worldwide.
By 2050, people over 60 years will increase
from 76.6 million (7.4% of total population
in 2001) to 300 million (17% of the population).
A great amount of money is being spent on medicine
marketing by pharmaceutical companies in various
ways, but they have not assessed the potential
of the medical consultation. A study by world
bank economist Jishnu (Hindustan times) found
that in India, average consultation time per
patient both at government and private hospitals
was 5.3 minutes and the rate of correct diagnosis
was just 21.8 %.
Generally, pharmaceutical marketing expenditure
is incurred on analyzing and understanding the
prescribing behaviour of medical practitioners
only, but if they start analyzing the quality
of doctor- patient interaction during medical
consultation, it will definitely add more value
in pharmaceutical interaction with medical fraternity.
The case: This case study is based on
the medical consultation belonging to three
types of chronic ailments, i.e. (Diabetes, Cardio-vascular
disease and Cancer) conducted at Visakhapatnam,
a port city in Andhra Pradesh. Visakhapatnam
has a 5 million Telugu speaking population displaying
a cosmopolitan nature. Visakhapatnam has many
hospitals ranging from the King George Hospital
to multi specialty hospitals like Care hospitals,
Apollo hospital, etc. These hospitals are catering
to the demand of diseases ranging from the smallest
flu to the biggest death causing infections.
The study is qualitative in nature. Observation
method was adopted for collecting data. Consultation
observation tool was prepared. Questions were
based on medical as well as nonmedical (psychosocial)
perspectives of medical consultation. This study
was carried out in the 7 hospitals at Vishakhapatnam
city. The consultation observation tool was
filled in by doctors. An observer was present
in the medical consultation session for noting
down the details of the medical consultation
session.
There are various numbers of consultation models
in existence, but most influential model is
the Calgary-Cambridge approach. This model identifies
five main stages (Figure 1) in the medical consultation
session.
Figure 1: Calgary-Cambridge Approach
•
INITIATING THE SESSION
• GATHERING INFORMATION
• PHYSICAL EXAMINATION
• EXPLANATION AND PLANNING
• CLOSING THE SESSION |
This framework provides structure and emphasizes
the importance of building a good doctor- patient
relationship. It is patient-centred and emphasizes
effective communication and gives the direction
for recording information from the consultation
session. But it gives little consideration for
the social, psychological and behavioural dimensions
of illness. In order to understand the process
of medical consultation, the consultation session
can be real or simulated. They can be observed
or recorded in a number of ways, such as:
1. An observer 'sits in' on real consultation
session.
2. An observer may watch through a one-way
glass so that they are not physically present
in the consultation.
3. Consultations can be recorded and
analyzed by using appropriate rules and guidelines.
4. Consultations can be described and
discussed after the consultation by doctors,
doctor and patient or more widely with others.
5. Mock consultations can be planned
with participants playing the role of doctor
or patient.
This case study is developed through the first
method (presence of observer in the real consultation
session) and revolving around the stages mentioned
in the Calgary-Cambridge model.
Lifestyle diseases such
as diabetes and hypertension
are commonly found associated
with rural and tribal
areas of Vishakhapatnam.
The findings are the
result of a six-month
pilot study on non-communicable
diseases (NCDs) being
undertaken by the Public
Health Foundation of
India (PHFI) in collaboration
with the Union health
ministry's directorate
of NCD and Nature NGO.
The main causes of these
diseases are changes
in lifestyle and diet
pattern, besides genetic
predisposition and weak
immunity system.
This case study analyzes
the nuances of the consultation
session. The table below
depicts a summary of
the patient details
which have been used
for analyzing the medical
consultation session.
Table 1: Patient Details
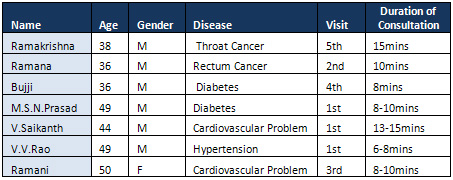
This case study
is developed for three
types of patients, i.e.
those suffering from lifestyle
diseases such as Diabetes,
Cardio-vascular problems
and Cancer. Observations
derived through the medical
consultation sessions
for 7 different patients
are illustrated as follows:
Ramakrishna agony of
Cancer…..
Ramakrishna, 38, works
as a drawing teacher
in a local private school
for the past 10 years.
One morning, he observed
some unwanted growth
on his throat which
was very disturbing.
On his meeting with
the doctor, it was confirmed
that it is an unwanted
growth which has to
be removed by chemotherapy.
Chemotherapy cycles
were planned and everything
was going well. On his
completion of the 4th
cycle out of 6 cycles,
Ramakrishna came to
visit the doctor to
give a report of his
health condition. Ramakrishna
was escorted by his
wife who stood supportive
all through the treatment.
The doctor started the
conversation and asked
about the well being
of Ramakrishna for which
the response was good.
Ramakrishna came up
with several doubts
regarding the necessity
of PET scan. The doctor
explained the relevance
of the scan as it supports
the normal CT (Computer
tomography). Hence it
helps in understanding
the condition of the
patient better. Ramakrishna
also complained about
the insomnia he is suffering
from for which the doctor
prescribed some sedatives
that will help the patient
to have a sound sleep.
Ramakrishna was completely
relieved of the tension
and greeted the doctor
while leaving the chamber.
This case indicates
that consultation session
(15 minutes) was not
only filled with the
biomedical (technical)
investigations, but
filled with the real
sharing of the patient's
concern and fear (psychosocial
session). This doctor-patient
communication process
has been widely researched
in the context of medical
teaching and training
in many studies conducted
by Kurtz et al (1998)
& Silverman et al
(2005).
Now, another case is
about a low profile
village farmer, who
is shocked at hearing
about his diagnosis
of cancer.
Ramana was shocked………
Ramana, 36, is a farmer
who lives in a village,
150 km away from the
city, and leads a common
life. Ramana suddenly
started facing some
problems in the stomach
which made him feel
sick. Ramana came to
know that he was suffering
from advanced rectum
tumour which he earlier
believed was some sort
of stomach problem.
Treatment included radiation
therapy which had to
be completed in 6 cycles.
The 1st cycle was successful
and he arrived to be
admitted to hospital
for the 2nd cycle to
commence. Ramana was
completely preoccupied
with the tensions regarding
his family, children
and work.
The doctor grasped
the situation of Ramana
and greeted him in a
comforting manner. He
made the patient comfortable
in the chamber by enquiring
about his family condition,
financial status and
about the consequences
of the first chemotherapy
cycle. Ramana gave one
word answers all the
time. The doctor also
checked the reports
and previous prescriptions
which helped him to
get an idea of the treatment
and the stage which
he needed to continue.
Ramana was examined
physically for about
a minute. "The
second cycle will start
from tomorrow and the
whole process will be
completed within 3 months.
You should be prepared
to get admitted to the
hospital and you have
to stay for the entire
period of chemotherapy"
remarked the doctor.
"Yes" is the
answer from Ramana.
Meanwhile, Ramana also
pointed towards his
wife who had accompanied
him with all the requirements
for his 3 months. The
doctor asked the nurse
to take care.
Here the session lasted
only for ten minutes
and covered the biomedical
aspect as the doctor
tried his level best
in reducing the shock
level of Ramana. Then,
patient became stronger
in accepting the mode
of treatment. This aspect
was similarly seen in
the study of Maguire
P et al 1996, as they
established key tasks
of the consultation
while conducting research
into doctor-patient
communications. It includes
patients' problems and
concerns, giving information,
discussing treatment
options and unconditional
support of the medical
fraternity. Studies
(Balint M; 1964) reveal
that doctor make patients
feel better when they
listen to the patients
attentively. Another
study by Jenkins et
al (2001) found that
87% of hospitalized
cancer patients interviewed
desired all the information
about their disease,
good and bad, and 98%
preferred to know whether
or not their illness
was cancer. Numerous
studies have also examined
the relationship between
cancer pain and various
forms of psychological
distress, including
mood disturbance, anxiety,
depression, emotional
distress, fear, and
worry (Francis et al.
2004).
Now-a-days, diabetes
is also becoming a major
problem and is considered
as the 'long-term sickness'
in people over the age
of 50 years (Waddell
& Aylward 2005).
Globally 366 million
people are suffering
from diabetes as per
2011 statistics. By
2030 it is expected
to double. While China
is leading in diabetic
population with about
97 million, India is
second only to China
with about 77 million
diabetic patients, said
Dr. Saxena, Chief advisor,
Kareus Therapeutics,
SA, during a symposium
at DRILS in Hyderabad
Central University.
Next observation is
of a government worker,
who has been suffering
from diabetes for the
last four years.
Bujji appearing for
routine check-up for
Diabetes ……….
Bujji, 36, works in
the government sector,
and has been suffering
from diabetes for the
past four years. He
only consulted a general
physician for the treatment.
The doctor examined
the previous prescriptions
and reports "There
is nothing much to worry
about regarding the
diabetes in your case,
as the sugar levels
are under good control
and you only have to
take precautions in
terms of diet and lifestyle"
he continued ."Get
your sugar level's checked
and show me the reports
after 3 months",
replied the doctor.
A sympathetic gesture
of the doctor brought
a smile to Bujji's face.
This 8 minute consultation
session highlighted
the psychosocial aspects.
Here observation is
displaying strong emotional
bond between doctor
and patient. It was
seen here that the doctor
tries to teach Bujji
the basics of self-management
for diabetes. Definitely
these self-management
sessions had strengthened
the doctor and patient
relationship over time.
This case justified
the study of Mishler
1984 that came up with
a disease centred model
where the doctors talk
in terms of medicine
only. Their main aim
and objective depends
on the explanation of
physical symptoms to
the patient and thus
the doctor listens to
the 'voice of the patient',
and encourages the patient's
active involvement in
the consultation. Thus,
a positive reply from
the patient drafts a
positive impact on health
care and status (Esterling
B et al 1990).
Another case is of Prasad,
who thought that his
eye infection was due
to his diabetes. But
the medical consultation
unfolded a different
story.
Prasad is confused by
the eye infection………..
A
case of Doctor-patient
exchanging information
M.S.N Prasad, male,
aged 49 works as
a conductor in a
government corporation
arrived to the clinic.
Doctor greeted the
patient with a smile
and Prasad occupied
the seat in front
of the table. The
session started
with formal greetings
from both of them
as they knew each
other, belonging
to the same department.
And the conversation
begins.
Prasad: "Doctor,
I have infection
in my eyes and they
are hurting a lot."
Doctor: "Let
me observe your
eyes first."
After a keen observation
into the cornea,
doctor came up with
some questions,
"Did you eat
anything which is
not in your regular
diet?"
Prasad: "Doctor,
I had mangoes which
literally started
irritation in my
eyes. Can eating
mangoes affect a
person?"
Doctor: "See,
it's not like that.
It depends on various
reasons. Did you
have this problem
before or did it
show after you had
this diet?"
Patient was a little
confused at this
answer. Immediately
the doctor came
up with some more
questions. "Do
you smoke?"
Prasad: "Yes"
was the answer after
some seconds of
silence.
Doctor: "Anybody
in your family suffered
from blood sugar
or any hereditary
disease?"
Prasad: "Yes
doctor. My mother
has a diabetic history
and she has been
treated for the
past ten years.
Is this blood sugar
doctor?" asked
the patient with
some state of tension
in his mind.
Doctor: "No,
I can't come to
a conclusion right
now. I have to perform
some basic tests.
I am prescribing
some medicines which
will reduce irritation
and also some tests
to be performed"
and continued "Please
meet me next time
with all your reports"
Prasad: "Yes
doctor, I will be
quitting smoking
as soon as possible".
Doctor: "Remember,
it's better to quit
smoking, it will
certainly help you
a lot" the
doctor ended the
consultation session.
|
In this consultation,
it was observed that
doctor was very much
pleased to hear the
positive reply from
the Prasad and therefore
session ended with the
positive note. This
medical consultation
session covered purely
biomedical aspects.
Psychological stress
in the workplace is
generally regarded by
the public as an important
cause of coronary heart
disease. While epidemiological
studies have amply demonstrated
a strong, consistent
relation between coronary
disease and cigarette
smoking, high blood
cholesterol, hypertension,
diabetes, and family
history (Kannel et al.1976;
Kannel et al 1986).
In India, three out
of every 1,000 people
suffer a stroke. The
number of deaths due
to heart attack was
projected as 1.2 million
to two million in 2010.
Studies (Ford et al
1997) found that doctor
feel that satisfied
patients follow the
treatments more religiously.
Now analyzing the medical
consultation session
for patients suffering
from cardiovascular
problem, the first patient
is V.Saikanth, who is
trying to figure out
the cause of chest pain
in his consultation
with the doctor.
Saikanth presented due
to severe pain in chest……………
V Saikanth, 44, is from
a middle class family
and he suffered some
unbearable pain that
rose from his chest
and made him to fall
tothe ground. Hence
Saikanth visited a specialist
doctor as recommended
by his friends.
Saikanth was escorted
by his wife. The doctor
examined Saikanth by
making him to perform
some breathing patterns.
The doctor also examined
the pulse, blood pressure
and the patterns of
heart beats. The doctor
started explaining the
case, "There is
nothing to worry much.
Your reports show that
you are fit and fine.
The main problem is
there is a blockage
in your blood vessel
which resulted in unbearable
pain. The solution for
this problem is to insert
stents which will clear
the blockage. Stents
are in the shape of
small tubes which free
the blood vessels from
blockages and help in
the free flow of blood.
The operation can be
scheduled in the next
week once all matters
are settled".
Saikanth replied, "Yes
doctor! I will be ready
with the arrangements
as soon as possible".
"Don't worry!!
Everything will be fine"
assured the doctor which
made the patient feel
comfortable and walk
out from the consultation
chamber with a cool
mind.
This session highlighted
both perspectives (psychosocial
& biomedical) of
the consultation session
and lasted up to 13-15
minutes. Hence the medical
practitioner was trying
to make the patient
feel satisfied and comfortable
in the entire session.
If the outlook of the
medical practitioner
provides a credible
self help approach to
the patient, definitely
the medical consultation
session will necessary
move from a 'disease
model' to a 'bio psychosocial
model' (Waddell &
Aylward 2010). Further
Maguire & Pitceathly
(2002) also emphasized
that the usage of more
open ended questions
should be adopted in
dealing with psychosocial
and complex emotional
issues and then only
will patients be more
involved in the session.
The last case is of
Mrs. Ramani. She is
trying hard to manage
high blood pressure
and increased level
of cholesterol.
Although Mrs Ramani
is vigilant about her
illness, still, there
is a long way to go…………….
Mrs.
Ramani, 50, is a
school teacher.
She had increased
level of cholesterol
and elevated blood
pressure for which
medications have
been prescribed.
For the past few
weeks, she has been
suffering from aches
and pains in the
legs which is disturbing
her dailyroutine.
She enters the chamber
with her son as
an escort.
"How are
you Mrs. Ramani?
Is everything going
fine?"
questioned the doctor.
"Doctor, I
am fine but, I had
severe ache and
pains in my legs
for the last few
weeks. I am a school
teacher; therefore,
I have to stand
throughout the day.
This is not new
to me but pain has
started suddenly
and is disturbing
my entire work schedule"
replied the patient.
"Do you have
anything new in
your diet?"
asked the doctor.
"Yes, I have
started taking fresh
grapefruit juice
that makes me energetic
and improves my
energy levels also,
so that I can get
on with my work
perfectly"
replied the patient.
"Yes, this
is the main reason
for your aches and
pains in the legs.
Grapefruit juice
is contraindicated
to the medications
which you are taking.
The main side effect
is myopathy or muscular
weakness and it
is the main reason
for your pain"
explained the doctor
patiently.
"So, Should
I stop grapefruit
juice doctor? Is
there anything more
I have to modify
in my diet?"
asked the patient.
"Yes, of
course! Stop having
grapefruit juice;
I am also prescribing
some new medications
which will relieve
you from pain or
muscular weakness.
Next time, please
consult me before
trying anything
new in the diet"
replied the doctor.
|
Medical
consultation
is
indeed
a
very
important
phenomenon,
as
it
initiates
the
rapport
between
doctor
and
patients.
Medical
consultation
is
not
only
about
doctor-patient
relationship
but
it
also
includes
doctor
and
pharmaceutical
representative
relationship.
Thus,
these
skills
are
of
great
benefit
to
doctors,
patients
and
pharmaceutical
representatives,
as
they
are
a
direct
or
indirect
link
to
consultation
phenomenon.
According
to
Pendleton
(1984),
consultation
is
'the
central
act
of
medicine'
which
'deserves
to
be
understood.'
It
is
focal
to
the
transaction
between
doctors
and
patients
and
plays
a
crucial
role
in
the
relationship
between
doctors
and
patients
(Smith
R
2003).
It
influences
the
precision
of
diagnosis
and
treatment,
and
studies
have
indicated
that
over
80%
of
diagnoses
in
general
medical
clinics
are
based
on
the
medical
history.
There
are
three
main
aspects
of
medical
consultation
session.
They
are:
Preparation,
Establishing
initial
rapport,
and
Identifying
the
problems
and
concern.
Click
here
for
Picture
1:
Consultation
Session
Preparation:
In
preparing
for
a
consultation,
an
optimal
setting
is
required.
It
includes
the
setting
of
consultation
room
and
waiting
lounge.
It
should
be
neat
and
tidy.
Time
management
is
a
very
important
aspect
in
medical
consultation
session,
as
it
not
only
includes
quality
of
the
consultation
session
but
also
waiting
time.
Establishing
initial
rapport:
During
the
consultation
session,
it
is
essential
to
develop
a
comfortable
bonding
between
doctor
and
patient.
Generally
the
doctor
sees
at
least
10
-15
patients
in
their
consultation
hour,
therefore
it
becomes
pertinent
for
the
medical
practitioners
to
understand
the
patient's
history
and
illness.
Only
then
does
the
real
diagnosis
happen.
Identification
of
problems
and
concern:
Once
the
patient
finishes
the
discussion
of
symptoms,
he/she
wants
to
know
the
mode
of
treatment.
If
the
session
has
gone
well,
then
it
leads
to
successful
identification
of
the
illness
and
the
treatment
regime
will
be
considered
by
the
patient.
Thus,
more
recent
approaches
to
medical
consultation
is
not
just
assessment
of
medical
anomaly
but
also
assessing
non-medical
(psychosocial)
issues
along
with
the
history
of
illness
(See
Diagram-1).
Broadly,
a
medical
consultation
session
should
cover
two
aspects,
i.e.
Medical
(Biomedical
aspects)
and
Non-medical
(Psychosocial
aspects).
Medical
aspects
include
the
pathophysiology
of
disease
that
is
assessed
through
symptoms
of
the
disease,
analyzing
the
diagnostic
report
and
the
history
of
illness.
Non-medical
aspects
include
the
true
emotional
trauma
of
patients
behind
their
illness.
Basically,
a
good
consultation
should
follow
a
set
schedule
which
starts
with
the
formal
interaction
and
goes
into
the
depth
of
concern
areas.
Gask
and
Usherwood
identified
three
major
features
of
the
consultation.
They
are
as
follows
(a)
Style
with
which
a
doctor
listens
to
a
patient
will
influence
what
they
say.
(b)
Effective
communication
between
doctor
and
patient
leads
to
improved
outcome
for
many
common
diseases.
(c)
Patients'
compliance
will
be
improved
if
the
management
plan
has
been
negotiated
jointly.
Once
these
features
are
met
in
the
consultation
session,
only
then
are
they
effective
and
fruitful.
Many-a-times,
doctors
often
fail
in
covering
all
these
tasks.
They
cannot
get
the
correct
information
regarding
the
patient's
agony
and
this
effects
quality
of
consultation.
They
do
not
check
how
well
the
patient
has
opened
up
with
their
problems
and
thereby
rapport
cannot
be
established.
Henceforth,
doctors
should
be
competent
in
maintaining
fruitful
interaction
with
patients.
It
is
estimated
that
a
doctor
might
perform
200,000
medical
consultations
in
his/her
lifetime
but
the
success
of
the
medical
consultation
depends
on
the
doctor's
clinical
knowledge,
interview
skills
and
doctor-patient
relationship.
A
study
by
Roter
and
colleagues
(1998)
concluded
that
those
physicians
who
are
trained
in
non-verbal
communication
skills,
ask
more
open-ended
questions,
and
use
greater
emotional
talk
and
are
more
likely
to
receive
greater
personal-
and
disease-related
information
from
their
patients.
It
leads
to
more
satisfied
patients
and
their
chances
to
follow
the
treatment
prescribed
more
strenuously
(Ford,
Bach,
and
Fottler
1997;
Parente,
Pinto,
and
Barber
2005;
Zandbeh
et
al.
2007).
Consultation
time
also
plays
a
crucial
role
in
assessing
the
quality
of
medical
consultation
session.
Generally,
medical
consultations
last
about
6
minutes,
although
this
can
vary
from
about
2
minutes
to
over
20
minutes.
This
time
pressure
results
in
tightly
controlled
doctor-centred
(or
'paternalistic')
consultation
with
less
attention
paid
to
the
social
and
psychological
aspects
of
a
patient's
illness.
Therefore,
less
psychological
problems
are
identified
and
more
prescriptions
are
issued
(Howie
et
al
1992).
Average
consultation
time
was
found
to
be
8
minutes
in
a
UK
study.
Other
studies
conducted
by
Ridsdale
and
his
colleagues
(1992)
conclude
that
the
time
available
for
consultations
was
increased
to
10
minutes.
Patients'
satisfaction
would
have
increased
by
improving
the
way
time
is
spent
within
the
consultation
(Ogden
J
2004).
Satisfaction
can
be
infused
only
when
the
doctor
increases
the
time
of
consultation
and
explains
the
patient's
concerns
clearly
(Tuckett
et
al
1985).
Another
qualitative
study
by
Barry
et
al
(2000)
that
was
based
on
35
patients
(18
years
plus)
and
20
general
practitioner
consultants,
found
that
only
four
of
35
patients
voiced
their
concerns
during
the
consultation.
Again
this
data
also
puts
a
serious
question
mark
on
the
psycho-social
perspective
of
the
consultation
session.
Thus,
it
becomes
imperative
to
analyze
the
nitty-gritty
of
consultation
session.
How
it
can
be
done
effectively?
Are
the
consultation
sessions
really
covering
the
biomedical
as
well
as
psychosocial
perspective
also?
Can
it
be
used
in
training
medical
representatives
for
making
their
interaction
with
doctors
more
fruitful?
Maybe
the
findings
can
bring
some
fruitful
changes
in
the
consultation
session.
This
case
study
is
an
attempt
to
address
these
intriguing
situations.
As
shown
in
the
study
done
by
Fottler
et
al
(2011)
some
patients
also
believe
or
feel
that
hospitals
and
health
care
systems
go
so
far
as
to
regard
them
as
guests
as
stated.
Another
study
conducted
by
Agnieszka
(2012)
also
stated
that
permanent
improvement
in
quality
of
health
care
can
be
enhanced
through
interpersonal
communication
and
it
simultaneously
shapes
the
attitudes
and
behaviours
of
health
(medical)
staff
as
well
as
consumers
of
health
services
(patients).
Epilogue:
These
cases
of
medical
consultation
tried
to
unravel
the
role
of
doctors.
These
can
also
be
used
as
training
materials
for
medical
representatives
as
they
get
to
know
what
exactly
is
happening
in
the
chamber
and
helps
them
in
preparing
themselves
for
their
meeting
with
the
doctors.
All
these
different
observationa
derived
from
medical
consultation
sessions
resulted
in
an
amazing
perspective:
•
Medical
consultations
are
really
meeting
the
criteria
of
fruitful
interaction
level
or
they
are
only
depictions
of
routine
doctor-patient
interaction.
•
Doctors
are
really
practising
the
non-medical
(behavioural/
psychosocial
pattern)
as
well
as
medical
(biomedical)
perspectives
of
medical
consultation
or
are
busy
in
calculating
the
number
of
patients.
•
Doctors
effectively
utilize
the
time
span
of
whole
medical
consultation
session
or
they
are
simply
keeping
track
of
the
number
of
patients
who
have
visited
them.
•
Patient
involvement
in
the
medical
consultation
session
is
required
especially
when
the
disease
falls
into
the
category
of
life
style
diseases
such
as
Cancer,
Diabetes,
Cardiac
diseases.
•
Patient's
outlook
is
to
be
a
treatment
seeker
or
is
an
active
participant
in
the
treatment
schedule.
This
case
study
dealt
with
all
the
phases
mentioned
in
the
Calgary-Cambridge
model
and
also
analyzed
the
biomedical
(medical)
and
psychosocial
(non-medical)
aspects
of
medical
consultation
sessions
but
a
few
issues
are
not
covered.
Details
of
clinical
assessment
and
safety
netting
(ability
of
the
doctor
to
consider
good
or
bad
outcome
of
the
consultation
and
be
ready
with
plan
'B')
are
the
issues
that
have
to
be
explored
more
in
future
studies.
1.
Agnieszka
Macia
G.
Assessment
of
effectiveness
of
the
interpersonal
communication
on
the
doctor-patient
level
in
Poland.
International
Journal
of
Healthcare
Management.
2012;
VOL.5,
NO.2:85-92.
2.
A.Raju.
(2013).
Healthcare
sector
witnessing
major
transition.
www.Pharmabiz.com
3.
Barry
CA
et
al
(2000).
Patients'
unvoiced
agendas
in
general
practice
consultations:
qualitative
study.
British
Medical
Journal
320:1245-50.
4.
Balint
M;
The
doctor,
his
patient
and
the
illness.
Churchill
Livingstone;
First
published
1957,
update
1964.
5.
Deveugele
M,
Derese
A,
De
Bacquer
D,
van
den
Brink-Muinen
A
et
al.
(2004).
Consultation
in
general
practice:
a
standard
operating
procedure?
Patient
Educ
Couns
Aug;54(2):227-33)
6.
Esterling
B.,
Antoni
M.,
Kumar
M.,
Schneiderman
N.(1990).
Emotional
repression,
stress
disclosure
responses
and
Epstein-Barr
viral
capsid
antigen
titers.
Psychosom
Med.
52:397-410.
7.
Francis
J.
Keefe,
Amy
P.
Abernethy,
and
Lisa
C.
Campbell.
Psychological
approaches
to
understanding
and
treating
disease-related
pain.
The
Annual
Review
of
Psychology,
July
13-2004:
617.
8.
Ford,
R.
C,
S.
A.
Bach,
and
M.
D.
Fottler.
(1997).
"Methods
of
Measuring
Patient
Satisfaction
in
Health
Care
Organizations."
Health
Care
Management
Review
22
(2):
74-89.
9.
Fottler,
M.
D.,
R.
C.
Ford,
and
C.
R
Heaton
(2011).
Achieving
Service
Excellence:
Strategies
for
Healthcare,
2nd
edition.
Chicago:
Health
Administration
Press.
10.
Gask
L.,
Usherwood
T.
ABC
of
psychological
medicine:
the
consultation.
BMJ.
2002;
324:1567-
1569.
11.
Howie
JGR
et
al
1992.
Attitudes
to
medical
care,
the
organisation
of
work,
and
work
stress
among
general
practitioners.
British
Journal
of
General
Practice
42:181-185
12.
Jenkins
V,
Fallowfield
L,
Saul
J
2001
Information
needs
of
patients
with
cancer:
results
from
a
large
study
in
UK
cancer
centers.
British
Journal
of
Cancer
84(1):48-51
13.
Kannel
WB,
McGee
D,
Gordon
T.
A
general
cardiovascular
risk
profile:
the
Framingham
study.
Am
J
Cardiol.
1976;
38:46-51.
14.
Kannel
WB,
Neaton
JD,
Wentworth
D,
Thomas
HE,
Stamler
J,
Hulley
SB,
Kjelsberg
MO.
Overall
and
coronary
heart
disease
mortality
rates
in
relation
to
major
risk
factors
in
325,348
men
screened
for
the
MRFIT.
Am
Heart
J.1986;
112:825-836.
15.
Kurtz
S.,
Silverman
J.,
Benson
J.,
Draper
J.
Radcliffe
Medical
Press;
Oxford:
1998.
Teaching
and
learning
communication
skills
in
medicine.
16.
Maguire
P.,
Faulkner
A.,
Booth
K
(1996).
Helping
cancer
patients
disclose
their
concerns.
Eur
J
Cancer;
32a:78-81.
17.
Maguire
P.,
Pitceathly
C.
Clinical
review:
key
communication
skills
and
how
to
acquire
them.
BMJ.
2002;
325:697-700.
18.
Mishler
EG
(1984).
The
discourse
of
medicine,
dialectics
of
medical
interviews.
Ablex
Publishing
Corporation,
Norwood,
NJ.
19.
Ogden
J,
Bavalia
K,
Bull
M,
et
al.
(2004).
"I
want
more
time
with
my
doctor":
a
quantitative
study
of
time
and
the
consultation.
Fam
Pract.
Oct;
21(5):479-83.
20.
Pendleton
D,
Schofield
T,
Tate
P
&
Havelock
P.(1984).
The
Consultation:
An
Approach
to
Learning
and
Teaching:
Oxford:
OUP.
21.
Ridsdale
L,
Morgan
M,
Morris
R
1992
Doctors'
interviewing
technique
and
its
response
to
different
booking
time.
Family
Practice
9:57-60
22.
Roter,
D.,
Rosenbaum,
J.,
Negri,
B.,
Renaud,
D.,
DiPrete-Brown,
L.,
&
Hernandez,
O.(1998).
The
effects
of
a
continuing
medical
education
program
in
interpersonal
communication
skills
on
doctor
practice
and
patient
satisfaction
in
Trinidad
and
Tobago.
Medical
Education,
32,
181-197.
23.
Silverman
J.,
Kurtz
S.,
Draper
J.
2nd
edn.
Radcliffe
Publishing;
Oxford:
2005.
Skills
for
communication
with
patients
24.
Smith
R
(2000).
Thoughts
for
new
medical
students
at
a
new
medical
school.
BMJ.
Dec
20;
327(7429):1430-3.
25.
Subramaniam
I,
Gold
JL.
Diabetes
mellitus
in
elderly:
An
overview.
J
Indian
Academy
Geriatr
2005;
2:77-81.
26.
Tuckett
D,
Boulton
M,
Oban
C,
Williams
A
(1985).
Meetings
between
experts:
an
approach
to
sharing
ideas
in
medical
consultations.
Tavistock
Publications,
London.
27.
Turk
DC.
2002.
Remember
the
distinction
between
malignant
and
benign
pain?
Well,
forget
it.
Clin.
J.
Pain
18(2):75-76.
28.
Waddell
G,
Aylward
M
(2005).The
Scientific
and
Conceptual
Basis
of
Incapacity
Benefits.
London:
TSO.
29.
Waddell
G.,
Aylward
M.
Royal
Society
of
Medicine
Press
Ltd;
London:
2010.
Models
of
sickness
and
disability:
applied
to
common
health
problems.
30.
Zandbelt,
L.
C,
E.
M.
Smets,
F.
I.
Oort,
M.
H.
Codfried,
and
H.
C.
de
Haes.
2007.
"Medical
Specialists'
Patient-Centered
Communication
and
Patient-Reported
Outcomes."
Medical
Care
45
(4):
330-39.
|

