|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................
|
Original
Contribution/Clinical Investigation
|
|

|
<-- Saudi Arabia -->
How Sensitive
is Urine Dipstick Analysis in Predicting Urinary
Tract Infections in Symptomatic Adults in a
Primary Care Setting
[pdf version]
Mokhtar Shatla,
Abdulrahman Almisfer, Shamsuldin Zawawi, Baraah
Damanhouri, Fahad Alharthi
<-- Turkey -->
Accelerated
atherosclerosis and digital clubbing in sickle
cell diseases
[pdf
version]
Mehmet Rami Helvaci, Mustafa Sahan, Agit Sulhan,
Abdullah Fatih Acik, Adil Ocak, Semih Salaz,
Lesley Pocock
<-- UAE/Saudi Arabia -->
Assessment
of home glucose monitoring system in primary
health care system; where are we?
[pdf
version]
Almoutaz Alkhier Ahmed, Amal Nouri
<--Lebanon -->
Cobalamin Injection:
Is it Useful in Lumbosacral Diseases?
[pdf version]
Abdulrazak Abyad
|
|
........................................................ |
Case
Report
........................................................
Continuing Medical
Education
........................................................
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| April 2016 - Volume
14, Issue 3 |
|
|
Assessment of home glucose
monitoring system in primary health care system;
where are we?
Almoutaz
Alkhier Ahmed
(1)
Amal Nouri
(2)
(1) Dr. Almoutaz Alkhier Ahmed , MSc in diabetes,
Pg Dip in diabetes , MRCGP[INT] :
Dubai Health Authority - Nad Alhamar Health
Center, Dubai, UAE
(2) Amal Nouri, Bs in nursing. National Guard
Specialized polyclinics.
National Guard Health Affairs , Jeddah, Saudi
Arabia
Correspondence:
Dr. Almoutaz Alkhier Ahmed , MSc in diabetes,
Pg Dip in diabetes , MRCGP[INT] :
Dubai Health Authority - Nad Alhamar Health
Center, Dubai, UAE
Email: Khier2@yahoo.com
|
Abstract
Introduction:
Self Monitoring Blood Glucose system is
one of the glycemic control assessment
tools. There are many barriers limiting
its proper usage. This system is based
on three components; availability of the
glucometers system, operating skills and
knowledge to interpretate its results.
Objectives:
To assess the components of self monitoring
blood glucose among patients with type
2 diabetes attending primary health care
service and its relation to glycemic control.
Methodology: Cross
sectional study was designed; one hundred
and seventy eight (178; male 72, female
106) were randomly selected from our diabetic
registry. All selected patients had type
2 diabetes. Data was collected through
a designed questionnaire. The three components
of the glucose self monitoring system
were assessed. Selected nurses were trained
to help patients who could not fill out
the questionnaire by themselves. Data
was collected and analyzed by SPSS Vers
14.
Results: One
hundred and seventy eight (178) subjects
; (40.04% male vs 59.56% female). Eighty
eight (88 subjects) were illiterate (49.4%)
and most of them were female (38.9% male
vs 56.6% female). In the male group only
77.7% had glucometers while in the female
group only 52.8% had glucometers (P value
<0.0001). In the male group only 61.1%
knew how to operate the SMBG while only
39.6% of female group could (P value <0.00001).
In the male group only 33.3% stated that
they knew the targets of glucose monitoring
while it was 68.8% in the female group
(P value <0.00001). Only 55.5% of male
subjects had the three components of proper
home glucose self monitoring compared
with 56.1% of female subjects (P value
0.036). Among males with full SMBG components
HbA1c was 9.4(+/-)1.9% and 8.1(+/-)1.7
among females with full SMBG components
(P value 0.002) .
Conclusion: Lack
of proper structured education presented
by educators and illiteracy may explain
the bad glycemic control in our study
sample. Further large studies were recommended.
Key words: Diabetes,
glucose monitoring
|
The measurement technology of measuring real
time blood glucose has passed through many generation
of development. The first self-testing kit for
measuring glucose in urine was developed in
the 1940s. The advent of capillary blood test
strips followed in 1956 and glucose meters in
the 1970s and early 1980s. (1) These advances
facilitated the adoption of self-monitoring
of blood glucose levels as part of the routine
diabetes care especially for those on insulin
therapy.
The self-monitoring blood glucose is one of
the tools used to assess glycemic control and
it can contribute to the control process by
allowing for adjustments in diet, physical activity
and pharmacotherapy in response to test results.
The effect of self monitoring in patients taking
insulin was well established (2) but its effect
on those not on insulin is still controversial
(3) but it is still the standard method for
glucose assessment. Factors such as economic
costs of strips used for tests and patient discomfort
and inconvenience may be some of the limitations
that have decreased the use of this tool.
Literature review showed some systematic reviews
reported marginal advantage of self-monitoring
blood glucose levels in terms of controlling
HbA1c; interestingly these studies usually did
not assess other outcomes such as hypoglycemia,
long-term complications of diabetes or quality
of life. (4-7)
It was very interesting that many studies did
not account for the degree to which participants
were educated on how to interpret and act on
test results of self-monitoring. This is one
of the three components of proper self-monitoring
blood glucose systems, since people using test
strips must be able to act properly in response
to abnormal readings if the system is to be
effective. One systematic review and meta analysis
showed that self monitoring of blood glucose
levels was associated with a modest, statistically
significant reduction in hemoglobin A1c concentration
(weighted mean difference - 0.25% , confidence
interval 0.36% - 0.15%) regardless of whether
patients were provided with education on how
to interpret and use the test results (weighted
mean difference - 0.28% , 95% CI 0.47 - 0.08%)
. (8)
The proper self-glucose monitoring needs the
availability of a glucose measurement device,
skills to operate the device and knowledge to
interpret the results. In our study we try to
find answers whether, these components are available
among our patients and if their presence will
affect glycemic control (HbA1c level).
Cross sectional study was designed .One hundred
and seventy-six (176 subjects) were randomly
selected from the diabetic patient registry.
Only patients with type 2 diabetes who did two
or more HbA1c tests during the year 2014 were
included. We select the one that comes each
with three components .Questionnaire was designed
and distributed to all selected participants
after their verbal acceptance to fill out the
questionnaires. Two nurses were trained to help
participants if they needed help in filling
the questionnaire. Each questionnaire-contained
questions covering the three components of glucose
self-monitoring system; availability of device
system, capability to operate the device system
and knowledge to interpret results. One hundred
and seventy six questionnaires were collected.
Patients' medical records were reviewed and
mean HbA1c for each patient was calculated.
Data was analyzed using SPSS ver 14. One-way
ANOVA test analysis was used to find any statistically
significant differences between means.
We defined high blood glucose as blood glucose
>= 250mg/dl and define low blood glucose
as blood glucose =< 70mg/dl.
One
hundred
and
seventy
eight
(178;
72
male
and
102
female)
subjects
with
type
2
diabetes
were
randomly
selected
with
main
age
56.13(+/-)
12.95
and
mean
HbA1c
8.6(+/-)
2.12
(mean
male
HbA1c
9.76(+/-)
2.05,
female
mean
HbA1c
8.3(+/-)
1.8)
(Table
1).
Table
1:
Bibliography
of
subjects
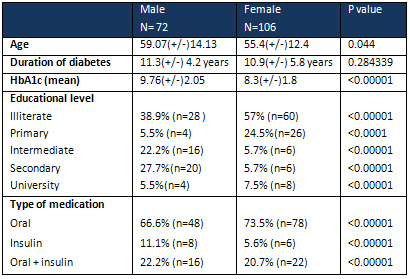
Eighty
eight
(88)
subjects
(50%)
were
illiterate
and
most
of
them
were
female
(57%
female
vs
38.9%
male
P
value
<0.00001)
(Table
1).
Majority
of
our
subjects
receive
oral
hypoglycemic
medication
(71.6%;
male
66.6%
while
female
73.5%
P
value
<0.00001)
(Table
1).
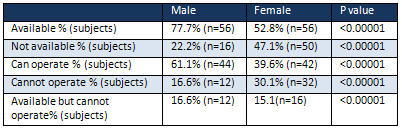
In
the
male
group
only
56
subjects
had
glucometers
while
16
subjects
had
not
(77.7%
vs
22.2%,
P
value
<0.00001).
In
female
group
56
subjects
had
glucometers
while
56
had
not
(52.8%
vs
47.1%,
P
value
<0.0001)
(Table
2).
It
was
interesting
to
notice
that
44
male
subjects
could
operate
their
glucometers
while
12
could
not
(61.1%
vs
16.6%,
P
value
<0.00001).
In
the
female
group,
42
of
subjects
could
operate
their
glucometers
while
32
could
not
(39.6%
vs
30.1%,
P
value
0.00001)
(Table
2).
In
the
male
group
we
noticed
12
patients
had
glucometers
but
they
cannot
operate
them
while
in
the
female
group
we
found
16
subjects
had
glucometers
but
they
could
not
operate
them
(16.6%
vs
15.1%
,
P
value
<0.00001)
(Table
2)
(Figure
1).
Table
2:
Availability
of
glucometers
and
operation
skills
Figure
1:
Components
of
SMBG
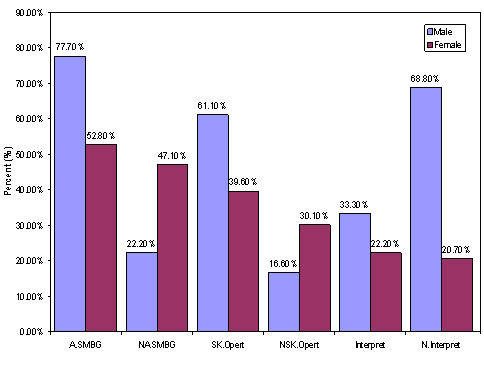
A.SMBG
=
Availability
of
self-monitoring
blood
glucose
NA.SMBG
=
No
availability
of
self-monitoring
blood
glucose
SK.Opert
=
Skills
to
operate
glucometer
NSK-Opert
=
No
Skills
to
operate
glucometer
Interpret
=
interpretation
glucometer
result
N.Interpret
=
No
interpretation
glucometer
result
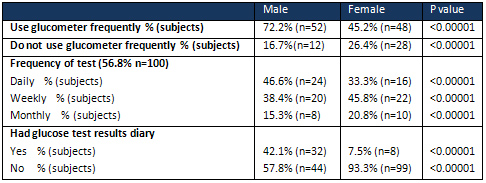
In
the
male
group
52
subjects
use
their
glucometers
frequently
at
home
while
12
subjects
did
not
(72.2%
vs
16.7%
,P
value
<0.00001).
In
the
female
group
48
subjects
did
frequent
use
of
their
glucometers
while
28
subjects
did
not
(45.2%
vs
26.4%
,P
value
<0.00001)
(Table
3).
It
was
very
interesting
to
note
that
only
32
male
subjects
had
a
glucose
test
results
diary
while
only
8
females
had
(42.1%
vs
7.5%
,
P
value
<0.00001).
Table
3:
Frequency
of
glucose
test
at
home
In
the
male
group
only
24
subjects
stated
that
they
knew
the
targets
of
glucose
monitoring
while
20
subjects
stated
they
did
not
know
(33.3%
vs
22.2%
,
P
value
<0.00001)
(Table
4).
In
the
female
group
74
stated
they
knew
the
targets
while
22
did
not
(68.8%
vs
20.7%,
P
value
<0.00001)
(Table
4).
Table
4:
Knowledge
of
glucose
targets
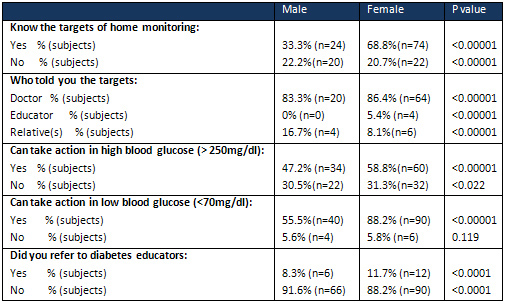
Only
24
male
subjects
can
take
action
in
case
of
high
blood
glucose
results
(>
250mg/dl)
while
12
stated
they
did
not
know
what
to
do
(47.2%
vs
30.5%
,
P
value
<0.00001).
In
the
female
group
60
subjects
can
take
action
while
32
subjects
did
not
know
what
to
do
(58.8%
vs
31.3%
,
P
value
<0.00001)
(Table
4).
When
we
compared
the
male
group
to
female
group
,we
found
that
47.2%
male
vs
58.8%
female
can
take
action
if
their
blood
glucose
>
250mg/dl
(P
value
0.00001)
In
case
of
low
blood
glucose
(<
70mg/dl),
50
male
subjects
can
take
action
and
only
14
did
not
know
(55.5%
vs
5.6%,
P
value
<0.00001).
In
the
female
group
90
subjects
can
take
action
while
six
subjects
cannot
take
action
(88.2%
vs
5.8%,
P
value
<0.00001)
(Table
4).
When
we
compared
the
male
group
to
female
group,
we
found
that
55.5%
male
vs
88.2%
female
can
take
action
if
their
blood
glucose
<70mg/dl
(P
value
0.00001).
Only
40
male
subjects
had
the
three
components
of
proper
home
glucose
self
monitoring
while
60
female
subjects
had
them
(55.5%
vs
56.5%,
P
value
0.036)
(Table
5).
Table
5:
Subjects
who
had
all
components
of
home
glucose
self
monitoring
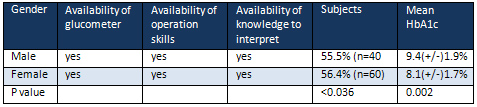
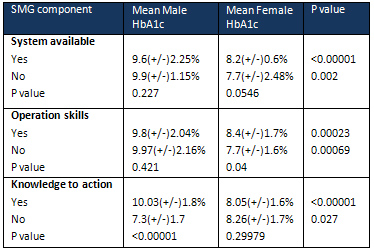
Table
6
explains
the
relation
between
the
components
of
SMBG
and
glycemic
control
among
male
and
female
groups.
The
differences
were
statistically
different
between
male
and
female
groups.
Neither
component
was
associated
with
good
glycemic
control
(mean
HbA1c
<7%).
Table
6:
Relation
of
SMG
components
to
HbA1c
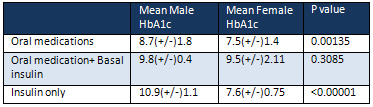
In
(Table
7)
we
discussed
the
relation
between
those
with
full
SMBG
components
and
the
type
of
medication
they
received.
Interestingly
HbA1c
was
7.6(+/-)
0.75
among
females
with
full
SMBG
components
treated
with
insulin
in
comparison
with
10.9
(+/-)
1.1
in
the
male
group
(P
value
<0.00001)
and
there
is
no
statistically
difference
between
male
and
female
groups
with
full
SMBG
monitoring
components
treated
with
oral
medication
plus
basal
insulin
(HbA1c
9.8(+/-)
0.4
vs
9.5(+/-)2.11
,
P
value
0.3085).
Table
7:
Comparison
between
subjects
with
full
SMBG
based
on
their
type
of
treatment
In
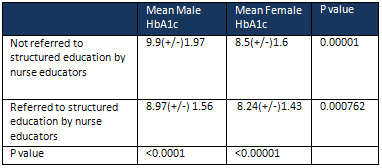
(Table
8)
we
discussed
the
effect
of
referral
to
structured
diabetes
education.
Interestingly,
our
results
showed
that
there
is
no
effect
of
referral
to
structured
education
programs
by
nurse
educators
on
bringing
HbA1c
towards
the
target
(<7%)
.
Interestingly
there
is
statistical
difference
between
male
and
female
groups
who
either
referred
or
not
referred;
those
not
referred
(9.9(+/-)1,97
vs
8.5(+/-)1.6
,
P
value
0.00001)
and
those
referred
(8.97(+/-)1.56
vs
8.24(+/-)1.43
,P
value
0.000762).
When
we
compared
male
to
male
not
referred
to
referred
the
difference
was
statistically
significant
(9.9(+/-)1.97
vs
8.97(+/-)1.56
,P
value
<
0.0001)
and
female
to
female
also
the
difference
was
found
to
be
statistically
significant
(8.5(+/-)
1.6
vs
8.24(+/-)1.43
,
P
value
<0.00001);
but
all
did
not
drop
to
the
target
level
(<7%).
Table
8:
Relation
between
mean
HbA1c
and
referred
patients
to
structured
education
by
nurse
educators
among
all
subjects
In
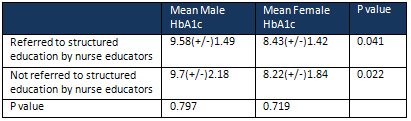
(Table
9)
we
compared
those
with
full
component
of
SMBG
regarding
referral
or
not
referral
to
structured
training
programs
by
nurse
educators.
Among
those
who
referred,
there
is
statistically
significant
difference
(male
mean
HbA1c
9.58(+/-)
1.49
vs
female
mean
HbA1c
8.43(+/-)
1.42,
P
value
0.041).
Interestingly
it
was
not
a
statistically
significantly
difference
when
we
compared
the
same
gender
groups;
male
group
(mean
HbA1c
9.58(+/-)
1.49
vs
9.7(+/-)
2.18,
P
value
0.797)
vs
female
group
(mean
HbA1c
8.43(+/-)
1.42
vs
8.22
(+/-)
1.84,
P
value
0.719).
Table
9:
Relation
between
referral
to
structured
education
by
educators
and
mean
HbA1c
in
subjects
with
full
SMBG
components
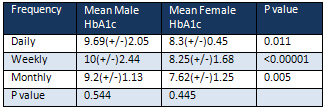
In
(Table
10)
we
showed
comparison
between
those
with
full
SMBG
components
regarding
their
frequency
of
SMBG
use
and
their
mean
HbA1c.
Results
showed
that
there
are
no
statistically
significant
differences
in
male
or
female
groups
regarding
the
frequency
of
use
and
HbA1c;
in
male
group
daily,
weekly
and
monthly
frequency
of
test
showed
HbA1c
9.69(+/-)
2.05,
10(+/-)
2.44
and
9.2(+/-)
1.13
respectively
with
P
value
0.544.
While
in
the
female
group,
it
was
8.3(+/-)
0.45,
8.25(+/-)
1.68
and
7.62(+/)
1.25
with
P
value
0.445.
When
we
compared
male
to
female
groups
it
was
significantly
statistically
different
for
daily,
weekly
and
monthly
frequency
(P
value
0.001
,P
value
<00001
and
P
value
0.005).
Table
10
:
Relation
with
full
SMBG
components
and
frequency
of
SMBG
to
mean
HbA1c
Diabetes
mellitus
is
a
chronic
disease
that
necessitates
continuing
treatment
and
patient
self-care
education.
Monitoring
of
blood
glucose
to
near
normal
level
without
hypoglycemia
becomes
a
challenge
in
the
management
of
diabetes.
The
global
prevalence
of
diabetes
by
International
Diabetes
Federation
(IDF)
estimation
shows
that
there
are
366
million
people
with
diabetes
in
2011,
and
this
is
expected
to
rise
to
552
million
by
2030.
(9)
Self-monitoring
of
blood
glucose
(SMBG)
has
been
shown
to
be
as
effective
in
insulin-treated
type
1
and
type
2
diabetes.
Although
the
effect
of
SMBG
is
already
demonstrated
in
some
meta-analysis
(10-11),
it
is
not
recommended
as
regular
use
in
non-insulin
treated
type
2
diabetes.
SMBG
fails
to
detect
nocturnal
hypoglycemia
and
asymptomatic
hypoglycemia
even
in
patients
with
good
control
of
HbA1c
values
and
it
needs
multiple
blood
samples
throughout
the
day.
In
addition,
SMBG
gives
a
single
instant
reading
without
any
information
on
glucose
trends
and
thus
may
miss
important
and
significant
glucose
fluctuations.
(12-14)
In
our
study,
we
tried
to
answer
some
questions
related
to
SMBG.
Firstly,
we
raised
the
question
whether
the
availability
of
a
SMBG
system
will
affect
the
glycemic
control.
Our
results
showed
that
availability
of
the
system
did
not
lead
to
good
glycemic
control
either
among
male
or
female
groups.
The
mean
HbA1c
during
the
year
2014
did
not
drop
to
below
7%,
which
we
considered
as
good
glycemic
control,
but
it
was
much
better
among
the
female
group
who
had
a
SMBG
system
(8.2
(+/-)
0.6%
vs
9.6(+/-)
2.25%,
P
value
0.00001).
In
a
randomized
control
trial
done
by
Wing
RR
et
al
(15)
the
authors
also
found
no
statistical
difference
in
HbA1c
between
those
who
had
SMBG
or
not.
Interestingly
this
study
was
done
among
patients
treated
with
insulin.
On
the
other
hand,
another
randomized
clinical
trial
(16)
in
subjects
treated
with
insulin
reached
a
conclusion
that
presence
of
SMBG
significantly
improved
HbA1c.
Guerci
et
al
in
their
randomized
control
trial
(17)
concluded
that
availability
of
a
SMBG
system
significantly
improved
HbA1c
while
Davidson
et
al
(18)
did
not
find
any
statistically
difference
in
HbA1c.
Interestingly
Guerci
et
al
was
a
large
trial
that
included
689
participants
while
Davidson
et
al's
trial
included
88
participants.
In
sub
analysis
of
our
participants
we
noticed
that
females
with
SMBG
system
treated
with
insulin
have
better
mean
HbA1c
than
the
male
group
treated
with
insulin
(7.6(+/-)0.75
vs
10(+/-)1.1
,
P
value
<0.00001)
.
When
we
work
to
find
an
explanation
for
this
result
we
noticed
that
compliance
to
insulin
therapy
was
better
among
female
subjects
treated
with
insulin
than
male
subjects
treated
with
insulin
(P
value
<0.00001).
Then
we
raised
a
second
question
whether
the
capability
to
operate
the
SMBG
will
affect
glycemic
control?
Our
results
showed
that
these
skills
did
not
take
participants
to
good
glycemic
control
whether
they
are
male
or
female
(
mean
HbA1c
9.8(+/-)2.04
vs
8.4(+/-)1.7
,
P
value
0.00023),
but
when
skills
are
available
with
other
components
mean
HbA1c
improved
(male
mean
HbA1c
9.4(+/-)1.9
vs
female
mean
HbA1c
8.1(+/-)1.7
,
P
value
0.002).
Brendan
M
et
al
(19)
found
in
their
systematic
review
and
meta
analysis
that
provided
patients
with
education
on
how
to
interpret
and
apply
SMBG
system,
results
were
similar
to
those
from
RCTs
that
did
not.
Our
third
question
was
whether
diabetes
education
presented
by
diabetes
educators
was
affective
in
glycemic
control.
Our
results
showed
that
only
10.5%
(18
subjects)
were
referred
to
diabetes
educators
for
a
structured
diabetes
education
program.
Among
those
who
were
referred,
the
male
group
mean
HbA1c
was
8.97(+/-)1.56
while
in
female
group
mean
HbA1c
was
8.24(+/-)1.43
with
statistically
significant
difference
between
the
two
groups
(P
value
0.000762).
In
subjects
who
were
not
referred
to
the
structured
education
program
by
nurse
educator
the
results
showed
a
statistically
significant
difference
between
male
and
female
groups
(9.9(+/-)
1.97
vs
8.5(+/-)
1.6,
P
value
0.00001)
with
better
mean
HbA1c
in
the
female
group.
This
finding
can
be
explained
by
that
female
patients
were
more
adherent
to
educational
data
and
advice.
Female
patients
usually
implement
more
what
they
learn
from
educational
sessions
to
their
daily
life,
than
male
patients.
When
we
do
sub-analysis
no
those
who
have
the
full
components
of
appropriate
SMBG
and
look
to
their
mean
HbA1c
based
on
their
referral
or
not
referral
to
structured
diabetes
program,
we
found
that
mean
HbA1c
dropped
more
in
the
male
group.
It
was
9.58(+/-)1.49
vs
8.97(+/-)1.56
P
value
0.00001).
Interestingly
it
was
not
improved
in
the
female
group
(8.24(+/-)1.43
vs
8.43(+/-)1.42,
P
value
0.382).
This
data
can
be
explained
by
that
female
patients
with
full
components
of
SMBG
were
more
reliant
on
the
system
itself
and
did
not
think
that
they
need
multiple
structured
education
sessions.
Also
the
power
of
culture
and
the
restriction
on
female
movement
in
the
community
forces
those
with
full
components
to
hold
any
participation
in
such
continuous
education
programs
as
long
as
they
have
the
components.
Among
male
patients,
the
presence
of
full
components
of
SMBG
was
a
motivation
to
join
a
structured
educational
program,
which
reflected
positively
on
their
mean
HbA1c
(Table
8-9).
Then
we
ask
ourself
if
the
frequency
of
SMBG
among
those
with
full
criteria
of
appropriate
SMBG
affected
their
mean
HbA1c?
Our
results
showed
no
statistically
significant
difference
between
male
to
male
and
female
to
female
groups
who
did
tests
on
a
daily
base,
weekly
base
and
monthly
base
(P
value
0.544
vs
P
value
0.445),
but
when
we
compared
male
to
female
groups,
the
difference
was
statistically
significant
(daily
base,
weekly
base
and
monthly
base
with
correspondent
P
values
0.005,
<0.00001
and
0.11)
(Table
10).
We
did
not
find
an
effect
on
frequency
of
SMBG
and
mean
HbA1
in
patients
receiving
oral,
oral
plus
insulin
or
insulin
only.
Schutt
M
et
al
(20)
did
not
find
effect
of
frequency
of
SMBG
and
level
of
HbA1c
among
patients
on
oral
anti-hyperglycemic
medications
but
they
found
effect
among
those
who
use
insulin.
The
use
of
SMBG
in
patients
with
type
2
diabetes
is
a
complex
issue
with
no
clear
findings
supporting
clear
recommendations.
There
are
many
papers
that
support
its
use
in
patients
with
type
2
diabetes
mellitus
especially
in
the
first
year
of
diabetes
where
its
significance
starts
to
decline
after
12
months.
On
the
other
hand,
there
are
studies
that
concluded
on
not
to
use
SMBG
in
patients
with
type
2
diabetes
due
to
insignificant
effect
on
glycemic
control
indicators
such
as
HbA1c
as
well
as
the
cost
of
these
systems.
In
our
opinion,
the
SMBG
when
individually
recommended
to
selected
patients
such
as
type
2
patients
on
insulin
or
with
add
on
insulin
or
on
their
first
year
after
diagnosis
will
help
these
patients
very
well
to
improve
their
HbA1c
and
the
long
term
metabolic
complications.
(21)
Acknowledgement:
The
author
would
like
to
thank
Mrs.
Mayada
Abubakr
Alsaeed
for
her
valuable
help
in
editing
and
organizing
this
study.
Abbreviations:
SMBG
=
Self
Monitoring
Blood
Glucose
HbA1c
=
Glycated
Haemoglobin
1)
Sonia
Butalia
and
Doreen
M
Rabi.
To
test
or
not
to
test?
Self
-monitoring
of
blood
glucose
in
patients
with
type
2
diabetes
managed
without
insulin
.
Open
Medicine
2010;4(2):
14-16
2)
Canadian
Diabetes
Association
2008
clinical
practice
guidelines
for
the
prevention
and
management
of
diabetes
in
Canada.
Can
J
Diabetes
2008;32
(Suppl
1):S1-S201.
3)
Davidson
MB,
Castellanos
M,
Kain
D,
Duran
P.
The
effect
of
self
monitoring
of
blood
glucose
concentrations
on
glycated
hemoglobin
levels
in
diabetic
patients
not
taking
insulin:
a
blinded,
randomized
trial.
Am
J
Med
2005;118(4):422-425.
4)
Towfigh
A,
Romanova
M,
Weinreb
JE,
Munjas
B,
Suttorp
MJ,
Zhou
A,
et
al.
Self-monitoring
of
blood
glucose
levels
in
patients
with
type
2
diabetes
mellitus
not
taking
insulin:
a
meta-analysis.
Am
J
Manag
Care
2008;14(7):468-475.
5)
Sarol
JN,
Nicodemus
NA,
Tan
KM,
Grava
MB.
Self-monitoring
of
blood
glucose
as
part
of
a
multi-component
therapy
among
non-insulin
requiring
type
2
diabetes
patients:
a
meta-analysis
(1966-2004).
Curr
Med
Res
Opin
2005;21(2):173-183.
6)
Poolsup
N,
Suksomboon
N,
Jiamsathit
W.
Systematic
review
of
the
benefits
of
self-monitoring
of
blood
glucose
on
glycemic
control
in
type
2
diabetes
patients.
Diabetes
Technol
Ther
2008;10(Suppl
1):S51-S66.
7)
McGeoch
G,
Derry
S,
Moore
RA.
Self-monitoring
of
blood
glucose
in
type-2
diabetes:
What
is
the
evidence?
Diabetes
Metab
Res
Rev
2007;23(6):423-
440.
8)
McIntosh
B,
Yu
C,
Lal
A,
Chelak
K,
Cameron
C,
Singh
SR,
Dahl
M.
Efficacy
of
self-monitoring
of
blood
glucose
in
patients
with
type
2
diabetes
mellitus
managed
without
insulin:
a
systematic
review
and
meta-analysis.
Open
Med
2010;4(2):e102-13.
9)
Whiting
DR,
Guariguata
L,
Weil
C,
Shaw
J:
IDF
diabetes
atlas:
global
estimates
of
the
prevalence
of
diabetes
for
2011
and
2030.
Diabetes
Res
Clin
Pract
2011,
94(3):311-321.
10)
Sarol
JN,
Nicodemus
NA,
Tan
KM,
Grava
MB:
Self-monitoring
of
blood
glucose
as
part
of
a
multi-component
therapy
among
non-insulin
requiring
type
2
diabetes
patients:
a
meta-analysis
(1996-2004).
Curr
Med
Res
Opin
2005,
21(2):173-184.
11)
Poolsup
N,
Suksomboon
N,
Rattanasookchit
S:
Meta-analysis
of
the
benefits
of
self-monitoring
of
blood
glucose
on
glycemic
control
in
type
2
diabetes
patients:
An
update.
Diabetes
Techno
Ther
2009,
11(12):775-782.
12)
Weber
KK,
Lohmann
T,
Busch
K,
Donati-Hirsch
I,
Riel
R:
High
frequency
of
unrecognized
hypoglycaemias
in
patients
with
type
2
diabetes
is
discovered
by
continuous
glucose
monitoring.
Exp
Clin
Endocrinol
Diabetes
2007,
115:491-494.
13)
Boland
E,
Monsod
T,
Delucia
M,
et
al:
Limitations
of
conventional
methods
of
self-monitoring
of
blood
glucose:
lessons
learned
from
3
days
of
continuous
glucose
sensing
in
pediatric
patients
with
type
1
diabetes.
Diabetes
Care
2001,
24(11):1858-1862.
14)
MacGowan
K,
Thomas
W,
Moran
A:
Spurious
reporting
of
nocturnal
hypoglycemia
by
CGMS
in
patients
with
tightly
controlled
type
1
diabetes.
Diabetes
Care
2002,
25(9):1499-1503.
15)
Wing
RR,
Epstein
LH,
Nowalk
MP,
Scott
N,
Koeske
R,
Hagg
S.
Does
self-monitoring
of
blood
glucose
levels
improve
dietary
compliance
for
obese
patients
with
type
II
diabetes?
Am
J
Med.
1986;81:830-836.
16)
Kwon
HS,
Cho
JH,
Kim
HS,
et
al.
Establishment
of
blood
glucose
monitoring
system
using
the
Internet.
Diabetes
Care.
2004;27:478-483.
17)
Schwedes
U,
Siebolds
M,
Mertes
G;
SMBG
Study
Group.
Meal-related
structured
self-monitoring
of
blood
glucose:
effect
on
diabetes
control
in
noninsulin-
treated
type
2
diabetic
patients.
Diabetes
Care.
2002;25:1928-1932
18)
Guerci
B,
Drouin
P,
Grange
V,
et
al.
Selfmonitoring
of
blood
glucose
significantly
improves
metabolic
control
in
patients
with
type
2
diabetes
mellitus
control
in
patients
with
type
2
diabetes.
Diabetes
Care.
2002;25:245-246.
19)
Brendan
McIntosh,
Changhua
Yu,
Avtar
Lal,
Krisen
Chelak,
Chris
Cameron,
Sumeet
R
Singh,
Marshall
Dahl.
Efficacy
of
self
-
monitoring
of
blood
glucose
in
patients
with
type
2
diabetes
mellitus
managed
without
insulin
:
a
systematic
review
and
meta
-
analysis.
Open
Medicine
2010;4(2):102-113
20)
Schutt
m,
Kern
W,
Krause
U,
Busch
P,
Dapp
A
,
Grziwtz
R
et
al
.
Is
the
frequency
of
self-monitoring
of
blood
glucose
related
to
long-term
metabolic
control?
Multicenter
analysis
including
24,500
patients
from
191
centers
in
Germany
and
Austria.
Exp
Clin
Endocrinol
Diabetes.
2006
Jul;114(7):384-8.
21)
Ahmed
AA.
Glycemic
control
in
diabetes.
Oman
Med
J.
2010
Jul;25(3):232-3
|
|
.................................................................................................................

|
| |
|

