The
study
was
performed
in
the
Abyad
Medical
Center,
a
model
multispeciality
group
with
15,000
thousand
registered
patients.
The
group
is
located
in
the
North
of
Lebanon.
The
mean
age
of
the
patients
was
55
years.
Fourty
percent
of
the
patients
were
male.
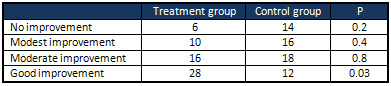
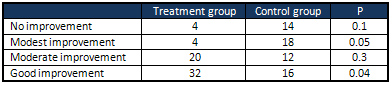
Both
treatment
groups
noted
a
marked
improvement
(Table
1).
Howver
good
improvement
was
statistically
more
significant
in
the
treatment
group.
Table
1:
Global
Result
treatment
as
reported
by
patients
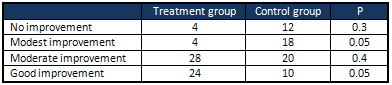
Both
the
treatment
and
placebo
group
reported
decrease
in
spontaneous
pain
(Table
2).
Again
both
moderate
and
good
improvement
was
statistically
more
significant
in
the
active
treatment
group.
Table
2:
Spontaneous
Pain
as
reported
by
patients
at
the
end
of
treatment
period
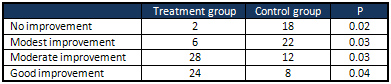
As
for
pain
provoked
by
movement
the
treatment
group
was
statistically
better
on
the
moderate
and
good
improvement
category
(Table
3).
Table
3:
Pain
provoked
by
movement
as
reported
by
patients
at
the
end
of
treatment
period
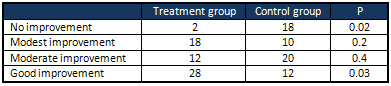
The
comaprison
of
the
group
at
the
end
of
treatment
period
revealed
that
nocturnal
pain
showed
a
statistical
significant
difference
in
favor
of
the
active
treatment
(Table
4).
Table
4:
Nocturnal
Pain
as
reported
by
patients
at
the
end
of
treatment
period
At
the
end
of
treatment
both
the
control
and
treatment
group
report
a
reduction
in
nocturnal
paraesthesia
(Table
5).
Table
5:
Nocturnal
Paraesthesia
as
reported
by
patients
at
the
end
of
treatment
period
Mean
consumption
of
paracetamol
was
significantly
higher
in
the
placebo
group
than
in
the
active
treatment
group
(45.7+-10.32
vs
14
+-9/21
days;
p<0.0001).
Fifteen
patients
in
the
treatment
group
did
not
take
any
paracetamol
tablets
vs
only
2
subjects
in
the
placebo
groups.
Safety
was
good
in
both
groups.
No
change
in
their
medical
conditions,
vital
signs,
nor
any
adverse
effects
at
the
end
of
treatment.
Chronic
pain
is
a
usual
complaint,
leading
the
sufferer
to
be
up
to
five
times
more
likely
to
pursue
medical
attention
as
compared
to
those
people
without
chronic
pain
(10).
Lumbago,
is
a
main
cause
of
chronic
pain.
Within
a
year
period
one
third
of
patients
with
this
pain
will
experience
lumbago
(11).
It
has
also
been
projected
that
around
80%
of
people
will
have
low
back
pain
at
some
point
during
their
life
(12).
The
bulk
of
low
back
pain
(90%)
without
related
neurological
symptoms
improves
within
3
months
(13).
The
remaining
10%
are
a
challenge
to
many
healthcare
providers,
not
only
because
chronic
low
back
pain
is
challenging
to
manage,
and
normally
linked
to
anxiety,
depression,
job
dissatisfaction,
poor
body
image
and
somatization
(11).
Back
pain
is
one
of
the
most
frequent
health
complaints.
It
is
a
common
complaint
affecting
70-85%
of
people
worldwide
at
some
point
during
their
life
(14).
The
differential
is
extensive
including
cancer,
infection,
inflammatory
disorders,
structural
disorders
of
the
spine
itself
and
disk
herniation,
are
somewhat
more
common,
and
together
account
for
back
pain.
According
to
the
WHO
(World
Health
Organization),
low
back
pain
leads
to
a
high
economic
burden
due
to
the
effects
this
often
chronic
problem
has
on
work
productivity
(15).
It
is
one
of
the
most
frequent
causes
behind
visiting
a
primary
care
provider,
and
in
the
top
five
of
the
most
common
reasons
for
having
surgery(12).
Initially,
low
back
pain
is
usually
managed
with
anti-inflammatories
including
non-steroidal,
muscle
relaxants,
and
narcotics.
Persistent
back
pain
is
further
treated
with
physical
therapy,
TENS
units,
massage,
epidural
steroid
injections,
and
surgery.
Treatment
varies
depending
on
the
patient.
The
majority
of
patients
recover
within
12
weeks,
while
10
to
20%
endure
low
back
pain
past
this
time
period,
even
with
treatment
(11,12).
It
emerges
that
vitamin
B12
might
be
one
of
those
additional
treatment
options.
This
study
clearly
showed
the
beneficial
effects
of
the
vitamin
in
low
back
pain.
The
advantage
of
using
B12
shots
included
decreasing
the
amount
of
non-steroidal
anti-inflammatory
drugs
(NSAID),
such
as
aspirin
and
ibuprofen.
Vitamin
B12
has
no
known
side
effects,
according
to
the
National
Institutes
of
Health
Office
of
Dietary
Supplements,
rivaled
to
long-term
NSAID
use,
which
may
harm
the
gastrointestinal
system
and
probably
lead
to
heart
attacks
and
strokes.
Vitamin
B12
helps
nerves
repair
and
regenerate
in
the
back.
Additional
benefits
to
treating
back
pain
with
B12
shots
include
the
vitamin's
low
cost,
minimal
side
effects,
and
ability
to
get
patients
back
to
work
and
enjoying
their
lives.
Studies
have
shown
that
vitamin
B12
shots
can
successfully
decrease
back
pain
(16,17).
One
study
conducted
in
2000
by
Italian
researchers
at
the
University
of
Palermo
found
that
vitamin
B12
helped
to
alleviate
lower
back
pain.
The
study
evaluated
60
patients
aged
between
18
and
65
with
proven
back
pain
lasting
anywhere
from
six
months
to
five
years.
Study
participants
were
divided
into
two
groups
and
received
either
a
B12
shot
or
a
placebo.
Results
showed
injections
alleviated
back
pain
in
patients
even
if
they
entered
the
study
with
adequate
blood
levels
of
vitamin
B12
(17).
The
therapeutic
options
for
low
back
pain
include
NSAIDs,
tramadol
acetaminophen
combinations,
non-SSRI
antidepressants,
and
glucocorticoids
or
local
anesthetic
to
the
spine
(18).
These
medications
may
lead
to
serious
side
effects,
particularly
when
used
for
a
long
time.
NSAIDS,
for
example
can
lead
to
kidney
dysfunction,
acetaminophen
can
cause
liver
dysfunction
and
glucocorticoids
can
cause
weight
gain,
insomnia,
and
Cushing
syndrome.
Studies
revealed
that
out
of
the
available
treatments
only
NSAIDs
seem
to
ameliorate
function
(18).
Recent
studies
including
this
study
(16,17)
have
shown
that
injectable
cobalamin
might
also
be
a
promising
treatment
option
for
lumbago.
Several
studies
(19-25),
have
suggested
that
large
doses
of
vitamin
B12
in
combination
with
NSAIDs
may
lead
to
heightening
effect
on
the
analgesic
properties
of
NSAIDs,
therefore
possibly
decreasing
NSAID
dosing.
Vitamin
B12
is
mostly
used
for
treatment
of
deficiency,
which
is
often
due
to
malabsorption,
insufficient
dietary
intake,
pernicious
anemia,
gastric
surgery,
GI
disease,
and
particular
medications
(26).
If
long
term
effects
of
vitamin
B12
injection
show
to
be
safe,
vitamin
B12
might
be
a
precious
treatment
alternative
for
low
back
pain.
This
will
be
particularly
important
for
the
elderly,
for
patients
prone
to
liver
or
kidney
disease
or
people
interested
in
natural
substances.
This
study
revealed
that
vitamin
B12
compared
to
placebo,
decreases
low
back
pain
and
improves
function
significantly.
However
there
are
certain
limitations,
including
small
size
that
leads
to
large
confidence
intervals
that
the
possibility
that
treatment
effect
was
not
precise.
In
addition
none
of
the
studies
investigated
the
long
term
effects
of
injectable
vitamin
B12.
Although
vitamin
B12
seems
to
have
significant
benefit
in
the
treatment
of
chronic
low
back
pain,
further
research,
with
elimination
of
some
of
these
limiting
factors,
is
needed
to
study
whether
the
intramuscular
vitamin
B12
injection
doses
are
indeed
harmful
in
the
long
run.
Intramuscular
vitamin
B12
injections
seem
to
be
effective
at
ameliorating
nonspecific
chronic
low
back
pain
as
compared
to
placebo.
Vitamin
B12
injections
also
have
exhibited
only
minimal
side
effects,
which
include
hematoma
and
pain
at
the
injection
site.
There
is
a
need
for
a
larger
study
with
longer
duration
that
spans
several
years
to
assess
the
long
term
side
effects,
especially
that
long
term
effects
can
be
possibly
serious.
1.
Patel
MS,
Rasul
Z,
Sell
P.
Dual
pathology
as
a
result
of
spinal
stenosis
and
vitaminB12
deficiency.
Eur
Spine
J.
2011;20:
2247-2251.
2.
L.
R.
McDowell,
Vitamins
in
Animal
and
Human
Nutrition,
John
Wiley
&
Sons,
2008.
3.
R.
Banerjee
and
S.
W.
Ragsdale,
"The
many
faces
of
vitamin
B12:
catalysis
by
cobalamin-dependent
enzymes,"
Annual
Review
of
Biochemistry,
vol.
72,
pp.
209-247,
2003.
4.
S.
K.
Ghosh,
N.
Rawal,
S.
K.
Syed,
W.
K.
Paik,
and
S.
D.
Kim,
"Enzymic
methylation
of
myelin
basic
protein
in
myelin,"
Biochemical
Journal,
vol.
275,
part
2,
pp.
381-387,
1991.
5.
A.
Pfohl-Leszkowicz,
G.
Keith,
and
G.
Dirheimer,
"Effect
of
cobalamin
derivatives
on
in
vitro
enzymatic
DNA
methylation:
methylcobalamin
can
act
as
a
methyl
donor,"
Biochemistry,
vol.
30,
no.
32,
pp.
8045-8051,
1991.
6.
J.
I.
Toohey,
"Vitamin
B12
and
methionine
synthesis:
a
critical
review.
Is
nature's
most
beautiful
cofactor
misunderstood?"
BioFactors,
vol.
26,
no.
1,
pp.
45-57,
2006.
7.
Bruggemann
G,
Koehler
CO,
Koch
EM.
Results
of
a
double-blind
study
of
diclofenac
+vitamin
B1,
B6,
B12
versus
diclofenac
in
patients
with
acute
pain
of
the
lumbar
vertebrae.
A
multicenter
study.
Klin
Wochenschr.
1990;68:116-20.
8.
Kuhlwein
A,
Meyer
HJ,
Koehler
CO.
Reduced
diclofenac
administration
by
B
vitamins:
results
of
a
randomized
double
blind
study
with
reduced
daily
doses
of
diclofenac
(75
mg
diclofenac
versus
75
mg
diclofenac
plus
B
vitamins)
in
acute
lumbar
vertebral
syndrome.
Klin
Wochenschr.
1990;68:107-15.
9.
Vetter
G,
Bruggemann
G,
Lettko
M,
et
al.
Shortnening
diclofenac
therapy
by
B
vitamins.
Results
of
a
randomized
double
blind
study,
diclofenac
50
mg
versus
diclofenac
50
mg
plus
B
vitamins,
in
painful
spinal
diseases
with
degenerative
changes.
Z
Rheumatol.
1988;47:351-62.
10.
A.
McCaddon
and
P.
R.
Hudson,
"L-methylfolate,
methylcobalamin,
and
N-acetylcysteine
in
the
treatment
of
Alzheimer's
disease-related
cognitive
decline,"
CNS
Spectrums,
vol.
15,
supplement
1,
no.
1,
pp.
2-6,
2010
11.
Hoy
D,
Brooks
P,
Blyth
F,
Buchbinder
R.
The
epidemiology
of
low
back
pain.
Best
Practice
&
Research
Clinical
Rheumatology.
2010;24:769-781.
12.
World
Health
Organization.
Low
Back
Pain.
http://www.who.int/medicines/areas/priority_medicines/BP6_24LBP.pdf?ua=1.
Updated
March
2013.
Accessed
March
19,
2014.
13.
Wheeler
SG,
Wipf
JE,
Staiger
TO,
Deyo
RA.
Approach
to
the
diagnosis
and
evaluation
of
low
back
pain
in
adults.
In:
UpToDate,
Atlas
SJ
(Ed),
UpToDate,
Waltham,
MA,
2014.
14.
J.
W.
Frymoyer,
"Back
pain
and
sciatica,"
The
New
England
Journal
of
Medicine,
vol.
318,
no.
5,
pp.
291-300,
1988.
15.
Andersson
GBJ.
Epidemiological
features
of
chronic
low
back
pain.
Lancet.
1999;354:581-85.
16.
Chiu
CK,
Low
TH,
Tey
YS,
Singh
VA,
Shong
HK.
The
efficacy
and
safety
of
intramuscular
injections
of
methylcobalamin
in
patients
with
chronic
nonspecific
low
back
pain:
a
randomized
controlled
trial.
Singapore
Med
J.
2011;52(12):
868-873.
17.
Mauro
GL,
Martorana
U,
Cataldo
P,
Brancato
G,
Letizia
G.
Vitamin
B12
in
low
back
pain:
a
randomized,
double-blind,
placebo-controlled
study.
European
Review
for
Medical
and
Pharmacological
Sciences.
2000;4:53-58.
18.
Bannwarth
B,
Kostine
M,
Shipley
E.
Nonspecific
low
back
pain:
Assessment
of
available
medications.
Joint
Bone
Spine.
2012;79:134-136.
19.
Rocha-Gonzales
HI,
Teran-Rosales
F,
Reyes-Garcia
G,
Medina-Santillan
R,
Granados-SotoV.
B
vitamins
increase
the
analgesic
effect
of
diclofenac
in
the
rat.
Proc
West
Pharmacol
Soc.
2004;47:84-7.
20.
Reyes-Garcia
G,
Medina-Santillan
R,
Teran-Rosales
F,
et
al.
B
vitamins
increase
the
antihyperalgesic
effect
of
diclofenac
in
the
rat.
Proc
West
Pharmacol
Soc.
2002;45:147-9.
21.
Reyes-Garcia
G,
Medina-Santillan
R,
Teran-Rosales
F,
Mateos-Garcia
E,
Castillo-Henkel
C.
22.
Characterization
of
the
potentiation
of
the
antinociceptive
effect
of
diclofenac
by
vitamin
B
complex
in
the
rat.
J
Pharmacol
Toxicol
Methods.
1999;42:73-7.
23.
Bartoszyk
GD,
Wild
A.
B-vitamins
potentiate
the
antinociceptive
effect
of
dicloenacin
carrageenan-induced
hyperalgesia.
24.
Bruggemann
G,
Koehler
CO,
Koch
EM.
Results
of
a
double-blind
study
of
diclofenac
+vitamin
B1,
B6,
B12
versus
diclofenac
in
patients
with
acute
pain
of
the
lumbar
vertebrae.
A
multicenter
study.
Klin
Wochenschr.
1990;68:116-20.
25.
Kuhlwein
A,
Meyer
HJ,
Koehler
CO.
Reduced
diclofenac
administration
by
B
vitamins:
results
of
a
randomized
double
blind
study
with
reduced
daily
doses
of
diclofenac
(75
mg
diclofenac
versus
75
mg
diclofenac
plus
B
vitamins)
in
acute
lumbar
vertebral
syndrome.
Klin
Wochenschr.
1990;68:107-15.
26.
Vetter
G,
Bruggemann
G,
Lettko
M,
et
al.
Shortnening
diclofenac
therapy
by
B
vitamins.
Results
of
a
randomized
double
blind
study,
diclofenac
50
mg
versus
diclofenac
50
mg
plus
B
vitamins,
in
painful
spinal
diseases
with
degenerative
changes.
Z
Rheumatol.
1988;47:351-62.

