|
How Sensitive is Urine
Dipstick Analysis in Predicting Urinary Tract
Infections in Symptomatic Adults in a Primary
Care Setting
Mokhtar Shatla
(1)
Abdulrahman Almisfer (2)
Shamsuldin Zawawi (2)
Baraah Damanhouri (2)
Fahad Alharthi (2)
(1) Department of Family Medicine, Faculty
of Medicine, Menoufia University, Egypt; and
Department of Family Medicine, Faculty of Medicine,
Umm Alqura University, Saudi Arabia
(2) Student, Faculty of Medicine, Umm Alqura
University, Saudi Arabia
Correspondence:
Mokhtar Shatla MD
Department of Family Medicine, Faculty of Medicine,
Menoufia University, Egypt
Department of Family Medicine, Faculty of Medicine,
Umm Alqura University, Saudi Arabia
Email: mokhtarshatla@gmail.com
|
Abstract
Background:
Urinary tract infection (UTI) is a common
clinical problem in the primary care setting.
Urine dipstick analysis is a quick, cheap
and widely used test to predict UTI in
clinically suspected patients.
Objective: To evaluate the sensitivity
of urine dipstick analysis as a screening
test in predicting UTI in symptomatic
adults in the primary care setting.
Methods: A total of 420 culture-positive
urine samples from patients with symptomatic
UTI, who had dipstick urinalysis in a
primary care center were the materials
of this study from March to October 2015.
The sensitivity of urine dipstick nitrites
(NT), leukocyte esterase (LE) and blood
was calculated and compared with positive
culture samples either individually or
in combination.
Results:
The sensitivity of dipstick NT alone was
the lowest of all tests (20.7%), while
LE alone was marginally higher than NT
(31.42%), whereas dipstick blood test
when considered alone was the highest
sensitive (61.9%). In combination, NT
and/or LE were marginally higher than
either test alone (41.2%), while NT and/or
blood were (64.5%). The highest sensitivity
of dipstick is obtained when all the three
parameters were considered together (NT
and/or LE and/or Blood, sensitivity 81.4%).
Conclusion: Dipstick NT, LE, and
blood are poor screening tests when used
individually. Dipstick sensitivity significantly
increases, and it could be considered
a good screening test to predict UTI in
symptomatic adults in the primary care
setting when its three components are
considered together. However, negative
dipstick analysis should not rule out
UTI in symptomatic adults, and urine culture
is necessary for accurate diagnosis.
Key words:
Urinary tract infection, dipstick analysis,
screening, urine culture, nitrites, leukocyte
esterase, blood.
|
Overall, urinary tract infections (UTI) are
the second most common infectious complaint
in outpatient primary care clinics, and the
most common outpatient complaint caused by bacteria.
[1]It is estimated that, 2-3% of all consultations,
and even 6% in the case of women, are due to
symptoms suggesting UTI. [2]According to one
estimate, 1 out of every 2 women will experience
a UTI in her lifetime. [3]Almost 20% of UTIs
are found in men especially the elderly due
to prostatomegaly and distorted anatomy of the
urinary tract. [4]
Symptoms of uncomplicated UTI include frequency,
burning, straining, urgency, and pain with voiding.
Patients may also experience hematuria, suprapubic
pain or tenderness, and a change in the odor
of the urine. [5]
Early diagnosis of uncomplicated UTI could significantly
improve patient management in addition to providing
optimum cost-effectiveness. [6,7] Urine culture
is the gold standard for the diagnosis of UTI
but is expensive and time consuming, requiring
at least 24 hours to produce results. These
limitations have made urine analysis including
dipstick a preferred first-step investigation
among primary care clinicians. [8]
The urine dipstick is a standard diagnostic
tool of UTI, but there is much debate about
its utility and role. There is doubt that this
test is rapid, cheap, quick, and easy to administer.
[9] Leukocyte esterase (LE, an enzyme produced
by neutrophils) and nitrite (NT, the end product
of bacterial nitrate reductase acting on nitrate
in the urine), two important parameters of dipstick
urinalysis, have been frequently used to predict
UTI. Positive results of LE and NT are often
used as a reflex to confirm diagnosis by urine
culture (both in the presence and absence of
clinical symptoms of UTI), or start of empiric
antimicrobials. [10] Dipstick detection of blood
in urine has been reported to possess a high
sensitivity but poor specificity to detect UTI.
[11]
There is much debate about the utility and role
of Dipstick screening in predicting UTI. [9]Some
studies have found negative urine dipstick analysis
to be valuable in ruling out UTI. [12]However,
other studies have shown a lack of sensitivity
and specificity of these tests as indicators
of UTI. [13]
So, there is marked heterogenicity in interpretation
of results of dipstick analysis. The purpose
of this study was to evaluate the sensitivity
of dipstick urine analysis with emphasis on
NT, LE and blood test, in predicting UTI in
symptomatic patients in a primary care setting.
This study evaluated the urine dipstick analysis
of 420 culture-positive urine samples of patients
who attended the family medicine and internal
medicine outpatient clinics of Umm Alqura University
Medical Center, Makkah, Saudi Arabia, from March
to October 2015. The center provides primary
health care to the university employees and
their families.
Urine samples from patients of both sexes and
complaining of symptoms suggestive of UTI were
included. Samples of patients less than 16 years
of age, and pregnant women were excluded. The
study was approved by the Research and Ethics
Committee of Umm Alqura Faculty of Medicine.
Samples were collected by the patients themselves
where they were asked to provide a midstream
clean catch urine sample in the same day of
the test. Dipstick urine analysis was done using
multistix 10 SG (Siemens) and clinitek advantus
analyzer. The reagent strip contains test pads
for NT, LE, blood, glucose, protein, ketone,
pH, specific gravity, bilirubin and urobilinogen.
In this study, urine parameters considered in
dipstick analysis were NT, LE, and blood. Reading
time for NT and blood was one minute, and two
minutes for LE. Cut-off values for a positive
result was trace or more of LE, nitrite (+)
and blood (+).
The presence of infection in this study was
determined by quantitative urine culture. This
is the gold standard criterion against which
the three dipstick tests were compared. The
cultures were done using blood agar and MacConkey
agar plates. The cultures were read after 24
hours of incubation at 37°C. A colony count
of more than 104 organisms/ml (for one organism)
was defined as a positive urine culture for
clean catch specimens. Full bacterial identification
and antimicrobial susceptibility testing were
performed for all positive specimens.[14] Specimens
that contained more than two isolates (with
any quantitation) were considered contaminated
and were not included in the analysis. Dipstick
urinalysis data as regards NT, LE, and blood
were compared with positive culture results.
The comparison was made for every individual
test alone, then in combinations.
In
this
study,
the
urine
dipstick
analyses
of
420
culture-positive
urine
samples
of
symptomatic
adults
were
studied.
Age
of
included
patients
ranged
from
21
to
64
years.
The
mean
age
of
the
patients
was
39
years.
Among
420
patients,
77.6%
were
females
(n=326),
and
22.4%
were
males
(n=94).
Of
the
420
culture
positives
samples,
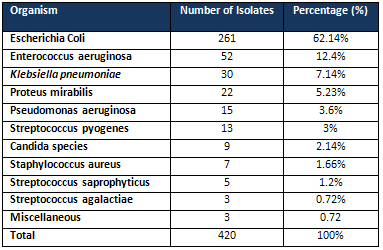
E.
coli
(62.1%)
was
the
predominant
isolate
followed
by
Enterococcus
species,
Klebsiella,
Proteus,
Pseudomonas,
Streptococcus
species,
Candida,
and
staphylococcus
aureus,
and
others
[Table
1].
The
sensitivity
of
dipstick
NT
alone
was
the
lowest
of
all
tests
(20.7%),
while
LE
alone
was
a
little
higher
than
NT
(31.42%),
whereas
dipstick
blood
test
when
considered
alone
was
the
highest
sensitive
(61.9%).
In
combination,
NT
and/or
LE
were
marginally
higher
than
either
test
alone
(41.2%),
while
NT
and/or
blood
were
(64.5%).
The
sensitivity
increases
when
LE
and/or
blood
were
considered
(69.7%).
The
highest
sensitivity
of
dipstick
screening
is
obtained
when
all
the
three
test
parameters
are
considered
together
(81.4%)
[Table
2].
Table
1:
Number
and
percentage
of
the
isolated
organisms
on
the
culture
positive
specimens
Table
2:
Sensitivity
of
the
urine
Dipstick
analysis
used
for
screening
UTI
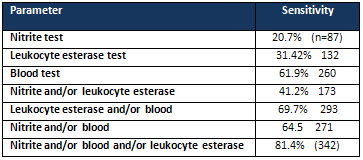
UTI:
urinary
tract
infections
Urinary
tract
infection
is
the
second
common
bacterial
infection
in
the
primary
care
setting.
It
is
more
common
in
females
especially
during
their
reproductive
age.
In
this
study,
most
patients
diagnosed
with
UTI
were
females.
This
coincides
with
many
studies
which
reported
higher
prevalence
of
UTI
in
adult
women
compared
to
men
mainly
due
to
the
anatomy
of
the
female
genito-urinary
tract.[3]
Diagnosis
of
UTI
is
based
on
clinical
symptoms,
together
with
positive
urine
culture.[15]
However,
the
concerns
of
cost-effectiveness
and
lengthy
processing
time
in
urine
culture
have
stimulated
the
use
of
other
rapid
diagnostic
tools
to
predict
UTI.[16]
Dipstick
analysis
is
a
common
rapid
laboratory
screening
tool
used
by
many
primary
care
clinicians
to
predict
UTI
in
symptomatic
patients.
It
assesses
presence
of
bacteriuria,
pyuria,
and
hematuria
associated
with
UTI.
Notably,
several
studies
have
demonstrated
significant
heterogenicity
in
interpretation
of
dipstick
results.[17]
Dipstick
nitrite
test
(NT)
is
used
to
detect
bacteriuria.
Normally,
nitrites
are
not
found
in
urine
but
result
when
bacteria
reduce
urinary
nitrates
to
nitrites.
Many
gram-negative
bacteria
including
E.
Coli,
and
some
gram-positive
bacteria
are
capable
of
this
conversion,
and
a
positive
dipstick
nitrite
test
indicates
that
these
bacteria
are
present
in
significant
numbers
(i.e.,
more
than
10,000
per
mL).
[18]
However,
non-nitrate-reducing
organisms
e.g.
Candida
and
Streptococci
including
Enterococci
do
not
reduce
nitrates,
and
may
cause
false-negative
results.
Although
E.
coli
was
the
predominantly
isolated
organism
in
this
study
(62.1%),
similar
to
other
studies,[19-21]
almost
20%
of
the
isolates
were
Enterococci,
Candida,
and
Streptococcus
species,
which
do
not
produce
nitrites.
Also,
for
bacteria
to
be
able
to
reduce
nitrates
and
produce
nitrites,
urine
should
contain
sufficient
dietary
nitrates
and
have
been
retained
in
the
bladder
for
more
than
4
hours
before
voiding.[22,23]
Performing
this
test
on
dilute
urine
may
contribute
to
false-negative
findings.[24]
In
patients
who
urinate
frequently,
dilution
of
NT
may
result
in
negative
results.
The
first
voided
urine
morning
specimen
has
been
proven
to
be
accurate
for
nitrate,
but
such
sample
collection
was
not
possible
in
all
patients
in
this
study.
[25]Also,
NT
may
be
affected
by
common
antibiotics
e.g.
nitrofurantoin,
cephalexin,
doxycycline,
as
well
as
vitamin
C
and
phenazoperidine
leading
to
suboptimal
detection
of
bacteria.
[26]
Hence,
an
absence
of
urinary
nitrite
cannot
rule
out
UTI.
All
mentioned
above
may
be
the
likely
explanations
for
the
low
sensitivity
of
nitrite
test
in
this
study
when
done
alone.
This
has
been
supported
by
findings
from
other
similar
studies.
[27,
28]
However,
the
sensitivity
of
nitrites
in
other
studies
varied
between
39%
and
81%.
[19,
25,
29]
The
leukocyte
esterase
(LE)
test
detects
esterase,
an
enzyme
released
by
neutrophils
and
may
indicate
white
cells
in
urine
(pyuria)
associated
with
UTI.
[22]
Normally,
urine
is
negative
for
LE.
Positive
value
of
the
test
correlates
with
the
number
of
WBC/hpf
urine
sediment,
and
can
vary
from
trace
to
many.
[30]
However,
there
are
many
conditions
other
than
UTI
causing
pyuria
and
subsequent
positive
LE
test
results
e.g.
chlamydial
urethritis,
analgesic
nephropathy
and
bladder
tumors.
False
positives
are
seen
in
conditions
when
the
urine
is
contaminated
with
bacteria,
eosinophils
or
trichomonas.
These
reasons
cause
the
positive
predictive
value
of
the
LE
test
to
vary
from
19%
to
88%.
[31,
32]
False
negative
results
may
occur
in
the
presence
of
significant
levels
of
protein
or
glucose
and
in
urines
with
high
specific
gravity
which
can
crenate
the
white
blood
cells,
leaving
them
unable
to
release
esterases.
[26,
33]
Similar
to
NT,
LE
results
may
be
affected
by
common
antibiotics
mentioned
above,
as
well
as
vitamin
C,
phenazoperidine,
glycosuria,
and
urobilinogen.
Also,
high
proteinuria
has
been
shown
to
inhibit
LE
test.
[26,34,35]
Hence,
LE
when
considered
alone
as
a
parameter
for
diagnosing
UTI
is
not
as
sensitive
as
when
it
is
combined
with
nitrites
in
urine.
A
similar
finding
by
Bhavsar
et
al.,
[36]
found
only
substantial
improvement
of
sensitivity
when
NT
and
LE
are
combined
together
to
predict
UTI
in
urine
culture
positive
patients.
This
finding
was
different
from
other
studies
where
the
sensitivity
of
LE
alone
was
high
and
varied
between
61.7%
and
77%.
[29,
37,
38]
The
explanation
for
low
sensitivity
of
LE
in
this
study
may
be
attributed
to
some
patients'
self-initiation
of
common
antibiotics
to
treat
their
condition.
These
medications
are
given
over-the-counter
in
Saudi
Arabia.
Moreover,
false
negative
LE
test
may
be
attributed
to
glycosuria
and
proteinuria,
a
common
association
of
a
prevalent
medical
problems
in
Saudi
Arabia,
diabetes
mellitus.
The
dipstick
test
for
blood
detects
the
peroxidase
activity
of
erythrocytes
in
case
of
hematuria
with
UTI.
However,
myoglobin
and
hemoglobin
also
will
catalyze
this
reaction,
so
a
false
positive
test
result
may
occur
with
conditions
other
than
UTI
including
hematuria
and
myoglobinuria
e.g.
ureteric
calculus,
glomerular
diseases,
menstrual
blood,
malignancy,
medications,
concentrated
urine,
and
strenuous
exercise.
[34]
False
negative
results
occur
if
pH
of
urine
is
less
than
5.1,
high
specific
gravity,
and
ascorbic
acid
(vitamin
C)
is
present
in
the
urine.
[22]
Blood
test
was
the
highest
sensitive
single
test
in
this
study.
It
has
been
reported
that
dipstick
sensitivity
for
blood
ranges
from
91-100%.[22,39,40]
In
this
study,
the
sensitivity
of
dipstick
was
highest
(81.4%)
when
its
three
parameters
(NT/LE/blood)
were
all
considered
together,
where
any
positive
dipstick
test
results
for
detection
of
bacteruria
by
NT
and/or
detection
of
pyuria
by
LE
and/or
detection
of
blood
improves
sensitivity
significantly,
a
finding
comparable
with
that
of
Mambatta
et
al.
with
sensitivity
74%,[40]
and
Memi?o?ullari
et
al.
with
a
sensitivity
of
80%,
[41].
However,
in
almost
one
fifth
of
the
patients,
there
will
be
no
positive
dipstick
test
results
and
the
patient's
diagnosis
might
be
missed.
Hence,
correlation
of
the
dipstick
test
results
with
the
patient's
clinical
condition
is
essential
for
accurate
diagnosis.
Dipstick
NT,
LE,
and
blood
are
poor
screening
tests
when
used
individually.
However,
Dipstick
sensitivity
significantly
increases,
and
it
could
be
considered
a
good
screening
test
to
predict
UTI
in
symptomatic
adults
in
the
setting
of
primary
care
when
its
three
components
are
considered
together.
However,
negative
dipstick
analysis
should
not
rule
out
UTI
in
adult
patients
with
symptoms
suggestive
of
UTI,
and
urine
culture
is
recommended
for
these
patients
for
proper
diagnosis
and
management.
Primary
care
and
family
physicians
are
encouraged
to
utilize
the
quick,
cheap,
sensitive
dipstick
screening
to
predict
UTI
in
symptomatic
adults
in
primary
care
centers,
and
to
delegate
the
expensive,
time
consuming
urine
culture
for
highly
suggestive
conditions
of
UTI
with
negative
dipstick
screening.
Larger
studies
are
recommended
for
larger
samples
from
multiple
primary
care
centers
for
more
data
generalizability.
1.
Foxman
B.
Epidemiology
of
urinary
tract
infections:
incidence,
morbidity,
and
economic
costs.
Am
J
Med.
2002;113(Suppl
1A):5S-13S.
2.
Brooks
D:
The
management
of
suspected
urinary
tract
infection
in
general
practice.
Br
J
Gen
Pract
1990,
40:399-402.
3.
Kunin
CM.
Urinary
tract
infections
in
females.
Clin
Infect
Dis.
1994;18:1-12
4.
Griebling
TL.
Urinary
tract
infection
in
men.
In:
Litwin
MS,
Saigal
CS,
Editors.
Urologic
Diseases
in
America.
DHHS,
PHS,
NIH,
NIDDK.
Washington,
DC:
GPO;
NIH
publication
075512;
2007.
p.
62145.
5.
Medina-Bombardo
D,
Segui-Diaz
M
Roca-Fusalba
C,
Llobera
J.
What
is
the
predictive
value
of
urinary
symptoms
for
diagnosing
urinary
tract
infection
in
women?
Fam
Pract.
2003;20:103-107.
6.
Gupta
K,
Hooton
TM,
Naber
KG,
et
al.
Infectious
Diseases
Society
of
America,
European
Society
for
Microbiology
and
Infectious
Diseases.
International
clinical
practice
guidelines
for
the
treatment
of
acute
uncomplicated
cystitis
and
pyelonephritis
in
women:
a
2010
update
by
the
Infectious
Diseases
Society
of
America
and
the
European
Society
for
Microbiology
and
Infectious
Diseases.
Clin
Infect
Dis.
2011;Mar;52(5):e103-20.
7.
Little
P,
Turner
S,
Rumsby
K,
et
al.
Developing
clinical
rules
to
predict
urinary
tract
infection
in
primary
care
settings:
sensitivity
and
specificity
of
near
patient
tests
(dipsticks)
and
clinical
scores.
Br
J
Gen
Pract.
2006
Aug;56(529):606-612.
8.
Lohr
JA:
Use
of
routine
urinalysis
in
making
a
presumptive
diagnosis
of
urinary
tract
infection
in
children.
Pediatr
Infect
Dis
J
1991,
10:646-50
9.
Deville
WLJM,
Yzermans
JC,
van
Duijn
NP,
Bezemer
PD,
van
der
Windt
DAWM,
Bouter
LM.
The
urine
dipstick
test
useful
to
rule
out
infections:
a
meta-analysis
of
the
accuracy.
BMC
Urol.
2004;4:1-14.
10.
Lohr
JA,
Portilla
MG,
Geuder
TG,
Dunn
ML,
Dudley
SM.
Making
a
presumptive
diagnosis
of
urinary
tract
infection
by
using
a
urinalysis
performed
in
an
on-site
laboratory.
The
Journal
of
Pediatrics.
1993;122:22-25.
11.
Anderson
J,
Fawcett
D,
Goldber
L,
et
al.
Joint
consensus
statement
on
the
initial
assessment
of
haematuria.
Prepared
on
behalf
of
the
Renal
Association
and
British
Association
of
Urological
Surgeons.
2008.
Available
from:
www.baus.org.uk
(Accessed
Jan,
2016).
12.
Ohly
N,
Teece
S.
Accuracy
of
negative
dipstick
urine
analysis
in
ruling
out
urinary
tract
infection
in
adults.
Emerg
Med
J
2003;20:362-3.
13.
Van
Nostrand
JD,
Junkins
AD,
Bartholdi
RK:
Poor
predictive
ability
of
urinalysis
and
microscopic
examination
to
detect
urinary
tract
infection.
American
Journal
of
Clinical
Pathology.
2000;113:709-713.
14.
McCarter
YS,
Hall
GS,
Zervos
M.
Laboratory
diagnosis
of
urinary
tract
infections.
Cumitech.
Edited
by
Coordinating
ed.
SSE.
Washington,
DC:
ASM
Press,
2009.
15.
Brendler,
CB.
Evaluation
of
the
urologic
patient:
history,
physical
examination
and
urinalysis.
In:
Campbell
MF,
Walsh
PC.
Campbell's
Urology.
7th
ed.
Philadelphia:
Saunders,
1998:144-56.
16.
Lifshitz
E,
Kramer
L:
Outpatient
urine
culture:
does
collection
technique
matter?
Archives
of
Internal
Medicine.
2000;160:2537-2540.
17.
Gorelick
MH,
Shaw
KN.
Screening
tests
for
urinary
tract
infection
in
children:
A
meta-analysis.
Pediatrics.1999;04:e54.
18.
Pels
RJ,
Bor
DH,
Woolhandler
S,
Himmelstein
DU,
Lawrence
RS.
Dipstick
urinalysis
screening
of
asymptomatic
adults
for
urinary
tract
disorders.
II.
Bacteriuria.
JAMA.
1989;262:1221-4.
19.
Taneja
N,
Chatterjee
SS,
Singh
M,
Sivapriya
S,
Sharma
M,
Sharma
SK.
Validity
of
quantitative
unspun
urine
microscopy,
dipstick
test
leucocyte
esterase
and
nitrite
tests
in
rapidly
diagnosing
urinary
tract
infections.
J
Assoc
Physicians
India
2010;58:485-7.
20.
Marques
LP,
Flores
JT,
Barros
Junior
Ode
O,
Rodrigues
GB,
MouracCde
M,
Moreira
RM.
Epidemiological
and
clinical
aspects
of
urinary
tract
infection
in
community?dwelling
elderly
women.
Braz
J
Infect
Dis
2012;16:436-41.
21.
Huysal
K,
Budak
YU,
Karaca
AU,
Aydos
M,
Kahvecioglu
S,
Bulut
M,
et
al.
Diagnostic
accuracy
of
UriSed
automated
urine
microscopic
sediment
analyser
and
dipstick
parameters
in
predicting
urine
culture
test
results.
Biochem
Med
(Zagreb)
2013;23:211-17.
22.
JEFF
A.
SIMERVILLE,
M.D.,
WILLIAM
C.
MAXTED,
M.D.,
and
JOHN
J.
PAHIRA,
M.D.,
Urinalysis:
A
Comprehensive
Review.
Am
Fam
Physician.
2005
Mar
15;71(6):1153-1162.
23.
Evans
PJ,
Leaker
BR,
McNabb
WR,
Lewis
RR:
Accuracy
of
reagent
strip
testing
for
urinary
tract
infection
in
the
elderly.
Journal
of
the
Royal
Society
of
Medicine.
1991;84:598-599.
24.
Pezzlo
M.
Detection
of
urinary
tract
infections
by
rapid
methods.
Clinical
Microbiology
Reviews.1988;1:268-280.
25.
Thakre
SS,
Dhakne
SS,
Thakre
SB,
Thakre
AD,
Ughade
SM,
Kale
P.
Can
the
Griess
Nitrite
Test
and
a
Urinary
Pus
Cell
Count
of
?5Cells
Per
Micro
Litre
of
Urine
in
Pregnant
Women
be
Used
for
the
Screening
or
the
Early
Detection
of
Urinary
Tract
Infections
in
Rural
India?
J
Clin
Diagn
Res
2012;6:1518-22.
26.
Beer
JH,
Vogt
A,
Neftel
K,
Cottagnoud
P.
False
positive
results
for
leucocytes
in
urine
dipstick
test
with
common
antibiotics.
BMJ.
1996;313:25.
27.
Zaman
Z,
Borremans
A,
Verhaegen
J,
Verbist
L,
Blanckaert
N.
Disappointing
dipstick
screening
for
urinary
tract
infection
in
hospital
inpatients.
Journal
of
Clinical
Pathology.
1998;51:471-472.
28.
Loo
SY,
Scottolini
AG,
Luangphinith
S,
Adam
AL,
Jacobs
LD,
Mariani
AJ:
Urine
screening
strategy
employing
dipstick
analysis
and
selective
culture:
an
evaluation.
American
Journal
of
Clinical
Pathology.
1984;81:634-642.
29.
Rehmani
R.
Accuracy
of
urine
dipstick
to
predict
urinary
tract
infections
in
an
emergency
department.
J
Ayub
Med
Coll
Abbottabad
2004;16:4-7.
30.
SHARP
V
J,
LEE
DK,
Askeland
EJ.
Urinalysis:
Case
Presentations
for
the
Primary
Care
Physician.
Am
Fam
Physician.
2014
Oct
15;90(8):542-547.
31.
Semeniuk
H,
Church
D.
Evaluation
of
the
leukocyte
esterase
and
nitrite
urine
dipstick
screening
tests
for
detection
of
bacteriuria
in
women
with
suspected
uncomplicated
urinary
tract
infections.
J
Clin
Microbiol
1999;37:3051-2.
32.
Bartlett
RC,
Zern
DA,
Ratiewicz
I,
Tetreault
JZ.
Reagent
strip
screening
for
sediment
abnormalities
identified
by
automated
microscopy
in
urine
from
patients
suspected
to
have
urinary
tract
disease.
Arch
Pathol
Lab
Med
1994;118:1096-101.
33.
McNair
RD,
MacDonald
SR,
Dooley
SL,
Peterson
LR:
Evaluation
of
the
centrifuged
and
Gram-stained
smear,
urinalysis,
and
reagent
strip
testing
to
detect
asymptomatic
bacteriuria
in
obstetric
patients.
American
Journal
of
Obstetrics
and
Gynecology.
2000;182:1076-1079.
34.
Gerber
GS,
Brendler
CB.
Evaluation
of
the
urologic
patient:
History,
physical
examination,
and
urinalysis.
In:
Wein
AJ,
Kavoussi
LR,
Novick
AC,
Partin
AW,
Peters
CA,
Editors,
Campbell-Walsh
Urology.
9th
ed.
Philadelphia:
Saunders
Elsevier;
2007.
p.
81-110.
35.
McPherson
RA,
Ben-Ezra
J.
Basic
examination
of
urine.
In:
McPherson
RA,
Pincus
MR,
Editors,
Henry's
Clinical
Diagnosis
and
Management
by
Laboratory
Methods.
22nd
ed.
Philadelphia:
Saunders
Elsevier;
2011.
p.
chap28.
36.
Bhavsar
T,
Potula
R,
Jin
M,
Truant
AL.
Predictability
of
urinalysis
parameters
in
the
diagnosis
of
urinary
tract
infection:
a
case
study.
MLO
Med
Lab
Obs.
2015
Jan;47(1):8,
10,
12;
quiz
13.
37.
Laosu-angkoon
_S.
The
sensitivity
and
specificity
of
a
urine
leukocyte
esterase
dipstick
test
for
the
diagnosis
of
urinary
tract
infection
in
the
outpatient
clinic
of
Rajavithi
Hospital.
J
Med
Assoc
Thai
2013;96:849-53.
38.
Gieteling
E,
van
de
Leur
JJ,
Stegeman
CA,
Groeneveld
PH.
Accurate
and
fast
diagnostic
algorithm
for
febrile
urinary
tract
infections
in
humans.
Neth
J
Med
2014;72:356-62.
39.
Woolhandler
S,
Pels
RJ,
Bor
DH,
Himmelstein
DU,
Lawrence
RS.
Dipstick
urinalysis
screening
of
asymptomatic
adults
for
urinary
tract
disorders.
I.
Hematuria
and
proteinuria.
JAMA.
1989;262:1214-9.
40.
Mambatta
AK,
Jayarajan
J,
Rashme
VL,
Harini
S,
Menon
S,
Kuppusamy
J.
Reliability
of
dipstick
assay
in
predicting
urinary
tract
infection.
J
Fam
Med
Primary
Care
2015;4:265-8.
41.
Memisogullari
R,
Yüksel
H,
Hayriye
Ak
Y?ld?r?m,
Yavuz
O.
Performance
characteristics
of
dipstick
and
microscopic
urinalysis
for
diagnosis
of
urinary
tract
infection.
Eur
J
Gen
Med
2010;7:174-8.
|

