|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
........................................................
In Memoriam
Professor
Orhan Ekrem Müftüoglu
|
........................................................
Original
Contribution / Clinical Investigation
|







|
Cholelithiasis
and cholecystectomy may lower the low density
lipoprotein cholesterol in plasma
DOI: 10.5742/MEWFM.2017.93010
[pdf
version]
Mehmet Rami Helvaci, Mursel Davarci, Orhan Veli
Ozkan, Ersan Semerci, Abdulrazak Abyad, Lesley
Pocock
Serum
and follicular fluid vitamin D and follicular
response among infertile women undergoing ICSI
DOI: 10.5742/MEWFM.2017.93011
[pdf
version]
Sedighe Esmaeilzadeh, Maryam Aliasgharpour,
Parvaneh Mirabi, Azita Ghanbarpour
Maede Fasihian
Studying
the relation of quality of work life with socio-economic
status and general health among the employees
working in Students Welfare Fund of Ministry
of Health and Medical Education in 2016
DOI: 10.5742/MEWFM.2017.93012
[pdf
version]
Saeed Reza Azami, Nasrin Shaarbafchizadeh, Soheil
Mokhtari, Ali Maher
On the Effect
of Cognitive Behavioural Counseling on Sexual
Satisfaction of Mothers with Autistic Children:
A Randomized Clinical Trial
DOI:
[pdf version]
Leila Arbil, Mitra Kolivand, Farzaneh Golboni,
Effat MerghatiKhoei, Mansour Rezaei
Pre-operative
sublingual misoprostol and intra-operative blood
loss during total abdominal hysterectomy: a
randomized single-blinded controlled clinical
trial
DOI: 10.5742/MEWFM.2017.93013
[pdf
version]
Taravat Fakheri, Tayebe Noori
Investigating
the Effect of Endotracheal Tube Cuff Pressure
on Sore Throat, Hoarseness and Cough in Patients
with Coronary Artery Bypass Surgery
DOI: 10.5742/MEWFM.2017.93014
[pdf
version]
Ali Akbar Vaezi, Mohammad Hassan Mondegari Bamakan
Comparing
the Self-Esteem and Resiliency between Blind
and Sighted Children and Adolescents in Kermanshah
City
DOI: 10.5742/MEWFM.2017.93015
[pdf
version]
Saeedeh Bakhshi, Nafiseh Montazeri , Babak Nazari,
Arash Ziapour, Hashem Barahooyi,
Fatemeh Dehghan
|
........................................................
Population
and Community Studies
|







|
Frequency
of Uric Acid Levels, Symptomatic and Asymptomatic
Hyperuricemia among the Pakistani Population
DOI: 10.5742/MEWFM.2017.93016
[pdf
version]
Waris Qidwai, Masood Jawaid
Determinants
of Tooth Brushing among Primary School Students
DOI: 10.5742/MEWFM.2017.93017
[pdf
version]
Mohammad Mahboubi, Mohammad Ismail Motlagh,
Mehdi Mirzaei-Alavijeh, Farzad Jalilian, Hassan
Gharibnavaz,
Mohammad Fattahi
Depression
in patients suffering from gender dysphoria:
The hospitalized patients of Legal Medicine
Center in Southwest of Iran
DOI: 10.5742/MEWFM.2017.93018
[pdf
version]
Zahra Gorjian, Mohammad Zarenezhad, Mohhamad
Mahboubi, Saeid Gholamzadeh,
Nahid Mahmoodi
An epidemiological
study of suicide attempts and to determine the
correlation between attempted suicide causes
and demographic characteristics of people in
Kermanshah Province during a year
DOI: 10.5742/MEWFM.2017.93019
[pdf
version]
Hamid Reza Shetabi, Samira Rostami, Mohsen Mohammadi,
Mahsa Cheleii, Lida Saedi, Saba Amiri Nasab,
Shirin Zardui GolAnbari
The
effectiveness of life skills training on happiness,
mental health, and marital satisfaction in wives
of Iran-Iraq war veterans
DOI: 10.5742/MEWFM.2017.93038
[pdf
version]
Kamal Solati
The
Role of Self-Compassion Factors in Predicting
the Marital Satisfaction of Staff at Kermanshah
University of Medical Sciences
DOI:10.5742/MEWFM.2017.93020
[pdf
version]
Parisa Janjani, Lida Haghnazari, Farahnaz Keshavarzi,
Alireza Rai
Mediating
role of irrational beliefs in the relationship
between the quality of family communication
and marital satisfaction
DOI:10.5742/MEWFM.2017.93021
[pdf
version]
Parisa Janjani, Khodamorad Momeni, Alireza Rai,
Mohammad Reza Saidi
|
........................................................
Review Article
........................................................
International Health
Affairs
........................................................
Education
and Training
........................................................
Clinical
Research and Methods
|





|
Adaptive
LASSO Logistic Regression applied on gene expression
of prostate cancer
DOI: 10.5742/MEWFM.2017.93028
[pdf version]
Amir Hossein Hashemian, Maryam Ghobadi Asl,
Soodeh Shahsavari, Mansour Rezaei,
Hadi Raeisi Shahraki
The
prevalence of brain and neck injuries in patients
with maxillofacial fractures in teaching hospitals
of Rasht in 2016
DOI: 10.5742/MEWFM.2017.93029
[pdf
version]
Seyed Mohammad Talebzadeh, Ali Khalighi Sigaroudi,
Babak Alijani, Safa Motevasseli,
Saied Dashtyari, Mahsa Shariati, Zeinab Davoudmanesh
Cultural
competency: a concept analysis in TUMS (Tehran
University of Medical Science) DOI:
10.5742/MEWFM.2017.93030
[pdf version]
Foruzan Khatamidoost, Mandana Shirazy, Hamid
Khankeh, Nemat Allah Musapour
Majid Sadeghi, Kamran Soltani Arabshahi
The
Effect of Proprioceptive Neuromuscular Facilitation
(PNF) on Activities of Daily Living of client
with Cerebrovascular accident
DOI: 10.5742/MEWFM.2017.93031
[pdf
version]
Najafi Doulatabad Shahla, Afrasiabifar Ardashir,
Parandvar Yaghoub
Evaluation
of the ratio of T helper 17 and T regulatory
cells in patients with chronic idiopathic urticaria
DOI: 10.5742/MEWFM.2017.93032
[pdf
version]
Hossein Shahriari, Farahzad Jabbari, Seyyed
Abdolrahim Rezaee, Houshang Rafatpanah
Majid Jafari, Reza Farid Hosseini, Majid Asadi-Samani
|
........................................................
Model
and System of Primary Care
........................................................
Case
Series and Case Reports
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| September 2017
- Volume 15, Issue 7 |
|
|
Right Thoracotomy Beating
Heart Technique in Emergency Re-Do Mitral Valve
Surgery: Is it Still Justified?
Hassan Mir Mohammad Sadeghi
Correspondence:
Hassan Mir Mohammad Sadeghi, BS, MD
Assistant Professor of Surgery, Rajaie Cardiovascular,
Medical and Research Center, Iran University
of Medical Sciences, Tehran, Iran
Email: samani1395@yahoo.com
|
Abstract
Background: With
the progressive aging of the western population,
cardiac surgeons are faced with treating
an increasing number of critically ill
and elderly patients. Controversy exists
as to whether the ordinary mid-sternotomy
approach to these malfunctioning mitral
valves will do the job or if the new right
thoracotomy approach without cross clamping
the aorta is better suited to take care
of the problem. The potential to avoid
mid-sternotomy surgery in re-do patients
with little chance of survival and poor
quality of life postoperatively would
spare unnecessary suffering, reduce operation
mortality, and enhance the use of resources.
Methods:
We managed 125 cases of severely ill patients
admitted to our department on referral
from rural areas with malfunctioning prosthetic
mitral valves from July 15, 2000 through
to August 30, 2012. In our study of 23
patients with right thoracotomy approach,
13 patients were women. Preoperatively
most of the patients were not moribund,
but 59% had ischemia. All of the patients
had prosthetic mitral valves. Hospital
mortality and morbidity modes, based on
our overall experience with 125 patients
operated on for malfunctioning mitral
valves during the period of the study
were developed by means of multivariate
logistic regression with preoperative
and intra operative variables used as
independent predictors of outcome.
Results: Our
overall hospital mortality was 13% compared
with 21% of standard median sternotomy
procedures. There was no intraoperative
mortality. All patients who survived had
one or more postoperative complications.
Mean hospital stay was 17 days with an
average of 10 days in the intensive care
units. All of the survivors (21 patients)
discharged from the hospital were able
to function
independently and
their survival at 6 months was 100%. Statistical
analysis of the overall experience with
this new operation for malfunction of
prosthetic mitral valves confirmed that
via Right Thoracotomy, the cross-clamping
of the aorta is the most important independent
patient risk factor associated with 30-day
mortality and morbidity.
Conclusion:
Operations for critically ill patients
involve increased hospital mortality and
morbidity. Short-term survival is unfavorable
and is associated with poor quality of
life. With additional corroborative studies
to endorse the present findings, the use
of right thoracotomy approach to have
access to malfunctioning mitral valve
without the cross-clamping of the aorta
remains a substantiated concept. In the
context of these critically ill patients,
the hypothesis that right thoracotomy
approach without the cross-clamping of
the aorta should be advocated for surgical
intervention to save these patients and
to conserve resources is supported by
the presented data.
Key words:
Emergency heart surgery, mitral valve
malfunction, thoracotomy
|
With important demographic changes taking place
in cardiac surgical practice, critically ill
patients are more frequently undergoing complex
operations (1-4). Controversy exists as to whether
the classical mid-sternotomy approach with cross-clamping
of aorta is better tolerated by patients compared
to right thoracotomy without the cross-clamping
of the aorta. Published studies on elective
coronary bypass graft and valve surgery reveal
that elderly and critically ill patients should
not be denied these procedures, although the
treatment of older patients involves increased
hospital mortality and morbidity, and longer
hospital stays (1-3).
Malfunctioning prosthetic mitral valve is generally
an acute condition and mortality from this remains
high despite important advances in operative
therapy. Recent reports indicate that cardiac
function is a risk determinant of early results
after emergency valve surgery. The study reviews
our experience with a particular subset of patients
with malfunctioning prosthetic mitral valves
referred to our center.
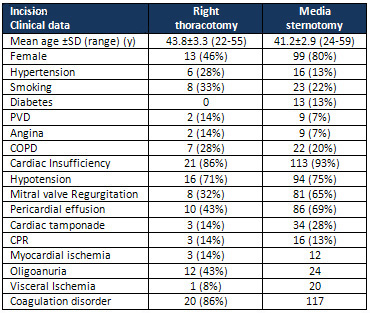
We
reviewed
the
records
of
23
malfunctioning
mitral
valve
patients
who
underwent
surgery
via
right
thoracotomy
from
July
15,
2000,
to
August
30,
2012
at
Heart
Hospital,
in
Tehran,
Iran.
They
represented
18%
of
125
operations
for
prosthetic
valve
malfunction
performed
in
the
same
period.
The
clinical
characteristics
of
these
patients,
consisting
of
13
women
and
10
men
are
presented
in
Table
1.
The
mean
age
of
patients
was
43.8
years
(median
33;
range
20-55
years).
All
the
patients
had
associated
diseases.
On
admission,
no
patient
was
moribund
and
none
required
external
chest
compression
for
cardiopulmonary
resuscitation,
although
67%
of
the
patients
had
hemodynamic
instability.
One
patient
was
unconscious
on
admission,
and
2
had
a
preoperative
stroke.
Renal
and
respiratory
insufficiency
was
present
before
admission
in
29%
and
70%
of
the
patients,
respectively.
A
total
of
57%
of
the
patients
had
a
reduction
in
renal
function
preoperatively,
which
was
largely
attributable
to
hemodynamic
instability.
Table
1:
Clinical
data
Ischemia
was
encountered
in
only
one
patient.
Moderate
to
severe
chronic
cardiac
failure
was
present
before
admission
in
29%
of
the
subjects.
No
patient
was
refused
surgery
because
of
age
or
concomitant
disease.
On
admission,
all
the
patients
had
severe
coagulation
disorders.
Platelet
aggregation
(aggregometry)
and
homeostasis
(thromboelastography)
were
markedly
reduced
in
all
the
patients.
In
addition,
variable
degrees
of
thrombocytopenia,
low
levels
of
the
thrombin
inhibitor
angiotensin
III,
and
coagulation
factors
(fibrinogen,
V,
VU,
\mi,
and
DC),
and
high
levels
of
plasmin
degradation
of
cross-linked
fibrin
(D-dimer)
were
measured.
All
procedures
were
performed
with
emergency
status
within
24
hours
after
the
initial
onset
of
dyspnoea
on
exertion
and
chest
pain,
and
all
the
patients
were
operated
on
within
4
hours
of
their
arrival.
The
operative
techniques
used
are
summarized
in
Table
2.
Click
here
for
Table
2:
Operations
Operative
Technique
All
the
operations
in
this
series
of
23
cases
were
performed
through
right
thoracotomy
incision
according
to
previously
described
standard
surgical
techniques.
In
the
last
case,
ascending
aortic
cannulation
was
done
instead
of
femoral
cannulation,
which
was
due
to
a
history
of
recent
bilateral
femoral
artery
embolectomy
procedure.
Preoperative
coagulation
disorders
were
aggressively
treated
from
the
time
of
admission
with
the
aid
of
blood
bank
products,
antithrombin
III,
aprotinin
and
coagulation
factor
concentrates.
Continuous
ultra
filtration
during
CPB
was
occasionally
used
as
was
a
cell
saver
device
(Haemonetics
Corp.,
Braintree,
Mass).
Arterial
pressure
monitoring
lines
were
routinely
placed
in
radial
arteries.
Systemic
anticoagulation
for
CPB
was
accomplished
with
heparin
at
an
initial
dose
of
3
mg/kg
body
weight.
Adequate
heparinization
for
CPB
was
assessed
with
the
activated
clotting
time
(Hemochron
FTK-ACT;
International
Technique
Corp.,
Edison
NJ),
with
further
dose
of
heparin
administered
as
required
so
as
to
maintain
an
activated
clotting
time
greater
than
750
seconds.
At
the
end
of
the
procedures,
heparin
was
neutralized
with
protamine
(0.8
mg
of
protamine
per
milligram
of
heparin).
CPB
was
established
with
cardiac
indices
of
2.0,
2.5
L.
Min-1
m-2.
Cooling
was
stopped
at
33°
C
in
patients
operated
on
without
the
cross-clamp
technique
under
mild
hypothermia.
Arterial
inflow
adequacy
was
assessed
clinically.
Acid-base
management
during
mild
hypothermia
was
via
an
alpha-stat
approach.
Before
opening
the
left
atrium,
the
head-down
position
(Trendelenberg)
was
established
and
immediately
after
opening
the
left
atrium,
provision
was
made
to
render
the
mitral
valve
incompetent
so
that
the
left
ventricle
would
pump
into
the
left
atrium
instead
of
the
aortic
root.
The
postoperative
homeostasis
protocol
used
was
derived
from
that
proposed
by
Szefner,
and
included
tests
for
platelet
function,
thrombin
formation
and
its
regulatory
pathways,
and
for
the
fibrinolytic
system.
Treatment
included
the
administration
of
small
doses
of
protamine,
modulated
doses
of
aprotinin,
fresh
frozen
plasma
as
well
as
fibrinogen.
Dosages
were
adapted
to
each
patient’s
clinical
profile
as
well
as
to
test
interpretation
criteria
in
order
to
provide
personalized
treatment.
Statistical
Methods
Medical
records
of
all
the
125
patients
operated
on
for
malfunctioning
mitral
valve
between
July
18,
2000,
and
August
30,
2012,
were
reviewed
and
preoperative
variables
that
were
believed
to
have
an
impact
on
outcome
were
obtained
(Table
1).
Data
were
studied
by
descriptive
and
statistical
analyses.
The
SPSS
application
software
version
10.0
(SPSS
Inc.,
Chicago,
ILL)
was
used
for
statistical
analyses.
Significant
differences
between
the
two
procedure
groups
(i.e.
median
sternotomy
and
right
thoracotomy
without
aortic
cross-clamping)
were
assessed
with
univariate
analysis
(Tables
1
to
3):
categoric
data
were
compared
by
means
of
the
x2
test
or
the
Fisher
exact
test
(as
appropriate)
and
continuous
variables
with
the
student
t
test.
Data
were
further
analyzed
by
univariate
and
multivariate
logistic
regression
with
the
response
variable
on
the
one
hand
being
hospital
mortality
(30
days
mortality),
and
on
the
other
hand,
morbidity.
All
variables
with
a
zero
or
near
zero
cell
count
were
treated
as
continuous
so
that
convergence
could
be
obtained.
Multivariate
models
were
applied
to
isolate
the
effect
of
each
factor
adjusted
for
all
other
factors:
the
0.25
level
(P<
0.25)
was
used
as
a
screening
criterion
for
the
selection
of
candidate
variables.
In
order
that
problems
created
by
multi
collinearity
could
be
avoided,
variables
that
were
too
highly
correlated
among
them
were
included
at
different
times
in
different
models.
A
background
procedure
was
used.
A
Wald
x2
test
was
used
for
testing
the
significance
of
individual
coefficients.
The
results
are
shown
as
odds
ratios
with
95%
confidence
intervals.
Descriptive
Analysis
Mortality:
Overall
hospital
mortality
was
13%
(three
patients,
Table
3).
Click
here
for
Table
3:
Complications
ntra-operative
mortality
was
9%
(12
patients).
Intra-operative
deaths
included
all
9
patients
with
bleeding
from
coagulation
disorders.
The
bleeding
was
due
to
the
poor
quality
of
the
ventricular
tissue
at
the
site
of
adhesional
release
in
9
patients
and
to
the
technique
of
repair
in
the
other
patients.
Mortality
from
cardiac
causes
was
12%
(15
cases);
12
patients
could
not
be
weaned
off
the
CPB
because
of
intractable
cardiac
dysfunction
and
2
died
postoperatively
of
low
cardiac
output
on
postoperative
days
8
and
15
respectively.
Permanent
neurologic
damage
with
cerebral
death
occurred
in
9
(7%)
patients.
Sepsis
complicated
by
multi-organ
system
failure
(specifically
renal
and
respiratory
failures),
was
the
cause
of
death
in
10
(8%)
patients.
Multiple
reoperation
for
bleeding
were
required
in
9
(8%)
other
patients.
Intravascular
disseminated
coagulation
(DIC)
in
its
different
phases
was
present
in
all
patients
from
the
time
of
admission.
Despite
aggressive
management
and
routine
blood
coagulation
tests,
coagulation
factor
levels
and
fibrinol:
vsin
remained
abnormal
for
the
duration
of
CPB.
Factor
V,
factor
VIII,
Fibrin
degradation
products
(FDP),
antithrombin
III,
D-dimer
levels,
and
platelet
counts
were
the
most
evident
defects
before,
during,
and
after
CPB
and
in
the
postoperative
period.
Prolonged
postoperative
inotropic
support
for
low
cardiac
output
was
required
in
34
patients.
Respiratory
failure
necessitating
tracheostomy
for
prolonged
assisted
ventilation
occurred
in
39
patients,
of
whom
9
died
of
sepsis
before
hospital
discharge.
Stroke
with
neurologic
damage
complicated
the
postoperative
course
of
8
(7%)
patients.
Five
patients
required
hemodialysis
treatment.
The
presence
of
renal
failure
in
the
postoperative
period
was
associated
with
death
in
all
patients
with
this
complication.
The
mean
duration
of
hospital
stay
was
38
days
with
an
average
of
10
days
in
ICU.
Late
Mortality:
Six
patients
who
had
preoperative
moderate
COPD
required
prolonged
ventilator
weaning
and
were
discharged
from
ICU
from
32
days
to
44
days
afterwards.
Of
these,
3
died
of
pneumonia
later
on
and
the
remaining
succumbed
to
malignant
arrhythmias
during
re-hospitalization
later
on
for
respiratory
failure.
One
patient
who
had
post
operative
renal
failure
died
of
cardiac
arrest
during
dialysis
5
months
after
the
operation.
Statistical
analysis
The
two
procedure
groups
examined
(right
thoracotomy
vs.
median
sternotomy)
were
not
significantly
different
from
each
other
with
respect
to
the
majority
of
perioperative
characteristics
that
are
believed
to
have
an
impact
on
outcome
in
patients
with
malfunctioning
prosthetic
mitral
valve
(Tables
1
and
2).
As
indicated
by
univariate
analysis,
perioperative
patient
variables
correlated
to
operative
mortality
were
median
sternotomy
(P<0.001),
bleeding
(P<0.001),
and
cardiac
ischemia
(P=0.02).
For
morbidity,
univariate
analysis
indicated
the
following
significant
variables:
median
sternotomy
(P<0.0001),
and
preoperative
myocardial
ischemia
(P=0.05).
Mortality
and
morbidity
models
based
on
multivariate
logistic
regression
analysis
confirmed
that
median
sternotomy
(as
a
continuous
variable)
is
by
far
the
most
important
risk
variable.
In
recent
years,
technical
improvement
in
emergency
redo
mitral
valve
operation
for
malfunctioning
prosthetic
mitral
valves,
associated
with
better
perioperative
management
and
postoperative
care
of
the
patient,
has
resulted
in
an
acceptable
decline
in
hospital
mortality
rate.
In
our
hospital,
the
results
obtained
in
right
thoracotomy
incision
without
cross
clamping
of
the
aorta
(Tables
1
to
3)
confirm
these
achievements.
The
dismal
outcome
that
we
have
observed
in
patients
with
median
sternotomy
with
the
cross
clamping
of
the
aorta
indicates
that
the
procedure
and
the
consequent
cross
clamping
of
the
aorta
further
exposes
this
population
to
the
risk
of
complicated
outcomes.
Median
sternotomy
patients
have
higher
hospital
mortality
and
more
complications,
even
though
preoperative
differences
between
the
two
procedural
groups
are
trivial.
This
is
particularly
the
case
for
the
variable
found
to
be
critical
in
the
statistical
model
of
mortality
and
morbidity
elaborated
in
this
study.
The
same
models
indicate
that
many
preoperative
factors
traditionally
associated
with
a
poor
outcome
such
as
renal
insufficiency,
stroke,
cardiac
insufficiency
and
chronic
obstructive
pulmonary
disease,
do
not
serve
here
as
predictors
of
mortality
and
morbidity,
thus
confirming
the
advances
made
in
the
management
of
patients
with
acute
malfunctioning
mitral
valve.
The
critical
influence
of
median
sternotomy
as
the
most
important
variable
on
the
postoperative
outcome
is
demonstrated
by
our
study.
From
a
statistical
point
of
view,
the
variable
“redo
median
sternotomy
with
cross-clamping
of
aorta
“condenses
a
variety
of
factors
that
are
very
difficult
to
categorize
and
quantify”
.
These
include
physiologic
and
pathologic
factors
related
to
the
normal
degenerative
processes
of
tissues
that
are
beyond
the
control
of
the
surgeon.
As
such,
significant
reductions
in
mortality
rates
appear
very
difficult
to
achieve.
Our
study
corroborates
the
hypothesis
that
median
sternotomy
with
the
cross-clamping
of
the
aorta
goes
beyond
the
limits
of
surgery
in
very
ill
patients,
unlike
other
cardiac
operations,
which
can
be
performed
via
right
thoracotomy
without
arresting
the
heart
with
a
high
risk
but
with
a
favorable
long-term
outcome.
In
this
era
of
diminishing
economic
resources
for
health
care,
the
question
of
whether
such
a
new
approach
of
surgical
therapy
should
be
offered
to
these
patients
is
very
relevant.
Society
must
always
face
the
reality
of
limited
medical
resources
and
must
find
mechanisms
for
distributing
these
resources
fairly
and
efficiently.
In
recent
years
the
focus
for
the
evaluation
of
health
services
has
shifted
from
unnecessary
treatment,
especially
unnecessary
surgery,
to
the
appropriateness
of
the
treatment.
Treatments
that
are
extremely
unlikely
to
be
beneficial
and
are
extremely
costly
may
be
considered
inappropriate
and
hence
inadvisable,
but
they
should
not
be
labeled
futile.
Three
sources
of
value
are
defined
that
give
meaning
to
“appropriateness”
in
patient
care:
the
clinical
point
of
view,
the
point
of
view
of
each
individual
patient,
and
the
societal
point
of
view(4).
These
concepts
necessitate
that
the
ethical
and
economic
implications
of
medical
services
be
integrated
into
outcome-based
guidelines.
The
aim
of
this
study
was
to
examine
whether
surgery
for
redo
mitral
valve
malfunction
in
critically
ill
patients
via
median
sternotomy
and
arresting
the
heart
is
beneficial
to
this
population.
In
light
of
the
data
presented,
we
conclude
that
such
surgical
treatment
is
inappropriate
while
right
thoracotomy
without
cross-clamping
the
aorta
remains
our
other
option.
In
all
these
cases
the
surgeon
is
emotionally
and
ethically
involved.
As
stated
by
Daniel
J.
Ullyot(5)
the
appropriate
application
of
technology
begins
early
in
the
clinical
encounter.
Very
often,
in
the
presence
of
very
ill
subjects,
what
appears
as
inappropriate
is
to
refer
the
patient
for
surgery.
A
surgical
consultation
offers
the
patient
more
than
the
simple
agreement
to
do
the
procedure,
because
it
creates
expectations
in
the
patient
or
patient’s
family,
making
the
decision
how
to
operate
extremely
difficult.
So
that
these
difficulties
can
be
overcome,
practice
guidelines
based
on
scientific
data
need
to
be
written.
The
present
work
aims
to
provide
a
small
contribution
to
this
commitment.
1.
Kirsch
M,
Guesnier
L,
Le
Besnerais
P,
Hillion
ML,
et
al.
Cardiac
operations
in
octogenarians:
Preoperative
risk
factors
for
death
and
impaired
autonomy
:
V.
Ann
Thorac
Surg
1998
;
66
:
60-7.
2.
Tsai
TP,
Matloff
JM,
Gray
RJ
et
al.
Cardiac
surgery
in
the
octogenarian
J
Thorac
Cardiovasc
Surg
1986
;
91
:
924-8.
3.
Tsai
TP.
Chaux
A,
Matlofr
JM,
et
al.
Ten-year
experience
of
cardiac
surgery
in
patients
aged
80
years
and
over.
Ann
Thorac
Surg
1994
;
58
:
445-50.
4.
Consensus
statement
of
the
society
of
critical
care
medicine’s
treatments.
Critcare
Med
1997
;
25
:
887-91.
5.
Ullyot
DJ.
The
assault
on
specialty
medicine
and
the
modern
surgeon.
J
Thorac
Cardiovascular
Surg
1998;
115:
273-80.
6.
Szefher
J.
Control
and
treatment
of
homeostasis
in
cardiovascular
surgery:
The
experience
of
La
Pitie
Hospital
with
patients
on
total
artificial
heart.
Int
J
Artif
Organs
1995;
18:633-
48.
7.
Morales
D,
Williams
E,
John
R.
Is
resternotomy
in
cardiac
surgery
still
a
problem?
Interact
cardiovasc
Thorac
Surg
2010;11:
277-86
[pubMed]
8.
Thompson
MJ,
Behranwala
A
et
al.
Immediate
and
long-term
results
of
mitral
prosthetic
replacement
using
a
right
thoracotomy
beating
heart
technique.
Eurjcardiothorac
surg
2003
;
24
:
47-51
;
discussions
51
[pubMed]
9.
Salhiyyah
K,
Taggart
D.
Beating-heart
valve
surgery:
A
systemic
review.
Asian
Cardiovas
Thorac
Ann
2009;
17:
650-8
[pubMed]
10.
Botta
L,
Cannata
A,
et
al.
Beating
heart
mitral
valve
surgery:
innovation
or
back
to
the
past?
J
Car
Surg
2010;
25:
318:
author
reply
318-9
[pubMed]
11.
Romano
MA,
haft
JW
et
al.
Beating
heart
surgery
via
right
thoracotomy
for
reoperative
mitral
valve
surgery
;
a
safe
and
effective
operative
alternative.
J
thome
Cardiovasc
Surg
2012;144
:
334-9
[pubMed]
12.
Holzhey
PM,
Shi
W.
et
al.
Minimally
invasive
versus
sternotomy
approach
for
mitral
valve
surgery
in
patients
greater
than
70
years
old:
a
propensity-matched
comparison.
Ann
Thorac
Surg
2011;
91:401-5
[PubMed]
|
|
.................................................................................................................

|
| |
|

