|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor)
DOI:10.5742/MEWFM.2019.93610
|
........................................................
|
|
Editorial
Dr.
Abdulrazak Abyad
DOI: 10.5742/MEWFM.2019.93623
Original Contribution
Self-monitoring
of Blood Glucose Among Type-2 Diabetic Patients:
An Analytical Cross-Sectional Study
[pdf]
Ahmed S. Alzahrani, Rishi K. Bharti, Hassan
M. Al-musa, Shweta Chaudhary
DOI: 10.5742/MEWFM.2019.93624
White
coat hypertension may actually be an acute phase
reactant in the body
[pdf]
Mehmet Rami Helvaci, Orhan Ayyildiz, Orhan Ekrem
Muftuoglu, Mehmet Gundogdu, Abdulrazak Abyad,
Lesley Pocock
DOI: 10.5742/MEWFM.2019.93625
Case Report
An
Unusual Persistent Mullerian Duct Syndrome in
a child in Abha city: A Case Report
[pdf]
Youssef Ali Mohamad Alqahtani, Abdulrazak Tamim
Abdulrazak, Hessa Gilban, Rasha Mirdad, Ashwaq
Y. Asiri, Rishi Kumar Bharti, Shweta Chaudhary
DOI: 10.5742/MEWFM.2019.93628
Population and Community
Studies
Prevalence
of abdominal obesity and its associated comorbid
condition in adult Yemeni people of Sana’a
City
[pdf]
Mohammed Ahmed Bamashmos
DOI: 10.5742/MEWFM.2019.93626
Smoking
may even cause irritable bowel syndrome
[pdf]
Mehmet Rami Helvaci, Guner Dede, Yasin Yildirim,
Semih Salaz, Abdulrazak Abyad, Lesley Pocock
DOI: 10.5742/MEWFM.2019.93629
Systematic
literature review on early onset dementia
[pdf]
Wendy Eskine
DOI: 10.5742/MEWFM.2019.93627
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
AUSTRALIA
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| March 2019 - Volume
17, Issue 3 |
|
|
Smoking may even cause irritable
bowel syndrome
Mehmet Rami Helvaci
(1)
Guner Dede (2)
Yasin Yildirim (2)
Semih Salaz (2)
Abdulrazak Abyad (3)
Lesley Pocock (4)
(1) Specialist of Internal Medicine, MD
(2) General practitioner, MD
(3) Middle-East Academy for Medicine of Aging,
MD
(4) medi-WORLD International
Corresponding
author:
Mehmet
Rami Helvaci, MD
07400, ALANYA, Turkey
Phone: 00-90-506-4708759
Email: mramihelvaci@hotmail.com
|
Abstract
Background: Smoking induced chronic
vascular endothelial inflammation may
even cause irritable bowel syndrome (IBS).
Method: IBS is diagnosed according
to Rome II criteria in the absence of
red flag symptoms.
Results: The study included 647
patients with IBS and 340 control cases.
Mean age of the IBS patients was 41.4
years. Interestingly, 64.2% of the IBS
patients were female. Prevalence of smoking
was higher in the IBS cases (36.4% versus
20.5%, p<0.001). Similarly, prevalence
of antidepressants use was higher in the
IBS patients (48.0% versus 15.5%, p<0.001).
Additionally, prevalence of urolithiasis
was also higher in the IBS group (23.3%
versus 9.4%, p<0.001). Mean body mass
index values were similar in the IBS and
control groups (27.5 versus 27.7 kg/m2,
p>0.05, respectively). Prevalence of
white coat hypertension was also similar
in them (29.3% versus 31.4%, p>0.05,
respectively). Although prevalence of
hypertension and diabetes mellitus and
mean values of total cholesterol, triglycerides,
low density lipoproteins, and high density
lipoproteins were all similar in them,
mean value of fasting plasma glucose (FPG)
was significantly higher in the IBS group
(110.1 versus 105.6 mg/dL, p= 0.013).
Conclusion: IBS may be a low-grade
inflammatory process being initiated with
infection, inflammation, psychological
disturbances-like stresses, and eventually
terminates with dysfunctions of gastrointestinal
and genitourinary tracts and other systems
of the body. Although there may be several
possible causes of IBS, smoking induced
chronic vascular endothelial inflammation
may even cause IBS. The higher FPG in
the IBS patients should be researched
with further studies.
Key words:
Smoking, irritable bowel syndrome,
metabolic syndrome, fasting plasma glucose
|
One of most frequent applications to Internal
Medicine Polyclinics are due to recurrent upper
abdominal discomfort (1). Although gastroesophageal
reflux disease, esophagitis, duodenal or gastric
ulcers, erosive gastritis or duodenitis, celiac
disease, chronic pancreatitis, and malignancies
are found among possible causes, irritable bowel
syndrome (IBS) may be one of the most frequently
diagnosed diseases, clinically. Flatulence,
periods of diarrhea or constipation, repeated
toilet visits due to urgent evacuation or early
filling sensation, excessive straining, feeling
of incomplete evacuation, frequency, urgency,
reduced feeling of well-being, and eventually
disturbed social life are often reported by
the IBS patients. Although many patients relate
onset of symptoms to intake of food, and often
incriminate specific food items, a meaningful
dietary role is doubtful in the IBS. According
to literature, 10-20% of the general population
have IBS, and it is more common among females
with unknown causes (2). Psychological factors
seem to precede onset or exacerbation of gut
symptoms, and many potentially psychiatric disorders
including anxiety, depression, or sleep disorders
frequently coexist with the IBS (3). For example,
thresholds for sensations of initial filling,
evacuation, urgent evacuation, and utmost tolerance
recorded via a rectal balloon significantly
decreased by focusing the examiners' attention
on gastrointestinal stimuli by reading pictures
of gastrointestinal malignancies in the IBS
cases (4). So although IBS is described as a
physical instead of a psychological disorder
according to Rome II guidelines, psychological
factors may be crucial for triggering of the
physical changes in the body. IBS is actually
defined as a brain-gut dysfunction according
to the Rome II criteria, and it may have more
complex mechanisms affecting various systems
of the body with a low-grade inflammatory state
(5). For example, IBS may even terminate with
chronic gastritis, urolithiasis, and hemorrhoid
in a significant proportion of patients (6-8).
Similarly, some authors studied the role of
inflammation via colonic biopsies in 77 patients
with IBS (9). Although 38 patients had normal
histology, 31 patients demonstrated microscopic
inflammation and eight patients fulfilled criteria
for lymphocytic colitis. However, immunohistology
revealed increased intraepithelial lymphocytes
as well as increased CD3 and CD25 positive cells
in lamina propria of the group with "normal"
histology. These features were more evident
in the microscopic inflammation group who additionally
revealed increased neutrophils, mast cells,
and natural killer cells. All of these immunopathological
abnormalities were the most evident in the lymphocytic
colitis group who also demonstrated HLA-DR staining
in the crypts and increased CD8 positive cells
in the lamina propria (9). A direct link between
the immunologic activation and IBS symptoms
was provided by work of some other authors (10).
They demonstrated not only an increased incidence
of mast cell degranulation in the colon but
also a direct correlation between proximity
of mast cells to neuronal elements and pain
severity in the IBS (10). In addition to these
findings, there is some evidence for extension
of the inflammatory process behind the mucosa.
Some authors addressed this issue in 10 patients
with severe IBS by examining full-thickness
jejunal biopsies obtained via laparoscopy (11).
They detected a low-grade infiltration of lymphocytes
in myenteric plexus of nine patients, four of
whom had an associated increase in intraepithelial
lymphocytes and six demonstrated evidence of
neuronal degeneration. Nine patients had hypertrophy
of longitudinal muscles and seven had abnormalities
in number and size of interstitial cells of
Cajal. The finding of intraepithelial lymphocytosis
was consistent with some other reports in the
colon (9) and duodenum (12). On the other hand,
smoking is a well-known cause of chronic vascular
endothelial inflammation all over the body.
We tried to understand whether or not smoking
induced chronic vascular endothelial inflammation
all over the body is found among one of the
possible causes of the IBS.
The
study
was
performed
in
the
Internal
Medicine
Polyclinic
of
the
Dumlupinar
University
between
August
2005
and
March
2007.
Consecutive
patients
with
upper
abdominal
discomfort
were
taken
into
the
study.
Their
medical
histories
including
smoking
habit,
hypertension
(HT),
diabetes
mellitus
(DM),
and
already
used
medications
including
antidepressants
at
least
for
a
period
of
six
months
were
learned.
A
routine
check
up
procedure
including
fasting
plasma
glucose
(FPG),
triglycerides,
low
density
lipoproteins
(LDL),
high
density
lipoproteins
(HDL),
erythrocyte
sedimentation
rate,
C-reactive
protein,
albumin,
thyroid
function
tests,
creatinine,
urinalysis,
hepatic
function
tests,
markers
of
hepatitis
A
virus,
hepatitis
B
virus,
hepatitis
C
virus,
and
human
immunodeficiency
virus,
a
posterior-anterior
chest
x-ray
film,
an
electrocardiogram,
a
Doppler
echocardiogram
in
case
of
requirement,
an
abdominal
ultrasonography,
an
abdominal
X-ray
graphy
in
supine
position,
and
a
questionnaire
for
IBS
was
performed.
IBS
is
diagnosed
according
to
Rome
II
criteria
in
the
absence
of
red
flag
symptoms
including
pain
and
diarrhea
that
awakens/interferes
with
sleep,
weight
loss,
fever,
and
abnormal
physical
examination
findings.
An
additional
intravenous
pyelography
was
performed
just
in
suspected
cases
from
presenting
urolithiasis
as
a
result
of
the
urinalysis
and
abdominal
X-ray
graphy.
So
urolithiasis
was
diagnosed
either
by
medical
history
or
as
a
result
of
clinical
findings.
Patients
with
a
history
of
eating
disorders
including
anorexia
nervosa,
bulimia
nervosa,
compulsive
overeating,
or
binge
eating
disorder,
insulin
using
diabetics,
and
patients
with
devastating
illnesses
including
malignancies,
acute
or
chronic
renal
failure,
cirrhosis,
hyper-
or
hypothyroidism,
and
heart
failure
were
excluded
to
avoid
their
possible
effects
on
weight.
Current
daily
smokers
at
least
for
six
months
and
cases
with
a
history
of
five
pack-year
were
accepted
as
smokers.
Body
mass
index
(BMI)
of
each
case
was
calculated
by
the
measurements
of
the
same
physician
instead
of
verbal
expressions.
Weight
in
kilograms
is
divided
by
height
in
meters
squared
(13).
Cases
with
an
overnight
FPG
level
of
126
mg/dL
or
higher
on
two
occasions
or
already
using
antidiabetic
medications
were
defined
as
diabetics.
An
oral
glucose
tolerance
test
with
75
grams
glucose
was
performed
in
cases
with
FPG
levels
between
100
and
126
mg/dL,
and
diagnosis
of
cases
with
2-hour
plasma
glucose
levels
of
200
mg/dL
or
higher
is
DM
(13).
Office
blood
pressure
(OBP)
was
checked
after
a
5-minute
rest
in
seated
position
with
mercury
sphygmomanometer
on
three
visits,
and
no
smoking
was
permitted
during
the
previous
2
hours.
Ten-day
twice
daily
measurements
of
blood
pressure
at
home
(HBP)
were
obtained
in
all
cases,
even
in
normotensives
in
the
office
due
to
the
risk
of
masked
HT
after
a
10-minute
education
session
about
proper
blood
pressure
(BP)
measurement
techniques
(14).
The
education
included
recommendation
of
upper
arm
while
discouraging
wrist
and
finger
devices,
using
a
standard
adult
cuff
with
bladder
sizes
of
12
x
26
cm
for
arm
circumferences
up
to
33
cm
in
length
and
a
large
adult
cuff
with
bladder
sizes
of
12
x
40
cm
for
arm
circumferences
up
to
50
cm
in
length,
and
taking
a
rest
at
least
for
a
period
of
5
minutes
in
the
seated
position
before
measurements.
An
additional
24-hour
ambulatory
blood
pressure
monitoring
(ABP)
was
not
required
due
to
an
equal
efficacy
of
the
method
with
HBP
measurement
to
diagnose
HT
(15).
Eventually,
HT
is
defined
as
a
mean
BP
of
140/90
mmHg
or
higher
on
HBP
measurements
and
white
coat
hypertension
(WCH)
is
defined
as
an
OBP
of
140/90
mmHg
or
higher,
but
a
mean
HBP
value
of
lower
than
140/90
mmHg
(14).
Eventually,
all
patients
with
the
IBS
were
collected
into
the
first
and
age
and
sex-matched
controls
were
collected
into
the
second,
groups.
Mean
BMI,
FPG,
total
cholesterol
(TC),
triglycerides,
LDL,
and
HDL
values
and
prevalences
of
smoking,
antidepressants
use,
urolithiasis,
WCH,
HT,
and
DM
were
detected
in
each
group
and
compared
in
between.
Mann-Whitney
U
test,
Independent-Samples
T
test,
and
comparison
of
proportions
were
used
as
the
methods
of
statistical
analyses.
The
study
included
647
patients
with
the
IBS
and
340
control
cases,
totally.
The
mean
age
of
the
IBS
patients
was
41.4
±
14.4
(15-86)
years.
Interestingly,
64.2%
(416)
of
the
IBS
patients
were
female.
Prevalence
of
smoking
was
significantly
higher
in
cases
with
the
IBS
(36.4%
versus
20.5%,
p<0.001).
Similarly,
prevalence
of
antidepressants
use
was
higher
in
cases
with
the
IBS
(48.0%
versus
15.5%,
p<0.001).
Beside
that
prevalence
of
urolithiasis
was
also
higher
in
the
IBS
group
(23.3%
versus
9.4%,
p<0.001).
Mean
BMI
values
were
similar
both
in
the
IBS
and
control
groups
(27.5
versus
27.7
kg/m2,
p>0.05,
respectively).
Additionally,
prevalence
of
WCH
was
similar
in
both
groups,
too
(29.3%
versus
31.4%,
p>0.05,
respectively).
Although
prevalence
of
HT
and
DM
and
mean
values
of
TC,
triglycerides,
LDL,
and
HDL
were
all
similar
in
both
groups
(p>0.05
for
all),
mean
value
of
FPG
was
significantly
higher
in
the
IBS
group
with
unknown
reasons,
yet
(110.1
versus
105.6
mg/dL,
p=
0.013)
(Table
1).
Table
1:
Comparison
of
patients
with
irritable
bowel
syndrome
and
control
cases
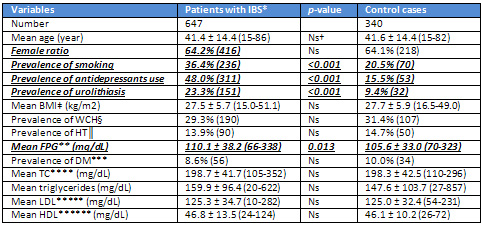 *Irritable
bowel
syndrome
†Nonsignificant
(p>0.05)
‡Body
mass
index
§White
coat
hypertension
?Hypertension
**Fasting
plasma
glucose
***Diabetes
mellitus
****Total
cholesterol
*****Low
density
lipoproteins
******High
density
lipoproteins *Irritable
bowel
syndrome
†Nonsignificant
(p>0.05)
‡Body
mass
index
§White
coat
hypertension
?Hypertension
**Fasting
plasma
glucose
***Diabetes
mellitus
****Total
cholesterol
*****Low
density
lipoproteins
******High
density
lipoproteins
| | |

