|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor)
DOI:10.5742/MEWFM.2019.93610
|
........................................................
|
|
Editorial
Dr.
Abdulrazak Abyad
DOI: 10.5742/MEWFM.2019.93623
Original Contribution
Self-monitoring
of Blood Glucose Among Type-2 Diabetic Patients:
An Analytical Cross-Sectional Study
[pdf]
Ahmed S. Alzahrani, Rishi K. Bharti, Hassan
M. Al-musa, Shweta Chaudhary
DOI: 10.5742/MEWFM.2019.93624
White
coat hypertension may actually be an acute phase
reactant in the body
[pdf]
Mehmet Rami Helvaci, Orhan Ayyildiz, Orhan Ekrem
Muftuoglu, Mehmet Gundogdu, Abdulrazak Abyad,
Lesley Pocock
DOI: 10.5742/MEWFM.2019.93625
Case Report
An
Unusual Persistent Mullerian Duct Syndrome in
a child in Abha city: A Case Report
[pdf]
Youssef Ali Mohamad Alqahtani, Abdulrazak Tamim
Abdulrazak, Hessa Gilban, Rasha Mirdad, Ashwaq
Y. Asiri, Rishi Kumar Bharti, Shweta Chaudhary
DOI: 10.5742/MEWFM.2019.93628
Population and Community
Studies
Prevalence
of abdominal obesity and its associated comorbid
condition in adult Yemeni people of Sana’a
City
[pdf]
Mohammed Ahmed Bamashmos
DOI: 10.5742/MEWFM.2019.93626
Smoking
may even cause irritable bowel syndrome
[pdf]
Mehmet Rami Helvaci, Guner Dede, Yasin Yildirim,
Semih Salaz, Abdulrazak Abyad, Lesley Pocock
DOI: 10.5742/MEWFM.2019.93629
Systematic
literature review on early onset dementia
[pdf]
Wendy Eskine
DOI: 10.5742/MEWFM.2019.93627
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
AUSTRALIA
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| March 2019 - Volume
17, Issue 3 |
|
|
An Unusual Persistent Mullerian
Duct Syndrome in a child in Abha city: A Case
Report
Youssef Ali Mohamad Alqahtani
(1)
Abdulrazak Tamim Abdulrazak (2)
Hessa Gilban (3)
Rasha Mirdad (4)
Ashwaq Y. Asiri (5)
Rishi Kumar Bharti (6)
Shweta Chaudhary (7)
(1) Assistant Professor of Paediatrics, Child
Health Department, College of Medicine,
King Khalid University, Abha, Kingdom of Saudi
Arabia
(2) Pediatric Surgery Resident, Abha Maternity
and Children Hospital, Abha, K.S.A
(3) Pediatric Consultant, Abha Maternity and
Children Hospital, Abha, Kingdom of Saudi Arabia
(4) Medical Student, College of Medicine, King
Khalid University, Abha, Kingdom of Saudi Arabia
Demonstrator, Surgery Department, College of
Medicine, Abha, Kingdom of Saudi Arabia
(6) Assistant Professor and Consultant, Family
& Community Medicine Department, College
of Medicine, King Khalid University, Abha, Saudi
Arabia.
(7) Assistant Professor, Anatomy Department,
College of Medicine, King Khalid University,
Abha, Saudi Arabia.
Corresponding author:
Dr. Youssef Ali Mohamad Alqahatni
College of Medicine,
King Khalid University,
Abha, Kingdom of Saudi Arabia
Contact No.: +966554736556
Email: youssefalqahtani641@gmail.com
|
Abstract
Background:
Persistent Mullerian duct syndrome (PMDS)
is a rare condition that is characterized
by the presence of the Mullerian duct
structures and is phenotypically and genotypically
male. It could result from insufficiency
of Mullerian inhibiting factor (MIF) or
its receptors.
Case presentation: A 9 month-old
Syrian boy was admitted to Abha Maternity
and Children Hospital with a previous
history of a huge left inguinal swelling
since 8 hours, vomiting 4 times, and with
yellowish discharge. Routine examinations
and investigations were done and the boy
was diagnosed with left unilateral inguinal
hernia with obstruction and during surgery
left ovotestis with fallopian tubes and
rudimentary uterus were detected. The
histopathology showed no signs of malignancy.
After two weeks from left inguinal hernia
repair, the boy presented with right incarcerated
hernia. The boy underwent right inguinal
herniotomy and right gonadopexy. During
the operation, right ovotestis, with vas
and fallopian tube were detected. The
tube was resected and the sac was dissected;
vas and vessels were secured. The boy
had no sexual dysfunction and chromosomal
investigation showed normal male karyotype.
The testosterone level was less than the
normal range (0.087 nmol/l).
Conclusion: The PMDS is a rare
condition and during early stages cannot
be detected; the only diagnostic procedure
is when the children are tested for other
diseases such as hernia or cryptorchidism.
The correct and early diagnosis depends
on genetic investigation and endocrinology.
Surgery is the treatment of choice.
Key words: Persistent Mullerian
duct syndrome (PMDS), Obstructed inguinal
hernia, male, Mullerian inhibiting factor,
Mullerian duct derivatives.
|
Persistent Mullerian duct syndrome (PMDS) is
a rare condition that has presented in only
150 cases in the literature (1). It is characterized
by the presence of the Mullerian duct structures
and is phenotypically and genotypically male
but the exact etiology is still a debate. It
could result from insufficiency of Mullerian
inhibiting factor (MIF) or its receptors(2).
The PMD patients are supposed to have normal
genitalia and sexual characteristics. Among
males, inguinal hernia is characterized by descending
of the testis and presence of inguinal hernia.
The second type of PMD is ectopia and hernia
of both testis (3, 4).
Most of the inguinal hernias present in the
groin (75%). Hernias have many complications
including obstruction of the bowel and strangling
among older subjects(5). Also, ectopic testis
diagnosed among PMD patient could result in
cryptorchidism among males. The tumors of the
testicular germ cell tumors have been reported
but are very rare among the Mullerian duct derivatives.
If the patients was diagnosed to be phenotypically
male, tumor and PMD are not suspected until
the time of surgery for hernia repair or treatment
of cryptorchidism(6, 7).
A
9
months-old
Syrian
boy
was
admitted
to
Abha
Maternity
and
Children
Hospital
with
a
previous
history
of
huge
left
inguinal
swelling
since
8
hours,
vomiting
4
times,
yellowish
discharge
and
these
symptoms
arre
the
most
common
symptoms
of
persistent
inguinal
hernia
according
to
the
literature
review(6,
7).
Routine
examinations
and
investigations
were
normal.
No
history
of
medical
chronic
condition,
surgical
operation,
allergy
to
medications
was
present
and
he
was
diagnosed
with
left
unilateral
inguinal
hernia
with
obstruction
and
the
patient
was
prepared
for
surgery.
The
child
had
urgent
left
inguinal
herniotomy,
gonadopexy
and
diagnostic
laparoscopy
after
3
days
of
admission.
During
operation
there
was
left
and
right
ovotestis
with
fallopian
tubes
and
rudimentary
uterus;
thus
the
boy
was
referred
for
consultation
in
the
OPD
after
2
weeks
(Figure
1).
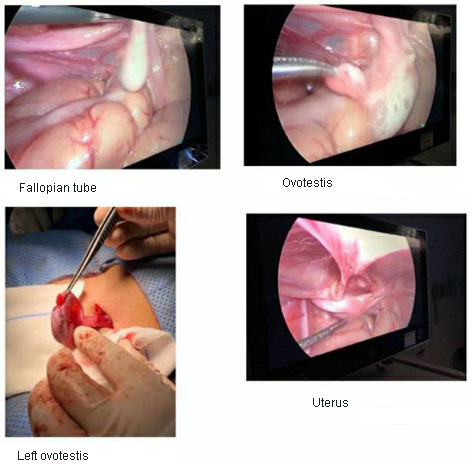
Figure
1
The
histopathology
of
the
tissue
from
the
left
fibroid
and
vas
side
of
the
testis
showed
normal
testis
composed
of
capsule,
lobule
and
convoluted
seminiferous
tubules.
The
tubules
were
enclosed
by
thick
basal
lamina
surrounded
by
muscles
cells.
The
tubules
contained
spermatogenic
cells
and
Sertoli
cells.
No
malignancy
was
seen.
At
discharge,
the
HB
was
9.7
mg/dl,
WBCs
were
6.87x103
and
normal
UE.
After
two
weeks
from
left
inguinal
hernia
repair,
the
boy
presented
with
right
incarcerated
hernia.
The
boy
underwent
right
inguinal
herniotomy
and
right
gonadopexy.
During
the
operation,
right
ovotestis,
with
vas
and
fallopian
tube
were
found.
The
tube
was
resected
and
the
sac
was
dissected;
vas
and
vessels
were
secured.
2
biopsies
were
taken
from
the
vas
site
and
the
fimbrial
site.
The
boy
had
no
sexual
dysfunction
and
chromosomal
investigation
showed
normal
male
karyotype
46
XY.
The
testosterone
level
was
less
than
the
normal
range
(0.087
nmol/l).
The
ALT
level
was
within
normal
range,
Fe,
BUN
and
creatinine
were
lower
than
the
normal
range
and
complete
blood
picture
was
done.
The
pathological
report
showed
immature
testicular
tissue
with
no
signs
of
malignancy.
| | |

