|
|
 |
Medicine and Society
........................................................
Case Report
........................................................
Continuing Education
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| January 2015 -
Volume 13 Issue 1 |
|
Women's
health Aspect In Humanitarian Missions And Disasters:
Jordanian Royal Medical Services Experience
Fatima
Al-Odwan
Suhair Wreikat
Specialist of obstetric and gynecology,
Royal Medical Services
Jordan
Correspondence:
Fatima Al-Odwan
Suhair Wreikat
Specialist of obstetric and gynecology,
Royal Medical Services
Jordan
Email: mkateeb@lycos.com
|
Abstract
Objective: To
review women's health problems in patients
who presented to Royal Medical Services
humanitarian missions over a 3 year period.
Design and method: Analysis of
humanitarian missions of RMS data and
records over three year period (2009-2011)
in regards to women's health issues, was
done. The data were analyzed in regards
to number of women seen, the presenting
conditions, and prevalence of domestic
violence in these cases.
Results: During
the 3 year period 72 missions were deployed
to 4 locations ( Gaza, Ram Allah -West
Bank, Jeneen-West Bank, and Iraq). Total
numbers of females seen in this period
was 86,436 women accounting for 56% of
adults patients seen by RMS humanitarian
missions. Acute injuries were responsible
for 32% of the cases, chronic diseases
for 52% and women's health issues for
the rest. Domestic violence was encountered
in 11% of the cases. Pregnancy related
problems were the main reason for presentation
(38%). Contraception was the second reason
for seeking help and was seen in 25% of
cases.
Conclusion: Women's
health care providers are needed to advise,
assist, and support public health authorities
in planning for and serving during a disaster.
Emergency preparedness is essential to
maintaining healthy pregnancies and ensuring
good outcomes for pregnant women and their
infants who endure disasters.
Key words: women's
health problems, humanitarian missions,
Royal Medical Services(RMS).
|
Gender can also place women and men at different
risks of disaster. Women suffer in the aftermath
of disasters when social networks are frayed,
when family and kin are displaced, and when
they feel the cumulative effects of caring for
others including for men and boys, are not well
served by disaster mental health care and facilities.
Examples from previous disaster events demonstrated
this gender difference: In 1976, in the technological
disaster of Seveso, Italy, the population was
exposed to dioxin. Biologic differences between
the sexes were seen: 15 years later, more men
died of rectal and lung cancer, whereas more
women died of diabetes. In the Indian Ocean
tsunami in 2004, the ratio of deaths between
women and men was 3:1 because men were stronger,
women had not learned to swim, and women's long
hair got entangled in debris.
In the 1993 earthquake in Maharashtra, India,
more women and children died than men because
the women were in the homes, whereas the men
were out in the fields. Conversely, social roles
determined that men were more affected than
women during the 1985 Chernobyl disaster. The
soldiers and male civilians predominantly cleaned
up the site and as a result were exposed to
more radiation. Cultural norms have prevented
women from seeking help after a disaster, especially
in certain regions where interacting with men
is strictly forbidden. (2) Social norms have
demonstrated that women bear more of the responsibility
of caring for children, elderly, and the sick
or injured.
Women also face an increased risk of domestic
violence: Studies have found that there are
many more calls to women's shelters as much
as year after an emergency, the aim of this
review is to study the effect on disasters on
women's health. Royal Medical Services has been
involved in more than 100 humanitarian missions
over the last 15 years in more than 15 locations
all over the world. The aim of this study is
to review women's health problems in patients
presented to RMS humanitarian missions over
a 3 year period.
Analysis of humanitarian
missions of RMS data and
records over a three year
period ( 2009-2011) in
regards to women health
issues was done. The data
were analyzed in regards
to number of women seen,
the presenting conditions,
and prevalence of domestic
violence in these cases.
During 3 years period
72 missions were deployed
to 4 locations ( Gaza,
Ram Allah -West Bank,
Jeneen-West Bank, and
Iraq).
Total number of females
seen in this period
was 86,436 women accounting
for 56% of adult patients
seen by RMS humanitarian
missions . Table 1 shows
the age distribution
of these women, and
Table 2 shows the presenting
conditions.
Table 1: Age of women
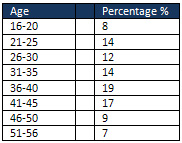
Table 2: Condition of
presentation
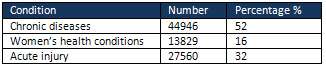
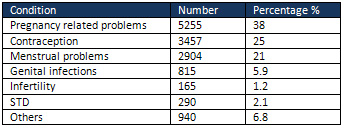
Table 3: Women's Health
condition
Acute injuries were
responsible for 32%
of the cases, chronic
diseases for 52%, and
women's health issues
for the rest. Domestic
violence was encountered
in 11% of the cases.
Pregnancy related problems
was the main reason
for presentation(38%).
Contraception was the
second reason for seeking
help and was seen in
25% of cases. Menstrual
related problems were
responsible for 21%
of cases, and genital
infections were responsible
for 8% of cases. Among
them STD was not prevalent
in the women who presented
(only 2.1%). Surprisingly
infertility problem
was the main cause of
presentation in 3% of
cases.
Pregnant
women,
newborns,
and
infants
may
be
disproportionately
harmed
by
natural
disasters.
The
lack
of
resources,
such
as
food
and
clean
water,
lack
of
access
to
health
care
and
medications,
as
well
as
psychologic
stress
in
the
aftermath
of
disasters
increase
pregnancy-related
morbidities.
After
Hurricane
Katrina,
the
Centers
for
Disease
Control
and
Prevention
found
that
the
14
Federal
Emergency
Management
Agency
designated
counties
and
parishes
affected
by
the
hurricane
had
a
significant
increase
in
the
number
of
women
who
received
late
or
no
prenatal
care.
In
the
designated
counties
in
Mississippi,
the
percentage
of
inadequate
prenatal
care
increased
significantly
from
2.3%
to
3.3%
(3).
In
Louisiana,
among
Hispanic
women,
it
increased
from
2.3%
to
3.9%
(3).
Infants
who
were
born
to
pregnant
women
living
within
a
2-mile
radius
of
the
World
Trade
Center
on
9/11
were
found
to
have
a
higher
rate
of
intrauterine
growth
restriction,
decreased
birth
weight,
and
a
small
head
circumference
.
In
a
study
that
monitored
birth
outcomes
following
Hurricane
Katrina,
women
who
experienced
three
or
more
severe
traumatic
situations
during
the
hurricane,
such
as
feeling
as
though
one's
life
was
in
danger,
walking
through
flood
waters,
or
having
a
loved
one
die,
were
found
to
have
a
higher
rate
of
low
birth
weight
infants
and
an
increase
in
preterm
deliveries.
Additionally,
disruption
of
the
health
care
system
may
result
in
the
separation
of
mothers
and
infants.
For
example,
during
Hurricane
Katrina,
many
critically
ill
hospitalized
infants
were
transported
to
medical
facilities
outside
of
New
Orleans
without
their
mothers.
The
separation
of
mothers
and
their
infants
can
interfere
with
breastfeeding
as
well
as
create
additional
stress
for
the
mothers.
These
pregnancy
morbidities
can
be
prevented
by
developing
an
emergency
plan
that
addresses
them.
As
providers
of
women's
health
care,
the
involvement
of
the
obstetrician-gynecologist
in
disaster
response
is
essential.
This
can
be
done
at
the
local
level
through
a
hospital
emergency
preparedness
committee
or
a
community
group
attached
to
the
fire
department
or
police
department
and
at
the
state
level.
Disaster
Preparedness
for
the
Health
Care
System
and
Providers
Caring
for
Pregnant
Women
Although
a
"one-size
fits
all"
emergency
plan
is
difficult
to
apply
to
all
disasters,
there
are
common
distresses
experienced
by
all
pregnant
women
regardless
of
the
nature
of
the
disaster.
Pregnant
women
should
be
encouraged
to
develop
evacuation
plans
in
the
event
there
is
enough
forewarning
to
allow
for
evacuation.
The
Red
Cross
provides
emergency
preparedness
checklists
for
specific
disasters.
However,
when
evacuation
is
not
possible,
the
health
care
for
women
in
the
antepartum,
intrapartum,
and
postpartum
periods
needs
to
be
safely
managed.
For
women
in
the
antepartum
period,
maintaining
prenatal
care
is
of
utmost
importance.
Health
care
providers
outside
the
perimeter
of
the
disaster
should
be
willing
to
accept
evacuees
in
an
effort
to
ensure
continuation
of
prenatal
care.
State
and
local
governments
should
establish
local
facilities
where
prenatal
care
and
obstetric
services
can
be
provided
for
those
women
unable
to
evacuate.
Accessing
prenatal
records
is
important
in
maintaining
prenatal
care.
This
will
be
impossible
if
written
records
are
destroyed
because
of
the
disaster
or
if
interruption
in
electricity
prohibits
access
to
electronic
medical
records.
In
preparation,
clinicians
should
make
patients
aware
of
their
specific
prenatal
issues
as
well
as
provide
them
with
key
portions
of
their
medical
records.
This
is
especially
true
in
areas
where
natural
disasters
are
seasonal
and
may
be
likely
to
occur.
Also,
health
care
providers
of
prenatal
care
should
increase
patients'
awareness
of
the
signs
of
preterm
labor
and
other
obstetric
emergencies
and
the
action
to
take
in
the
event
of
these
emergencies.
Obstetric
care
at
a
designated
facility
is
ideal,
and
it
is
the
role
of
public
health
officials
in
an
area
to
designate
and
equip
obstetric
care
facilities,
publicize
which
facilities
in
a
given
area
will
offer
obstetric
services,
identify
alternative
safe
delivery
sites,
and
arrange
for
the
staffing
of
the
facilities.
Individual
obstetric
care
providers
are
urged
to
assist
public
health
officials
and
to
practice
within
the
obstetric
care
system
that
is
established.
However,
there
are
several
factors
that
may
contribute
to
difficulty
in
accessing
obstetric
health
care
facilities
during
a
disaster.
The
health
care
system
may
become
inundated
with
other
health
emergencies,
which
could
decrease
the
resources
available
to
pregnant
women.
Also,
physical
barriers,
such
as
impassible
roads,
demolished
bridges
and
fire
lines,
may
serve
as
obstacles
to
accessing
obstetric
care
facilities.
These
hindrances
may
result
in
women
giving
birth
outside
of
health
care
facilities.
To
prepare,
clinicians
should
make
pregnant
women
who
reside
in
locations
subject
to
seasonal
or
frequent
environmental
emergencies
aware
of
the
availability
of
emergency
birth
kits
.
These
kits
have
all
of
the
essential
equipment
necessary
should
a
birth
occur
outside
of
a
birthing
facility.
During
a
disaster,
women
who
are
not
breastfeeding
may
have
difficulty
in
providing
food
for
their
newborns.
Some
new
mothers
may
plan
to
bottle-feed
their
newborns.
However,
during
a
disaster,
there
may
not
be
access
to
clean
water
for
sterilization
of
bottles
or
access
to
formula.
Encouraging
and
establishing
breastfeeding
as
a
part
of
routine
care
ensures
that
mothers
are
able
to
feed
their
newborns
in
the
event
of
a
disaster.
Additionally,
health
care
providers
should
be
educated
in
lactation
to
assist
new
mothers
in
initiating
breastfeeding
in
the
immediate
phase
of
a
disaster.
For
mothers
who
are
less
than
6
months
postpartum,
even
if
they
have
not
previously
established
lactation,
relactation
can
be
established
and
should
be
encouraged.
For
those
mothers
who
choose
not
to
begin
relactation
or
are
beyond
the
6-month
period,
ready-to-feed
infant
formula
in
a
single-serving
bottle
should
be
provided.
Disaster
Preparedness
for
the
Health
Care
System
and
Providers
Caring
for
Nonpregnant
Women
Providing
contraception
for
postpartum
and
nonpregnant
women
during
a
disaster
is
also
important
to
prevent
unintended
pregnancies.
Contraception
should
be
provided
in
the
form
of
emergency
contraception
as
well
as
prophylactic
contraception.
Providing
condoms
allows
for
the
prevention
of
not
only
unintended
pregnancies
but
also
decreases
the
transmission
of
sexually
transmitted
diseases.
For
women
who
are
using
reversible
contraception
in
the
form
of
pills,
the
ring,
or
the
patch,
these
prescription
medications
should
be
provided
to
enable
these
women
to
maintain
their
current
form
of
birth
control.
When
possible,
emergency
health
care
facilities
should
stock
and
dispense
a
variety
of
contraceptive
products.
Mental
Health
Considerations
Involvement
in
a
disaster
situation
causes
and
exacerbates
tremendous
anxiety,
depression,
and
grief.
Post-disaster,
patients
and
health
care
providers
need
to
be
aware
of
the
signs
of
mental
distress
requiring
medical
attention.
The
Centers
for
Disease
Control
and
Prevention
offers
information
and
resources
for
mental
health
care
during
and
after
disasters.
This
can
be
accessed
at
http://www.bt.cdc.gov/mentalhealth/.
Prevention
of
Violence
Against
Women
During
a
Disaster
Women
are
subjected
to
and
vulnerable
to
intimate
partner
violence
and
sexual
assault
during
disasters
(9,
10).
Similar
to
the
conditions
found
in
refugee
camps
where
sexual
violence
also
is
increased,
during
the
phases
of
a
disaster
women
are
isolated
from
their
families
and
without
physical
protection.
The
United
Nations
Refugee
Agency,
in
developing
guidelines
for
prevention
and
response
to
sexual
violence
against
refugees,
has
identified
some
contributing
circumstances:
1)
male
perpetrators'
dominance
over
female
victims,
2)
psychologic
strains
in
refugee
camps,
3)
absence
of
support
systems
for
protection,
4)
crowded
facilities,
5)
lack
of
physical
protection,
6)
general
lawlessness,
7)
alcohol
and
drug
abuse,
8)
politically
motivated
violence
against
refugees,
and
9)
single
females
separated
from
male
family
members
(5).
Ironically,
these
same
circumstances
existed
among
the
Hurricane
Katrina
evacuees
and
were
likely
responsible
for
the
many
personal
accounts
of
rape
that
occurred
in
evacuation
shelters.
Establishing
safety,
order,
and
the
rule
of
law
in
shelters
for
disaster
survivors
is
paramount
to
the
protection
of
women
from
sexual
assault.
In
the
event
that
sexual
violence
does
occur,
appropriate
and
sensitive
services
should
be
available
to
victims,
including
emergency
contraception
and
sexual
assault
forensic
examiners
or
sexual
assault
nurse
examiners.
Disasters are unplanned
but can be anticipated.
Emergency preparedness
is essential to maintaining
healthy pregnancies and
ensuring good outcomes
for pregnant women and
their infants who endure
disasters. Developing
an evacuation plan is
the first step. However,
if evacuation is not possible,
identifying local health
care facilities that can
provide obstetric care,
discussing the availability
of emergency birth kits,
and emphasizing the importance
of lactation are key steps
to facing the many challenges
of a disaster that are
unique to pregnant women.
Postpartum and nonpregnant
women must have access
to contraception. Women's
health care providers
are needed to advise,
assist, and support public
health authorities in
planning for and serving
during a disaster. Clinicians
also should encourage
local and state governments
to provide shelters that
are safe and secure to
prevent violence against
women.
1.
Toner
E,
Waldhorn
R,
Franco
C,
Courtney
B,
Rambhia
K,
Norwood
A,
Inglesby
TV,
O'Toole
T.
Hospitals
Rising
to
the
Challenge:
The
First
Five
Years
of
the
U.S.
Hospital
Preparedness
Program
and
Priorities
Going
Forward.
Prepared
by
the
Center
for
Biosecurity
of
UPMC
for
the
U.S.
Department
of
Health
and
Human
Services
under
Contract
No.
HHSO100200700038C.
2009.
2.
Women
and
Infants
Services
Package
(WISP),
from
the
National
Working
Group
for
Women
and
Infant
Needs
in
Emergencies,
White
Ribbon
Alliance.
Accessed
March
24,
2008
from
http://www.whiteribbonalliance.org/Resources/Documents/WISP
.Final.07.27.07.pdf.
3.
Hamilton
B,
Sutton
P,
Matthews
TJ,
Martin
J,
Ventura
S.
The
Effect
of
Hurricane
Katrina:
Births
in
the
U.S.
Gulf
Coast
Region,
Before
and
After
the
Storm.
National
Vital
Statistics
Report.
Vol
58,
No
2.
4.
Callaghan
W,
Rasmussen,
S,
Jamieson
D,
Ventura
S,
Farr
S,
Sutton
P,
Mathews,
T,
Hamilton
B,
Shealy
K,
Brantley
D,
Posner
S.
Health
Concerns
of
Women
and
Infants
in
Times
of
Natural
Disasters:
Lessons
Learned
from
Hurricane
Katrina.
Maternal
and
Child
Health
Journal.
2007;
11(4):
307-311.
5.
Lederman
SA,
Rauh
V,
Weiss
L,
Stein
JL,
Hoepner
LA,
Becker
M,
et
al.
The
effects
of
the
World
Trade
Center
event
on
birth
outcomes
among
term
deliveries
at
three
lower
Manhattan
hospitals.
Environ
Health
Perspect
2004;112:1772-8.
6.
Xiong
X,
Harville
E,
Mattison
D,
Elkind-Hirsch
K,
Pridjian
G,
Buekens
P.
Exposure
to
Hurricane
Katrina,
Post-Traumatic
Stress
Disorder
and
Birth
Outcomes.
Am
J
Med
Sci
2008
August;
336(2):
111-115.
doi:
10.1097/MAJ.
0b013e318180f21c.
7.
American
Red
Cross,
"Preparedness
Fast
Facts:
Emergency-Specific
Preparedness
Information".
Copyright
2009.
The
American
National
Red
Cross.
http://www.redcross.org/portal/site/en/menuitem.86f46a12f382290517a8f210b80f78a0/?vgnextoid=92d51a53f1c37110VgnVCM100
0003481a10aRCRD
8.
La
Leche
League
International,
"When
an
Emergency
Strikes
Breastfeeding
Can
Save
Lives,
Part
2,"
media
release,
September
1,
2005.
Accessed
October
3,
2006
from
http://www.lalecheleague.org/Release/emergency2.html
9.
United
Nations
High
Commissioner
for
Refugees
(UNHCR).
Prevention
and
Response
to
Sexual
and
Gender-Based
Violence
in
Refugee
Situations.
Proceedings
of
the
Inter-Agency
Lessons
Learned
Conference,
Geneva
(March
27-29,
2001).
Available
at:
http://action.web.ca/home/cpcc/attach/prevention%20and%20responses.pdf
10.
Thornton,
W.,
Voigt,
L.
"Disaster
Rape:
Vulnerability
of
Women
to
Sexual
Assaults
During
Hurricane
Katrina."
Journal
of
Public
Management
&
Social
Policy.
Fall
2007.
|
|
.................................................................................................................

|
| |
|

