|
|
 |
Medicine and Society
........................................................
Case Report
........................................................
Continuing Education
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| January 2015 -
Volume 13 Issue 1 |
|
Non-Compliance
to Antihypertensive Treatment among Patients Attending
Prince Zaid Military Hospital
Lana Sati Goussous
(1)
Nashat Ayoub Halasah (1)
Manhal Halasa (2)
(1) Royal medical
Services, Jordan
(2) Manhal Halasa, MD, Epidemiologist at World
Health Organization
Correspondence:
Lana sati Goussous, Msc Pharm,
Royal Medical Services
Jordan
Email: halasah@yahoo.com
|
Abstract
Hypertension
is considered as one of the most frequent
chronic illnesses and the most important
cardiovascular risk factor in developed
countries. Despite the fact that many
advances in the management of hypertension
have been made, still noncompliance with
prescribed therapeutic drugs is considered
a major barrier in clinical control and
management of hypertension drug therapy.
This study aimed to determine the most
prevalent factors related to non-compliance
to antihypertensive treatment.
Design: A questionnaire-based cross-sectional
study focused on factors thought to be
responsible for non-compliance with hypertensive
medication, in patients referred to out-patient
medical clinic at Prince Zaid Military
Hospital, Jordan.
Participants: 471 patients attended
the out-patient medical clinic during
the period from June, 2011 - December,
2011.
Results: The study revealed that
about 24% of the enrolled patients were
non-compliant to the hypertensive treatment
in which (80.7%) reported that lack of
information regarding importance of taking
drugs, drug prescription regimen for more
than one dose per day accounted for (71.9%)
while primary and secondary education
levels (70.2%) were more than the illiterate
and higher education. The number of medications
among non-compliant patients accounted
for (62.2) for more than one medication
and unavailability of drug (59.6%), forgetfulness
(55.3%) and drug side effects (50.9%)
and absence of symptoms (44.7 %) was the
least reported factor of non-compliance.
Key words: Hypertension, Compliance,
non-compliance.
|
Hypertension is one of the most common disorders
in the world. For some patients with hypertension,
blood pressure can't be adequately controlled
despite treatment with antihypertensive drugs
(1). Such patients have treatment resistant
hypertension, which is according to one definition:
persistent high blood pressure > 140/90 mmHg
for patients aged less than or equal to 60 years,
or 160/90 mmHg for those aged more than 60 years
(2). Various explanations have been given for
treatment resistant hypertension; these include
secondary hypertension, endogenous resistance
to treatment, and noncompliance to treatment
(2), for which the last reason is the most prevalent
( 3). Patients' poor compliance with treatment
is often suggested as the reason for lack of
response to antihypertensive drugs and causes
reduction of benefit provided by these drugs.
Consequently, prescription of additional unnecessary
drugs that might cause health care costs to
be increased through unnecessary investigations,
and dose adaptation for patients who aren't
taking their drug adequately or potential increase
of the number of hospitalizations (4).
Identifying factors associated with noncompliance
will help set the strategies to enhance compliance.
Definition of Terms
For the purpose of this study, terms were theoretically
and operationally defined:
Hypertension was theoretically defined as the
persistent high arterial blood pressure reading
of 140/90 mmhg for those aged below 60 years
and 150/100 mmhg for those aged above 60 years
(2), and hypertension was operationally defined
as the presentation of high blood pressure >
140/90 mmhg for Patients aged < 60years or
> 160/90 mmhg for those aged > 60 years)
as measured by the sphygmomanometer with the
patient lying down 5 minutes at least after
being in the clinic.
Compliance: The general term was defined
by the World Health Organization in their 2001
meeting as, "the extent to which a patient
follows medical instructions". With respect
to the drug therapy, compliance is defined as
the degree of correspondence of the actual dosing
history with the prescribed drug regimen (5).
Compliance rate was estimated as
No. of pills missed ..........................................
*100%
No. of prescribed pills in the same period
Non-compliance: was defined as the deviation
of the dosing history from the drug regimen
(5), and those who reported irregularity in
taking their antihypertensive treatment and
compliance rate below 80% was considered to
be noncompliance.
Purpose of the study:
The purpose of this study was to identify factors
responsible for non-Compliance with the treatment
of patients with Hypertension.
A Cross- Sectional Study
Design was used for the
purpose of this study;
471 hypertensive patients
attended the out-patient
clinic at Prince Hashim
Hospital during the period
from June, 2011 - December,
2011. All patients diagnosed
with hypertension and
willing to be enrolled
in this study after obtaining
informed consent from
each patient, were interviewed
using a structured questionnaire
form. The first part of
data collection form included
information about gender,
age, educational level
and information regarding
aspects of hypertension
treatment, such as disease
duration, number of drugs
taken for hypertension
(1, 2 or > 2 drugs),
drug regimen (once, twice
or more than twice per
day). The second part
of the questionnaire consisted
of a list of factors thought
to be responsible for
non-compliance and the
patient was expected to
select their own reason
for being non-compliant.
These factors included:
lacking information regarding
importance of taking drugs,
absence of symptoms, non-availability
of drug, drug side effects
and forgetfulness.
Non-compliance hypertensive
patients were defined
as those with raised blood
pressure of more than
or equal to 140/90 mmHg
on two prior clinical
visits. Patients who had
a systolic blood pressure
of less than 140 mmHg
and/or Diastolic blood
pressure of less than
90 mmHg were considered
to have a controlled blood
pressure and compliant
to the treatment.
The
study
revealed
that
about
24%
of
the
enrolled
patients
were
non-compliant
to
the
antihypertensive
treatment
and
among
those
(80.7%)
reported
that
they
don't
have
enough
information
about
their
disease
and
lack
of
information
regarding
importance
of
taking
drugs
given
to
them
by
health
care
team
(nurse
or
doctor).
Drug
prescription
regimen
was
viewed
as
the
2nd
reason
behind
non-compliance
which
attributed
to
drug
prescription
regimen
as
a
strong
factor
harboring
their
compliance
with
their
treatment
(71.9%)
while
non-compliance
among
primary
and
secondary
education
levels
(70.2%)
were
more
than
the
illiterate
and
higher
education.
The
number
of
medications
among
non-compliance
accounted
for
(62.2)
for
more
than
one
medication
and
unavailability
of
drug
(59.6%),
forgetfulness
(55.3%)
and
drug
side
effects
were
(50.9%)
and
absence
of
symptoms
(44.7
%)
was
the
least
reported
factor
of
non-compliance.
The
mean
age
of
participants
was
59
years
(SD
11.18)
and
the
age
group
of
more
than
60
years
comprised
56.7%
of
the
cases.
There
was
no
gender
difference
among
non-compliant
patients
to
antihypertensive
medication.
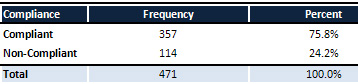
Table
1:
Distribution
of
hypertensive
patients
by
their
compliance
to
Treatment
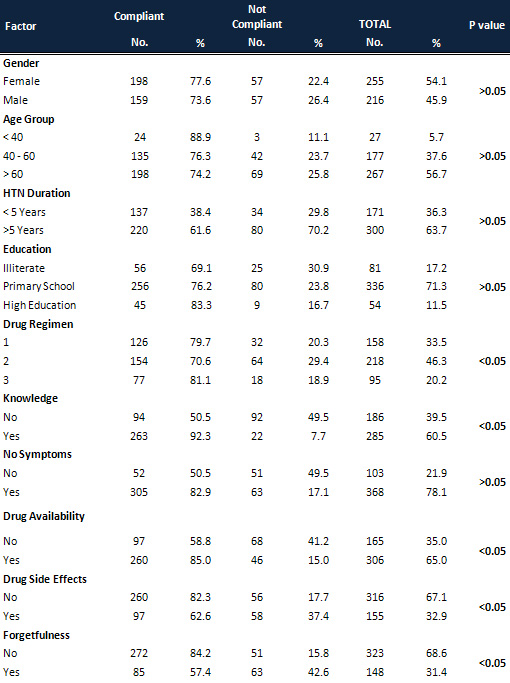
Table
2:
Compliance
rate
in
relation
to
Socio-demographic
factors
Patients
involved
in
this
study
were
middle
aged
to
elderly
hypertensive
men
and
women
who
had
the
disease
for
several
years.
The
study
was
based
on
the
self-reporting
estimation,
which
was
the
only
available
and
accessible
method
that
could
be
used
since
the
electronic
method
is
not
available
and
pill
counting
method
is
thought
to
be
overestimating
compliance.
Finding
of
this
study
revealed
a
variety
of
results
and
associated
factors
which
influence
the
compliance
behavior
among
patients
with
hypertension.
The
major
cause
of
noncompliance
was
lack
of
information
and
knowledge
on
need
for
regular
antihypertensive
treatment
which
was
consistent
with
findings
of
a
similar
study
in
Nigeria
(6)
and
in
a
qualitative
study
conducted
on
seven
focus
groups
attending
two
primary
health
care
centers
of
the
Spanish
national
health
services,
in
an
attempt
to
identify
factors
of
noncompliance,
factors
were
identified
that
influence
noncompliance.
Lack
of
basic
background
knowledge
about
hypertension
and
patient
fear
and
negative
images
of
antihypertensive
drugs,
lack
of
basic
knowledge
background,
was
explained
by
the
previous
study
and
the
explanation
that
was
also
thought
to
explain
the
findings,
is
that
clinical
encounter
was
viewed
as
unsatisfactory
because
of
its
length
and
low
patient-physician
interaction
time
that
resulted
from
overwhelming
number
of
patients
attending
the
clinic
(7).
No
relation
between
age
and
compliance
rate
was
found
(P-value
not
significant,
0.23)
which
is
inconsistent
with
a
study
done
in
Saudi
Arabia
which
showed
a
higher
compliance
rate
among
those
>
55
years
of
age
(48.5%)
(9).
Another
study
in
Ghana
showed
a
higher
compliance
rate
in
age
group
40-60
years
(68%)
and
a
decreased
rate
in
those
less
than
40)
years
and
above
60
years
(6%,
33%
respectively)
(10),
and
is
compatible
with
a
study
done
in
Shiraz,
Iran.
(11)
There
is
a
decrease
in
compliance
rate
in
those
patients
with
primary
and
secondary
school
education
(70.2%)
while
no
significant
difference
among
those
with
higher
education
and
non-educated
patients
which
is
inconsistent
with
two
studies
done
in
Ghana
(9)
and
Saudi
Arabia
(8)
showing
that
compliance
rates
in
educated
patients
were
18%
and
33
%respectively
and
consistent
with
two
studies
in
Finland
(11)
and
Nigeria
(6)
showing
high
compliance
rate
in
educated
patients
(81.5%,74.2%
respectively).
These
differences
could
be
due
to
the
characters
of
patients
attending
these
health
care
centers
while
most
of
our
patients
were
primary
and
secondary
education
and
the
least
were
highly
educated.
It
is
well
known
that
compliance
is
improved
if
the
patient
is
taking
a
single
drug
rather
than
two
or
more
(11).
This
study
showed
that
those
on
single
medication
were
more
compliant
(79.7%)
than
those
on
more
than
one
drug
which
is
compatible
with
a
study
in
Sudan
(12)
and
Saudi
Arabia
(8),
which
showed
compliance
rate
with
one
drug
of
(80.8%
and
78.9%
respectively).
A
higher
rate
of
non-compliance
was
seen
in
those
patients
who
had
been
hypertensive
for
more
than
5
years
and
decreased
rate
with
less
than
5
years
which
is
contradicting
the
findings
of
Mallon
JM
(13),
who
showed
that
54-83%
of
patients
were
more
compliant
after
5
years
from
start
of
their
medications.
The
fact
that
patients
think
that
they
have
been
cured
so
they
were
not
regularly
taking
their
medication
due
to
the
absence
of
symptoms
only
(17.1%)
were
non-compliant
to
antihypertensive
treatment
compared
with
a
study
in
the
United
States
(14)
which
showed
that
(46%)
were
non-compliant
while
the
same
study
found
that
non
-
compliance
due
to
side
effects
was
(11%)
compared
to
what
was
found
in
this
study
(37.4).
| CONCLUSION
AND
RECOMMENDATIONS
|
Blood
Pressure
control
remains
an
essential
therapeutic
approach
to
prevent
the
occurrence
of
coronary
heart
disease,
heart
failure,
stroke
and
premature
death.
Compliance
with
treatment
is
a
fundamental
prerequisite
for
therapeutic
benefit.
Strategies
to
overcome
the
barriers
perceived
by
the
patient
and
hinder
their
compliance
should
be
set
as
a
priority.
To
provide
sufficient
information
about
hypertension,
risks
and
treatment,
must
be
considered.
To
plan
to
prescribe
a
drug
regimen
that
is
effective,
long
acting
drugs
that
provide
blood
pressure
control
beyond
the
24
hour
dosing
period
might
help
to
prevent
the
consequences
of
occasional
drug
omission.
In
addition,
increased
physician
-patient
interaction
and
awareness
of
health
status
are
essential.
1.
The
sixth
report
of
the
joint
national
committee
on
Detection,
Evaluation,
and
Treatment
of
High
Blood
Pressure.
(1997).
Archives
of
International
Medicine,
157,
2413-2445.
2.
John
F.
Setaro,
HENRY
R.
Black.
(1992).
Refractory
hypertension.
The
New
English
Journal
of
Medicine;
327,
8:
534-
547.
3.
Davidson's
Principles
and
Practice
of
medicine
(P.
222).
Philadelphia:
Churchill
Livingstone.
4.
Mark
V.Pauly.
The
American
Journal
of
medicine
(1986)
,81(suppl
60):3-8
5.
Urquhart,
J.
(1994).
Role
of
patient
compliance
in
clinical
pharmacokinetics
:
review
of
recent
research
.clinical
pharmacokinetics
,
1994
,
Abstract
.
6.
M.kabir,
Z.lliyasu,
I.S.Abubakar,
M.Jibirl.
Compliance
to
medication
among
hypertensive
patient
in
Murtala
Mohammed
specialist
Hospital,
Kano,Nigeria.
2004,16:16-20.
7.
Juan
J.
Gascon,
Montserrat
Sanchez
-ortuns,
Bartolome
Lior,
David
Skidmore,
Pedrj
Saturns
for
the
treatment
compliance
in
hypertension
study
group.
Why
hypertensive
patients
don't
comply
with
the
treatment
:
result
from
a
qualitative
study.
Abstract.
8.
Al-
sowielem
S,
Al-zubier
A.
Compliance
and
knowledge
of
hypertensive
patients
attending
PHC
centers
in
Alkhobar.
Saudi
Arabia,
Eastern
Mediterranean
Health
Journal.1998;4:301-7.
9.
Kwane
O,
Lioyd
M.
Unaffordable
drug
prices:
the
major
cause
of
non-compliance
with
hypertensive
medication
in
Ghana.
Journal
of
pharmacy,
2004;7:350-52.
10.
Nadi
N,
Gooran
N.
Effectiveness
of
hypertension
educational
program
on
increasing
medical
compliance
in
Shiraz.
Shiraz
Medical
Journal,
2006;7:11-12
11.
Erkki
J.
Compliance
and
patients-perceived
problems
in
the
treatment
of
hypertension.
PhD
dissertation,
2005.
12.
Alzubier
A,
Hussein
M.
Drug
compliance
among
hypertensive
patients
in
kassala
(Sudan).
EMHJ,2000;6:100-105.
13.
Mallion
J,
Schmitt
D.
Patient
compliance
in
the
treatment
of
arterial
hypertension.
European
Society
of
hypertension
scientific
newsletter,
2001;2.
14.
Gallup
G,
Cotugno
H.
Preferences
and
practices
of
american
and
their
physicians
in
hypertensive
therapy.
AMJ,
1986;81:20-24.
|
|
.................................................................................................................

|
| |
|

