|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................
|
Original
Contribution/Clinical Investigation
|
|

|
<-- Turkey -->
Very high
levels of C-reactive protein should alert the
clinician to the development of acute chest
syndrome in sickle cell patients
[pdf version]
Can Acipayam, Sadik Kaya, Mehmet Rami Helvaci,
Gül Ilhan, Gönül Oktay
<-- Jordan -->
Seroprevalence
of HBV, HCV, HIV and syphilis infections among
blood donors at Blood Bank of King Hussein Medical
Center: A 3 Year Study
[pdf
version]
Baheieh Al Abaddi, Maha Al Amr, Lamees Abasi,
Abeer Saleem, Nisreen Abu hazeem, Ahmd Marafi
|
|
........................................................ |
Medicine and Society
........................................................
International Health
Affairs
.......................................................
Education
and Training
.......................................................
Continuing
Medical Education
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| August 2014 -
Volume 12 Issue 6 |
|
Training
medical students in general practices: Patients'
attitudes
R. P. J .C. Ramanayake (1)
A. H. W. de Silva (2)
D. P. Perera (2)
R. D. N. Sumanasekera (2)
K. A. T. Fernando (3)
L. A. C. L. Athukorala (3)
(1) Senior Lecturer, Department of Family
Medicine, Faculty of Medicine, University of
Kelaniya, Sri Lanka.
(2) Lecturer, Department
of Family Medicine, Faculty of Medicine, University
of Kelaniya, Sri Lanka.
(3) Demonstrator,
Department of Family Medicine, Faculty of Medicine,
University of Kelaniya, Sri Lanka.
Correspondence:
Dr. R. P. J. C. Ramanayake
Senior
Lecturer, Department of Family Medicine, Faculty
of Medicine,
University of Kelaniya, Sri Lanka.
Mobile: 0094773308700
Email:
rpjcr@yahoo.com
|
Abstract
Introduction:
Training medical students in the setting
of family/general practice has increased
considerably in the past few decades in
Sri Lanka with the introduction of family
medicine into the undergraduate curriculum.
This study was conducted to explore patients'
attitudes towards training students in
fee levying general practices.
Methodology: Six general practices,
to represent different practices (urban,
semi urban, male and female trainers)
where students undergo training, were
selected for the study. Randomly 50 adult
patients were selected from each practice
and they responded to a self administered
questionnaire following a consultation
where medical students had been present.
Results: 300 patients (57.2 % females)
participated in the study. 44.1% had previously
experienced students. 30.3% were able
to understand English. Patients agreed
to involvement of students; taking histories
(95.3%), examination (88.5%), looking
at reports (96.6) and presence during
consultation (88.3 %). Patients' perceived
no change in duration (55%) or quality
(56.3%) of the consultation due to the
presence of students. The majority (78%)
preferred if doctor student interaction
took place in their native language. 45.8%
expected prior notice regarding student
participation and two to three students
were the preferred number. 93.6% considered
their participation as a social service
and only 8.8% expected a payment.
Conclusion: The vast majority of
the patients accepted the presence of
students and were willing to participate
in this education process without any
reservation. Their wishes should be respected.
The outcome of this study is an encouragement
to educationists and GP teachers.
Key words: Medical students, training,
General practice, patients' attitudes
|
There is a growing trend that undergraduate teaching
should take place more within the community, primarily
in the general practices(1,2) and as a result
worldwide Family medicine has come into the core
of the medical curriculum during the last few
decades.(3,4) That trend has invaded the Sri Lankan
medical schools as well and it is now well established
in most of the medical schools in the country.(5)
The reasons for this trend are many; everywhere
in the world in-patient care as a proportion of
all medical care is decreasing.(4,6) Diseases
which required in-patient care earlier no longer
do so due to the invention of newer medications
and newer techniques and accessibility of general
practitioners to investigations, telemedicine
and the internet.(4) The duration of stay in hospitals
for diseases which require admission has also
reduced considerably due to more efficient newer
medications and techniques. Educationally, there
are implications on undergraduate training due
to this trend. The morbidity seen in a hospital
ward has become less and less representative of
the overall morbidity in the whole population
and the opportunity for hands on experience for
students has reduced.(4) In the mean time community
offers a wealth of teaching opportunities for
medical students, a fact which was recognized
by the General medical council's directive, Tomorrow's
doctors(GMC,1993)(2).
General practitioner teachers have also transformed
from their original role as teachers of behavioral
science and general practice(7) into teachers
of clinical skills, with excellent access to a
wide range of patients.(8,9) It has been found
that community based teaching is as effective
as hospital based teaching of basic clinical skills.(10,11)
General practices offer a highly personalized
teaching in an environment where the importance
of social, economic, psychological and cultural
influences on a patient's illness and the family
response can be experienced firsthand. (12) It
is also an opportunity for students to get an
insight into the socio-economic environment of
patients and the local resources available to
them.
Participating in a general practice clerkship
has been shown to stimulate students to choose
general practice for their career(13) and students
who will take on another specialty will have gained
an understanding of primary care. (14)
Training undergraduates in family practices converts
an activity between two parties (doctor and patient)
into a three party affair.(15) It's in the privacy
of the consultation room that patients divulge
and discuss some sensitive issues and the presence
of students could affect the doctor patient relationship
and interaction. In a family practice patients
are autonomous and the majority of the patients
are ambulatory. They spend only a limited time
in a family practice and student participation
could lead to delays. Patients' consent to participate
in medical education is often taken for granted
and patients are not always aware of teaching
activities.(16)
The Faculty of Medicine, University of Kelaniya
sends students to general practices during their
fourth year. They learn by observing doctor
patient encounters, taking histories, performing
clinical examinations and getting involved with
the management of patients with the GP teacher.
The doctor student interaction usually takes
place in English which is the medium of medical
education in the country.
Although studies from the western world have
revealed the positive attitude of patients towards
presence and involvement of students during
the consultation, this area remains relatively
unresearched in Sri Lanka and the south Asian
region. The only reported study from Sri Lanka
in this regard also supported the acceptance
of students by the patients but this study has
been conducted in a non fee levying university
family practice.(17)
Therefore this multicentre study was planned
to explore attitudes of patients towards students
in fee levying general practices.
This descriptive cross sectional study was conducted
in 6 general practices purposively selected to
represent urban and semi-urban practices as well
as general practices managed by both male and
female doctors. A self administered questionnaire
was used to gather demographic data, number of
previous consultations with student participation
and their willingness to have presence of students
at different stages of the consultation, reasons
for the willingness, the factors impacting upon
willingness, patients' experience of consultations
in the presence of students and their views on
consent and confidentiality. Fifty consecutive
eligible patients who consulted the doctor in
the presence of students were invited to respond
to the questionnaire. Patients below 16 years,
seriously ill patients, and confused or cognitively
impaired patients, who were unable to read and
write, were excluded. Younger patients were excluded
since they may not be able to respond to the questionnaire
and the opinion of the guardian could vary depending
on the relationship to the patient.
Ethical approval for the study was obtained from
the ethical review committee of the faculty of
medicine, University of Kelaniya.
A total of 300 patients responded to the questionnaire.
Table 1: Demographic details of the patients
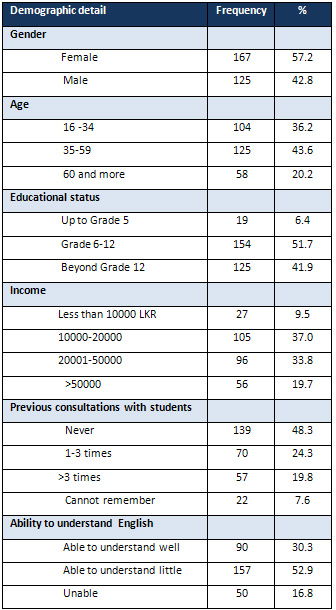
n=300 note: Percentages expressed are of valid
responses for a given item, not for the entire
sample
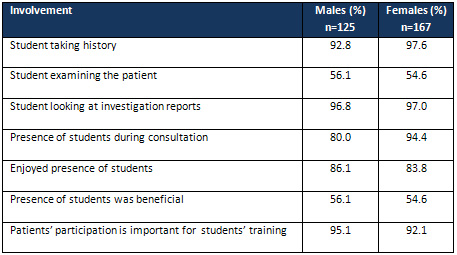
Table 2: Patients' agreement on involvement
of students
Patients' opinion on discussing their problems
in English
Overall 81.7% agreed with the doctor discussing
their problem in English with students, while
77% felt it was better if the discussion took
place in their native language. More people
among those who could not understand English
preferred if discussions took place in their
native language.
Table 3: Patients' attitudes towards discussion
in English vs their knowledge of English
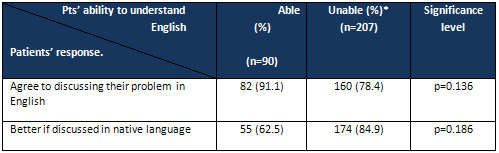
*able to understand little + unable to understand
Graph 1: Patients' perception on the impact
of presence of students on quality & duration
of consultation
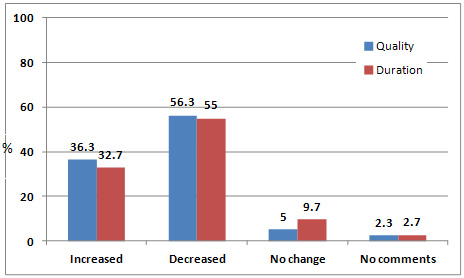
Only 14.3% of the patients were unhappy about
having to spend more time during consultation
due to the involvement of students. 75.5% were
not bothered while 10.2% did not respond to
the question.
Graph 2: Patients' opinion on involvement
of training and expectation of a payment
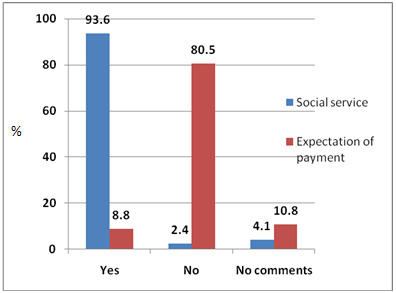
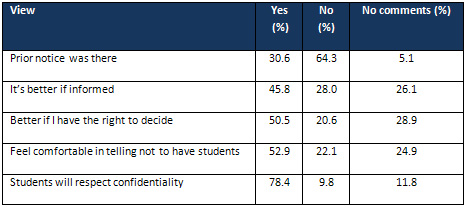
Table 4: Patients' views on consent and
confidentiality
Patients' views on number of student participation
during consultation
17.1% of the patients preferred the presence
of one student while 29.0% preferred 2 students.
Another 23.9% preferred 3 and 30% agree with
the presence of more than 3 students.
For this multicenter study general practices were
purposively selected to include general practices
with different backgrounds with the objective
of obtaining views of a wide range of patients.
Analysis of their demographic details shows that
the sample included both males and females, patients
belonged to all age groups, and different socioeconomic
and educational backgrounds. It also included
patients who had previous experience with students
and those who had not consulted the doctor in
the presence of students.
The vast majority of patients had positive feelings
about the involvement of medical students. More
than 90% of the patients were willing to tell
details of the disease to students but only about
50% agreed to be examined by a student. There
was no significant difference in attitudes between
males and females. There was no resistance to
students looking at their investigation reports
and the majority not only agreed to presence of
students during consultation, they enjoyed interaction
with students as well. Quite rightly patients
have understood that their participation is important
for student training. Number of previous studies
also reported high consent rate to presence or
participation of students in general practices.(18,19,20)
Our finding that patients were less willing to
be examined by a student was also in line with
reported studies. (16,21,)
This study explored views of patients on doctor
student interaction taking place in English
which is not the native language of the country.
Only 30.3% of the participants could understand
English language well according to them. Even
though they agreed to doctor student interaction
in English they preferred if discussions took
place in their native language. Studies conducted
in western countries where the medium of learning
and the mother tongue of patients were the same
revealed that patients enjoyed hearing their
condition being discussed with the students
(22), drew more information from the explanation
directed at students and discussions with students
led to increased insight into clinical reasoning.(23)
Such benefits cannot be expected for patients
in Sri Lankan settings and even could have unwarranted
effects such as misunderstandings in patients
which could create unnecessary anxiety. Therefore
GP teachers should either discuss with students
in native language or offer an explanation to
patients afterwards. It is important not to
sideline patients in discussions and a sense
of inclusion and participation is essential
for patient satisfaction with the experience.
(24)
The perception among patients that the quality
of the consultation was not adversely affected
due to the presence of students by the majority
(92.6%) is an encouragement to GP trainers.
In fact about one third felt there was a positive
impact perhaps due to more detailed history
taking, methodical examination and plan of management
and doctor spending more time with the patient
due to the presence of students. The findings
regarding quality of consultation of this study
are in line with previous studies which reported
no decreased sense of patient enablement or
satisfaction(25,26) and even a positive effect.(26,27,28)
32.7 percent thought the duration of the consultation
was more when students were present but the
majority (74%) was not unhappy and willing to
sacrifice their time.
It is heartening to note that the majority of
the respondents were of the view that their
involvement in undergraduate training is a social
service and did not expect a payment for their
involvement and contribution. The probable reasons
may be sense of altruism, mutual obligation
and giving something back to the system.(24,29)
Patients' opinion on the number of students
they would like to interact with at a time varied.
When deciding on the number of students the
space in the consultation room also should be
taken into account. If the room is overcrowded
patients may not feel free to divulge information
and feel embarrassed during examination. It
can create problems for the doctor in managing
patients and for students such an environment
may not be conducive for learning. More students
could compromise one of the key advantages of
community based learning which is the one to
one supervision and the attention of the trainer.
According to patients only 30.6% were aware
that students would be present during the consultation
which is not a satisfactory situation. A fairly
high percentage thought it would have been better
if they were informed beforehand. It is interesting
to note that half the patients felt that they
should be given the choice to decide. Studies
elsewhere in the world have revealed that patients'
consent to participation in medical education
is often taken for granted and formal consent
is not obtained prior to their involvement in
teaching.(16) It is only 52.9% who felt comfortable
in telling the doctor not to have students.
Patients may feel pressured to consent to the
students' presence and they may be concerned
that refusal to have students may disappoint
their family doctor. There is evidence that
patients may have difficulty refusing consent(26)
and GPs should be mindful of this fact.
Patients were of the view that students will
respect the confidentiality of the information
they receive from patients. In one study patients
expressed concern that students would talk about
them afterwards.(30) Students should be strictly
instructed not to discuss about patients in
a careless manner.
Issue of consent and confidentiality should
be an integral part of teaching in both primary
and secondary care and patients should be explained
the need of their participation in teaching
and advantages and disadvantages of participation
of students. Patients should be made aware that
they have the freedom to choose and their non
involvement will in no way influence the care
they receive or the doctor patient relationship.
Patient information can be made available in
the waiting room and consulting rooms to reiterate
that patients have a choice about presence of
students.
This study which demonstrates the views of
a broad range of patients reveals the positive
attitudes of patients and their willingness
to participate in student training which is
vital for the sustainability of community-based
teaching.(31) The findings of this study will
be reassuring for doctors who presently are
involved and those who plan to be involved in
undergraduate training in the future. It will
be of help in planning general practice clerkships.
1. Patients are a willing resource for
student education in training practices.
2. Patients perceive that presence of students
does not decrease the quality of consultation.
3. Patients should be able to choose when
they want to be involved in teaching.
4. Trainers should be careful when discussing
with students in a language not understood by
the patient and at least a brief explanation should
be provided to the patient on what was discussed
1. Boaden N, Bligh J.
Community based medical
education. London: Arnold.
1999;29-41
2. General Medical Council.
Tomorrow's Doctors: Recommendations
on Undergraduate Medical
Education. London: GMC,1993.
3. Marley J. Family medicine
in the 21st century. Sri
Lankan Family Physician
1998;21:22-23
4. Metcalfe D. Family
Medicine: in from the
periphery in medical education.
Sri Lankan Family Physician
1999: 22(1); 3-7.
5. Ramanayake RPJC. Historical
evolution and present
status of family medicine
in Sri Lanka. Journal
of family medicine and
primary care 2013:2;131-134
6. Institute for the Future.
Health and health care,
2010, the forecast, the
future, the challenge.
San Francisco: Jossey-Bass,
2000;6-8.
7. Towle A. Community
based teaching. Sharing
ideas 1. London: King's
Fund Centre; 1992.
8. Parle JV, Greenfield
SM, Skelton J, Lester
H, Hobbs FD. Acquisition
of basic clinical skills
in the general practice
setting. Med Educ 1997;31:99-104.
9. Oswald NT. Teaching
clinical methods to medical
students. Med Educ 1993;27:351-
4.
10. Murray E, Jolly B,
Model M. Can students
learn clinical method
in general practice? A
randomized crossover trial
based on objective structured
clinical examinations.
Br Med J 1997;315:920-3.
11. Berg D. Sebastian
J, Heudebert G. Development,
Implementation and evaluation
of an advanced physical
diagnosis course for senior
medical students. Acad
Med 1994;69:758-64.
12. Lefford F, Mccroriet
P, Perrins F. A survey
of medical undergraduate
community-based
teaching: taking undergraduate
teaching into the community.
Medical Education 1994;28:
312-315
13. Senf JH, Campos-Outcalt
D, Kutob R. 2003. Factors
related to the choice
of family medicine: A
reassessment and literature
review. J Am Board Fam
Pract 2003; 16(6):502-12.
14. Mol SSL, Peelen JH,
Kuyvenhoven MM. Patients'
views on student participation
in general practice consultations:
A comprehensive review.
Medical teacher 2011;33:e397-e400
15. Wright HJ. Patients'
Attitudes to Medical Students
in General Practice. BMJ
1974;1: 372-6.
16. Monnickendam SM, Vinker
S, Zalewski S , Cohen
O, Kitai E. Patients'
Attitudes Towards the
Presence of Medical Students
In Family Practice Consultations.
IMAJ 2001; 3:903-906 .
17. Ramanayake RPJC, Sumathipala
WLAH, Rajakaruna IMSM,
Ariyapala DPN. Patients'
Attitudes Towards Medical
Students in a Teaching
Family Practice: A Sri
Lankan Experience. Journal
of Family Medicine and
Primary Care 2012 ; 1
(2): 122-126
18. Choudhury TR, Moosa
AA ,Cushing A, Bestwick
J. Patients' attitudes
towards the presence of
medical students during
consultations. Med Teach
2006 ;28(7): e198-203
19. Haffling AC, Hakansson
A. 2008. Patients consulting
with students in general
practice: Survey of patients'
satisfaction and their
role in teaching. Med
Teach 30: 622-629.
20.Hudson JN, Weston KM,
Farmer EE, Ivers RG, Pearson
RW. 2010. Are patients
willing participants in
the new wave of community-based
medical education in regional
and rural Australia? Med
J Aust 192(3):150-153.
21. Salisbury K, Farmer
EA, Vnuk A. Patients'
views on the training
of medical students in
Australian general practice
settings. Australian Family
Physician 2004;33(4):281-283
22. Grant A, Robling M.
Introducing undergraduate
medical teaching into
general practice: an action
research study. Medical
teacher 2006; 28: 7:e192-e197
(doi:10.1080/01421590600825383)
23. Sturman N. Teaching
medical students Ethical
challenges. Aust Fam physician
2011;40(12):992-995
24. Sweeney K, Magin P,
Pond D. Patient attitudes:
training students in general
practice. Aust Fam Physician
2010;39:676-82
25. Benson J, Quince T,
Hibble A, Fanshawe T,
Emery J. Impact on patients
of expanded, general practice
based, student teaching:
observational and qualitative
study. BM J 2005;331:89.
doi: 10.1136/bmj.38492.599606.8F
26. Price R, Spencer J,
Walker J. Does the presence
of medical students affect
quality in general practice
consultations? Med Educ
2008;42:374-81.
27. Cooke F, Galasko G,
Ramrakha V, Richards D,
Rose A, Watkins J. Medical
students in general practice:
how do patients feel?
BM J 1996;46:361-2.
28. Holden J, Pullon S.
Trainee interns in general
practices. N Z Med J 1997;110:377-9.
29. Coleman K, Murray
E. Patients' views and
feelings on the community-based
teaching of undergraduate
medical students: a qualitative
study. Family Practice
2002;19: 2:183
30. O'Flynn N, Spencer
J, Jones R. Consent and
confidentiality in teaching
in general practice: survey
of patients' views on
presence of students.
BMJ 1997; 315: 1142.
31. Rod Pearce, Caroline
O Laurence, Linda E Black,
Nigel Stocks. The challenges
of teaching in a general
practice setting. MJA
2007:187;129-132
|
|
.................................................................................................................

|
| |
|

