|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................
|
Original
Contribution/Clinical Investigation
|
|

|
<-- Turkey -->
Very high
levels of C-reactive protein should alert the
clinician to the development of acute chest
syndrome in sickle cell patients
[pdf version]
Can Acipayam, Sadik Kaya, Mehmet Rami Helvaci,
Gül Ilhan, Gönül Oktay
<-- Jordan -->
Seroprevalence
of HBV, HCV, HIV and syphilis infections among
blood donors at Blood Bank of King Hussein Medical
Center: A 3 Year Study
[pdf
version]
Baheieh Al Abaddi, Maha Al Amr, Lamees Abasi,
Abeer Saleem, Nisreen Abu hazeem, Ahmd Marafi
|
|
........................................................ |
Medicine and Society
........................................................
International Health
Affairs
.......................................................
Education
and Training
.......................................................
Continuing
Medical Education
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| August 2014 -
Volume 12 Issue 6 |
|
The
presence of H.pylori in cases of chronic idiopathic
urticaria
Rashad Feddah
Ibraheem Banihameem
Anwar Farhan
Saeed Al-Ahmari
Fayeh Asiri
Hamad AL Fahaad
Wadha Alfarwan
Correspondence:
Dr. Anwar Farhan, MD
Consultant dermatologist
King Khalid Hospital, Najran, Saudi Arabia
Tel: (Cell phone) +966 553044333
Email:
anwarfarhan@yahoo.com
|
Abstract
Introduction:
Urticaria (or hives) are a kind of skin
rash notable for dark red, raised, itchy
bumps.Chronic urticaria, defined as urticaria
that persists for longer than 6 weeks,
it is not a single disease but a reaction
pattern that represents cutaneous mast
cell degranulation, resulting in extravasation
of plasma into the dermis and the patients
may not improve or may depend on medication
for years to relieve symptoms. chronic
urticaria is one of the most common problems
facing dermatologists and other specialities.
It is the problem which bothers both the
patient and the dermatologist. Traditionally,
the approach in patients with chronic
urticaria (when physical etiology has
been excluded) has been to order a panel
of laboratory tests to discover an occult
medical condition responsible for the
skin findings. In many patients, an extensive
workup does not discover an etiology.
Patients in whom no explanation for his
urticaria are said to have chronic idiopathic
urticaria. Various infectious agents have
been reported as causes of urticaria,
including Helicobacter pylori (H. pylori),
which is a common worldwide bacterial
infection. Its role in inducing allergic
conditions, such as chronic urticaria,
has been suggested in some reports and
ignored in others.
Aim : In our research, we want
to look for the prevalence of Helicobacter
pylori in the serum of patient who presented
with chronic urticaria .The patient has
endure treatment and is not cured besides
partial treatment causes temporary relive
of symptoms. So, it is important to make
the right decisions regarding the treatment
of chronic urticaria by adding triple
therapy for those who are H.pylori
positive.
Subjects and Methods: This study
is a non controlled , consecutive interventional
study involving 60 patients during the
period from November 2012 to April 2013
with history of urticarial lesions of
> 6 weeks, to search for the possible
cause of their chronic urticaria.
Results: Among 60 patients suffering
from chronic Urticaria only 40 (66.7%)
patients were enrolled in the study with
chronic idiopathic urticaria.
25 patients (62.5%) of chronic idiopathic
urticaria were infected with H.pylori
and 15 patients (37.5%) had negative serology
for H.pylori. 80% of patients with
positive H.pylori had G.I.T symptoms
,18 patients (72%) were achieved eradication
with the first line therapy while 5 patients
(20%) required the second line therapy
for eradication. In 2 patients (8%) H.pylori
persisted despite two courses of
eradication therapy. Response to eradication
therapy was evident in 19 patients (76%)
in whom H.pylori was eradicated
while 4 patients (16%) showed no response
despite eradication of H.pylori.
Two patients (8%) with persistent H.pylori
infection showed no improvement in
the urticarial symptoms at the end of
study period.
Conclusion: The results of our
study strongly suggest that H.pylori should
be specifically tested in all patients
of CIU, to identify subset of patients
who are infected and who could benefit
from eradication therapy. H.pylori
should be included in the diagnostic work
up of all patients with CIU.
Key words : H.pylori, chronic
idiopathic urticaria , chronic urticaria
|
The aim of this study is to identify cases who
presented with chronic urticaria at the health
center; to detect the appearance of H. pylori
in the serum of patients with chronic idiopathic
urticaria.
|
JUSTIFICATIONS OF THE STUDY |
Chronic urticaria is one of the most common problems
which we face in our clinical practice. It is
the problem which bothers both the patient and
the dermatologist. Traditionally, the approach
in patients with chronic urticaria (when physical
etiology has been excluded) has been to order
a panel of laboratory tests to uncover an occult
medical condition responsible for the skin findings.
In many patients, an extensive workup does not
uncover an etiology. Urticaria rarely is the sole
manifestation of an underlying medical problem.
Patients in whom no explanation for the urticaria
is established are said to have chronic idiopathic
urticaria. Various infectious agents have been
reported as causes of urticaria, including Helicobacter
pylori, which is a common worldwide bacterial
infection. Its role in inducing allergic conditions,
such as chronic urticaria, has been suggested
in some reports and ignored in others.
In our research, we want to look for the prevalence
of Helicobacter pylori in the serum of patients
who presented with chronic urticaria. The patient
has endured treatment and is not cured besides
partial treatment causes temporary relief of symptoms,
so it is important to make the right decisions
regarding the treatment of chronic urticaria by
adding triple therapy for those who are H.pylori
positive.
Urticaria (from the Latin urtica, nettle (whence
It. ortica, Sp. ortiga, Pg. urtiga) urere, to
burn) (or hives) is a kind of skin rash notable
for dark red, raised, itchy bumps. [1]
Chronic urticaria, defined as urticaria that persists
for longer than 6 weeks, is not a single disease
but a reaction pattern that represents cutaneous
mast cell degranulation, resulting in extravasation
of plasma into the dermis and the patients may
not improve or may depend on medication for years
to relieve symptoms. [1]
The primary subgroups of chronic urticaria include
physical urticaria (symptomatic dermatographism,
cholinergic urticaria, pressure urticaria), urticaria
secondary to an underlying medical condition,
and chronic idiopathic urticaria. Physical urticaria,
which is reproducible with the appropriate stimuli,
can be identified with a thorough history and
challenge testing. [2]
Traditionally, the approach in patients with chronic
urticaria (when physical etiology has been excluded)
has been to order a panel of laboratory tests
to uncover an occult medical condition responsible
for the skin findings. In many patients, an extensive
workup does not uncover an etiology. Urticaria
rarely is the sole manifestation of an underlying
medical problem. Patients in whom no explanation
for the urticaria is established are said to have
chronic idiopathic urticaria; however, findings
suggest that in 25-45% of patients, chronic idiopathic
urticaria is not idiopathic but is an autoimmune
disease termed chronic autoimmune urticaria.[2]
After eliminating the physical urticarias and
urticarial vasculitis, chronic urticaria can be
divided into autoimmune chronic urticaria (45%)
and idiopathic chronic urticaria (55%).[3]
Approximately one third of patients with chronic
urticaria have either or both antithyroglobulin
antibody and antimicrosomal antibody, and up to
one fifth have abnormal thyroid function. A positive
functional anti-Fc R
test result supports an autoimmune basis and the
affected patients may be categorized as having
autoimmune chronic urticaria. Approximately one
third of patients with chronic urticaria may develop
angioedema after administration of aspirin or
othernonsteroidal anti inflammatory drugs.[4] R
test result supports an autoimmune basis and the
affected patients may be categorized as having
autoimmune chronic urticaria. Approximately one
third of patients with chronic urticaria may develop
angioedema after administration of aspirin or
othernonsteroidal anti inflammatory drugs.[4]
Approximately 85% of histamine receptors in the
skin are of the H1 subtype, with the remaining
15% being H2 receptors. The combination of H2
receptor antagonists with an H1 receptor antagonist
provides small additional benefit. Doxepin blocks
both types of histamine receptors and is a much
more potent inhibitor of H1 receptors than diphenhydramine
or hydroxyzine. [5]
A number of factors have been reported to cause
chronic urticaria, and these include medications
(aspirin, other non-steroidal anti-inflammatory
drugs, opioids, ACE inhibitors, and alcohol),
contact with an inciting agent, latex (especially
in health care workers), plants, animals (e.g.
caterpillars, dander), food (e.g. fish, garlic,
onions and tomato), arthropod assault (the most
common cause of papular urticaria) and infections
(HBV, HSV, Streptococcus, Mycoplasma, Helicobacter.pylori
and Mycobacterium tuberculosis). [6,7]
Urticaria has been associated with a number of
autoimmune diseases,.including systemic lupus
erythematosus, cryoglobulinemia, juvenile rheumatoid
arthritis and autoimmune thyroid disease, including
Graves disease.[8,9] Urticaria is a feature of
Muckle-Wells syndrome (amyloidosis, nerve deafness,
and urticaria) and Schnitzler syndrome (fever,
joint/bone pain, monoclonal gammopathy, and urticaria).[10]
Little evidence exists to support the concern
that chronic urticaria is a cutaneous sign of
occult internal malignancy. In a study of 1,155
patients with chronic urticaria in Sweden, Sigurgeirsson
found no association with cancer, although acquired
angioedema associated with C1 inhibitor depletion
may be associated with malignancy.[11]
Physical factors are the most commonly identified
etiologies of chronic urticaria, accounting for
approximately 20% of cases. [14]
Chronic urticaria may be a consequence of fibromyalgia-neurogenic
skin inflammation and psychological factors are
reported to play a role in a number of patients.
[12]
Avoidance of mental stress, overtiredness, alcohol,
non-steroidal anti-inflammatory drugs, and tight-fitting
garments is recommended. Nocturnal pruritus may
be reduced by lukewarm bathing and keeping the
ambient temperature of the bedroom cool. Application
of lotions with menthol and phenol (Sarna) provide
prompt relief of pruritus for some patients. [13]
Non-sedating antihistamines remain the mainstay
of treatment. Many patients find pruritus less
troublesome during the daytime, with pruritus
maximized at night when there are fewer distractions.
An additional nocturnal dose of a sedative antihistamine
such as hydroxyzine or doxepin may be added to
the morning dose of a low-sedation anti H1 antihistamine.
Doxepin should not be used in patients with glaucoma
and should be used with extreme caution in elderly
patients or those with heart disease. Doubling
the labeled dose of low-sedating antihistamines
may benefit some patients, and increasing the
dose of these antihistamines is often the safest
therapeutic approach for patients who do not have
an adequate response to the.conventional.dose.of.these.medications.
[14]
Patients who respond poorly to antihistamine therapy
or who are known to have urticaria in which the
inflammatory infiltrate is neutrophil predominant
may require the addition of colchicine (0.6 mg
twice daily) or dapsone (50-150 mg once daily)
to the treatment regimen (except patients with
glucose-6-phosphate dehydrogenase [G-6-PD] deficiency).
Patients with autoimmune urticaria may benefit
from methotrexate or cyclosporine.[13- 15]
A possible association between H. pylori infection
and chronic urticaria has been proposed [16-22],
and several mechanisms have been implicated. One
proposed mechanism is that an increase in gastric
vascular permeability during infection results
in greater exposure of the host to alimentary
allergens [23].In support of this suggestion duodenal
ulcer patients have a higher incidence of allergic
manifestations than controls. IgE-containing cells
in gastric and duodenal mucosa seem to be the
culprits [24], although there is limited evidence
for HP-specific IgE. Thus, the possibility that
patients with urticaria develop specific IgE against
H. pylori is an attractive pathogenic explanation
that unfortunately has not been confirmed yet.
[25,26]
The immunomodulatory role of H. pylori infection
in CU is a subject of intensive debate. This immunomodulation
is not only dependent on the virulence of H. pylori
but also on host and environmental factors. An
alternative possibility is that immunological
stimulation by chronic infection may produce,
through mediator release, a non-specific increase
in sensitivity of the cutaneous vasculature to
agents that enhance vascular permeability. Furthermore,
IgG and IgA antibodies to 19-kDa H. pylori-associated
lipoprotein were found to play a role in the pathogenesis
of CU. [27,28]
Moreover, H. pylori causes pronounced complement
consumption due to H. pylori specific antibodies.
This contributes further to the pathogenesis of
CU [29,30]. As recent studies have demonstrated,
IgG auto antibodies against IgE and/or Fc Ri a can be
found in the sera of one-third of patients with
CU, and it is postulated that infection with H.
pylori may induce production of pathogenetic antibodies
possibly by molecular mimicry [31]. A growing
body of evidence suggests that 30-50% of CU results
from an autoimmune process involving functional
histamine-releasing anti-Fc
Ri a can be
found in the sera of one-third of patients with
CU, and it is postulated that infection with H.
pylori may induce production of pathogenetic antibodies
possibly by molecular mimicry [31]. A growing
body of evidence suggests that 30-50% of CU results
from an autoimmune process involving functional
histamine-releasing anti-Fc  RI a auto antibodies
or less commonly, anti IgE auto antibodies [32,33].
Appelmelk et al first demonstrated the molecular
mimicry between H. pylori and lipopolysaccharide
(LPS) and anti-Lewis antibodies in autoimmune
type-B gastritis. [31] Further evidence was provided
by the highly positive autologous serum skin test
(ASST) results in chronic urticaria patients with
H. pylori IgG antibodies [34].
RI a auto antibodies
or less commonly, anti IgE auto antibodies [32,33].
Appelmelk et al first demonstrated the molecular
mimicry between H. pylori and lipopolysaccharide
(LPS) and anti-Lewis antibodies in autoimmune
type-B gastritis. [31] Further evidence was provided
by the highly positive autologous serum skin test
(ASST) results in chronic urticaria patients with
H. pylori IgG antibodies [34].
|
DIAGNOSIS OF HELICOBACTER PYLORI |
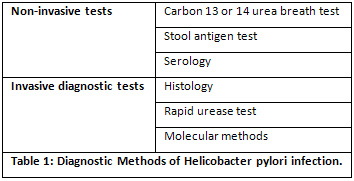
The available diagnostic methods are summarized
in Table 1. Carbon 13 or 14 urea breath test (UBT)
and the stool antigen tests are non-invasive tests
that can be used for testing in the clinical setting.
Serology kits for the presence of antibodies in
the blood can also be applied with high accuracy.
The commonly used medication proton pump inhibitor
leads to false negative breath and stool antigen
tests, but does not affect the results of serological
tests. Proton pump inhibitors should be stopped
at least 2 weeks before performing a breath test
or a stool antigen test. It is recommended to
perform a follow-up test in patients who underwent
H. pylori eradication using urea breath tests.
If this diagnostic procedure is not available
a laboratory-based stool antigen test, preferably
using monoclonal antibodies, could be used [35].
Treatment of H. pylori infection with triple therapy
(a proton-pump inhibitor such as omeprazole 40mg
once daily, amoxicillin 1g twice daily and clarithromycin
500mg twice daily for 7 to 14 days ) cures up
to 90% of individuals. [36].
Type of Sampling: Consecutive sampling
involves taking every subject who presents him/herself
to the hospital over a specified time period.
Study Design: This study is a non controlled
interventional study.
Data collection methods: In the same period
permission was granted by the ethics committee
and informed consent was taken from all patients.
Patients were examined individually. Each patient
with Chronic urticaria had an evaluation sheet
which was filled by the principal investigator
(Table 2) before and after therapy, and the findings
were compared statistically.
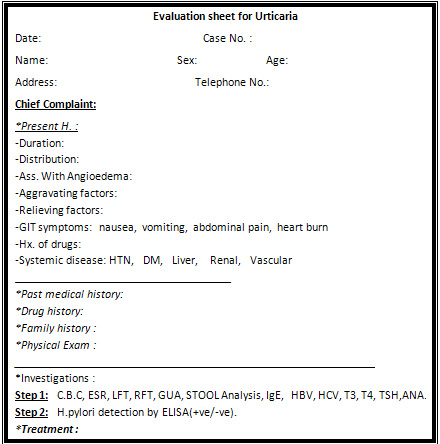
Table 2 : Evaluation sheet for urticaria
Sample size : 60 human subjects.
Methods: Sixty patients attending the dermatology
clinic, at King Khalid Hospital, Najran, Saudi
Arabia during the period from November 2012 to
April 2013 with a history of urticarial lesions
of > 6 weeks as in Figures 1 and 2, were screened
to elicit the possible factors of their chronic
urticaria. The preliminary screening panel for
each patient included complete history, physical
examination and the following laboratory tests:
complete blood count including differential count,
total eosinophil count, sedimentation rate, urine
analysis, liver function test, serum test for
hepatitis B and C, T3 (free), T4 (free), TSH,
anti thyroid antibodies, stool examination for
parasites and ova and total IgE (chemiluminescence).
Each patient who presented with chronic Urticaria
was provided with an evaluation sheet for follow
up (Table 2).
Other tests which were done when indicated by
patients history included: prick test with a panel
of common inhalants and food allergens (animal
dander, pollens, house dust mites, milk, egg,
nut, tomato, wheat, peach, banana), investigation
for focus of infection in various locations (teeth,
upper respiratory and urogenital tract). Patients
with an identifiable cause were treated accordingly
and patients with Chronic Idiopathic Urticaria
(chronic urticaria with no identifiable cause)
were enrolled in the study (Table 2).
Inclusion criteria: All patients of Chronic
Idiopathic Urticaria willing to be enrolled for
the study.
Exclusion criteria: patients suffering
from physical urticaria, patients less than 11
or greater than 60 years of age, pregnant females,
patients who had taken proton pump inhibitors
/antibiotics within the preceding 4 weeks, and
presence of other concomitant serious medical
and surgical diseases.
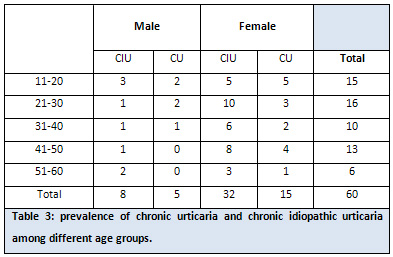
Forty (8 males, 32 females) patients of CIU
(66.7%) with mean age 35.5 years (11-60 years)
were enrolled in this study (Table 3). Blood
sampling was taken from the target population
who complained of chronic idiopathic urticaria
to detect H. pylori IgG and or IgA. Patients
with positive HP in the blood sample were given
first-line therapy comprising omeprazole 20
mg, amoxicillin 1000 mg and clarithromycin 500
mg, twice daily for 14 days.
H. pylori eradication was assessed by Urea Breath
test (which has a sensitivity and specificity
of 95% ). [42] If H. pylori persisted after
first line therapy, patients were offered second
line therapy, comprising omeprazole 20 mg, amoxicillin
1000 mg, metronidazole 500 mg, twice a day for
another 7 days. After completion of therapy,
all infected patients were prescribed antihistamines
to be used as 'rescue medicine'. Non infected
patients were treated with antihistamines or
steroids. All patients were followed up during
the study duration of six months. Also each
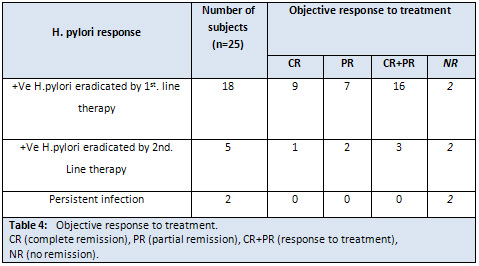
patient's objective response to treatment was
judged using 3 variables based on the need for
'rescue medicine': complete remission (CR -
no need for antihistamines), partial remission
(PR - occasional need for antihistamines), and
no remission (NR -frequent/daily need for antihistamines),(Table.4).
The total number of cases with chronic urticaria
(CU) was 60 patients.
40 patients with Chronic Idiopathic Urticaria
(CIU)
25 patients with (CIU) are (+Ve H.pylori ) M:F
ratio 5:20
15 patients with (CIU) are (-Ve H.pylori ) M:F
ratio 3:12 20 patients with (CU) M:F 5:15
Among 60 patients suffering from chronic Urticaria,
male to female ratio was 13:47. 40 (66.7%) patients
were enrolled in the study with chronic idiopathic
urticaria. 25 (62.5%) patients of chronic idiopathic
urticaria were infected with H.pylori and 15 (37.5%)
patients had negative serology for H.pylori .
80% of patients with positive H.pylori presented
with G.I.T symptoms and 20% without G.I.T symptoms
(Table 5). 18 (72%) infected patients achieved
eradication with first line therapy while 5 (20%)
patients required second line therapy for eradication.
In 2 (8%) patients HP persisted despite two courses
of eradication therapy. Response to eradication
therapy (CR + PR) was evident in 19 (76%) patients
in whom HP was eradicated while 4 (16%) patients
showed no response despite eradication of HP.
Two (8%) patients with persistent HP infection
showed no objective improvement in urticarial
symptoms at the end of study period (Table 4).
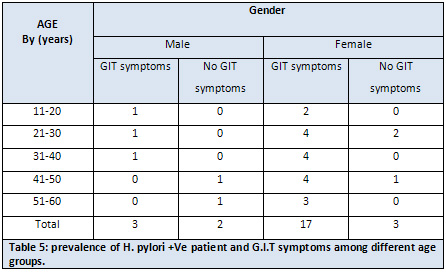

Figure 1: Urticarial lesions on the right side
of the upper limb of a 20 year old male patient

Figure 2: Urticarial lesions on the abdomen of
a 42 year old female patient
The present study was performed to assess the
possible association of HP with CIU. This study
is important because there is high prevalence
of HP infection among the population and there
are conflicting reports of association between
HP infection and CIU from several western studies.
In this study there is high prevalence of HP
infection, with 25 (62.5%) of the patients with
CIU. The high prevalence of HP infection has
been previously reported in other studies, as
well.[37] In the infected patients there is
resolution of urticarial symptoms when HP eradication
therapy was given. This is in concordance with
previous studies, which have shown resolution
of urticaria after HP eradication therapy. [38,39]
However the role of HP as an eliciting factor
for CIU is still controversial. While several
authors have suggested a possible role of HP
in the pathogenesis of CIU, others have shown
no correlation between treatment and remission
of urticaria. [38,40] A recent study in Japanese
university students showed that allergic diseases
are negatively associated with HP infection,
especially in men. [41] Another study showed
that eradication of HP infection by triple therapy
significantly and equally reduces urticarial
activity score in CU patients with positive
and negative autologous serum test.[42]
The discrepancy between results of these different
studies may be due to the different methods
used for detection and establishment of HP infection
or resistance of HP to therapy or recurrences
shortly after successful therapy. The pathogenic
mechanism that may exist between CIU and HP
infection remains unknown. HP by causing inflammation
in the gastrointestinal tract might facilitate
absorption of antigens or unmask existing antigens.
[43] Once this occurs the production of IgE
antibodies responsible for urticarial symptoms
might continue even after eradication of HP.
Thus HP infection may perpetuate the urticarial
tendency of an infected person. [43] HP infection
is frequent, but it triggers urticaria only
in some infected patients, so long duration
studies are needed to establish natural history
of HP infection with respect to urticarial symptoms,
their reinfection and retreatment. Only such
studies will fulfill the Koch's postulate and
only then HP could be labeled as an etiological
factor for CU. [43] Already there are reports
of patient of CU who had gone into remission
after elimination of HP and had a relapse with
reinfection, which again cleared after elimination.
[43] Addition of HP in diagnostic workup of
patients with CIU identifies patients who could
benefit from eradication therapy and thus extends
the treatment options. [44]
The results of our study strongly suggest that
HP should be specifically tested in all patients
of CIU, to identify a subset of patients who
are infected and who could benefit from eradication
therapy. HP should be included in the diagnostic
work up of all patients with CIU.
(1) "Urticaria"
The Oxford English Dictionary.
2nd ed. 1989. OED Online.
Oxford University Press.
2 May 2009.
(2) Tong LJ, Balakrishnan
G, Kochan JP, Kinet JP,
Kaplan AP. Assessment
of autoimmunity in patients
with chronic urticaria.
J Allergy Clin Immunol.
Apr 1997;99(4):461-5.
Medline.
(3) Kaplan AP, Greaves
M. Pathogenesis of chronic
urticaria. Clin Exp Allergy.
Jun 2009;39(6):777-87.
Medline.
(4) Mathelier-Fusade P.
Drug-induced urticarias.
Clin Rev Allergy Immunol.
Feb 2006;30(1):19-23.
Medline.
(5) Yosipovitch G, Greaves
M. Chronic idiopathic
urticaria: a "Cinderella"
disease with a negative
impact on quality of life
and health care costs.
Arch Dermatol. Jan 2008;144(1):102-3.
Medline.
(6) Tebbe B, Geilen CC,
Schulzke JD, Bojarski
C, Radenhausen M, Orfanos
CE. Helicobacter pylori
infection and chronic
urticaria. J Am Acad Dermatol.
Apr 1996;34(4):685-6.
Medline.
(7) Valsecchi R, Pigatto
P. Chronic urticaria and
Helicobacter pylori. Acta
Derm Venereol. Nov 1998;78(6):440-2.
Medline.
(8) Heymann WR. Chronic
urticaria and angioedema
associated with thyroid
autoimmunity: review and
therapeutic implications.
J Am Acad Dermatol. Feb
1999;40(2 Pt 1):229-32.
Medline.
(9) Bansal AS, Hayman
GR. Graves disease associated
with chronic idiopathic
urticaria: 2 case reports.
J Investig Allergol Clin
Immunol. 2009;19(1):54-6.
Medline.
(10) Baty V, Hoen B, Hudziak
H, Aghassian C, Jeandel
C, Canton P. Schnitzler's
syndrome: two case reports
and review of the literature.
Mayo Clin Proc. Jun 1995;70(6):570-2.
Medline.
(11) Sigurgeirsson B.
Skin disease and malignancy.
An epidemiological study.
Acta Derm Venereol Suppl
(Stockh). 1992;178:1-110.
Medline.
(12) Torresani C, Bellafiore
S, De Panfilis G. Chronic
urticaria is usually associated
with fibromyalgia syndrome.
Acta Derm Venereol. 2009;89(4):389-92.
Medline.
(13) Morgan M, Khan DA.
Therapeutic alternatives
for chronic urticaria:
an evidence-based review,
part 1. Ann Allergy Asthma
Immunol. May 2008;100(5):403-11;
quiz 412-4, 468. Medline.
(14) [Guideline] Powell
RJ, Du Toit GL, Siddique
N, et al. BSACI guidelines
for the management of
chronic urticaria and
angio-oedema. Clin Exp
Allergy. May 2007;37(5):631-50.
Medline.
(15) Zuberbier T, Maurer
M. Urticaria: current
opinions about etiology,
diagnosis and therapy.
Acta Derm Venereol. 2007;87(3):196-205.
Medline.
(16) Wai YC, Sussman GL.
Evaluating chronic urticaria
patients for allergies,
infections, or autoimmune
disorders. Clin Rev Allergy
Immunol 2002; 23: 185-93.
(17) Magen E, Mishal J,
Schlesinger M, Scharf
S. Eradication of Helicobacter
pylori infection equally
improves chronic urticaria
with positive and negative
autologous serum skin
test. Helicobacter 2007;
12: 567-71.
(18) Galadari IH, Sheriff
MO. The role of Helicobacter
pylori in urticaria and
atopic dermatitis. Skinmed
2006; 5: 172-6.
(19) Baskan EB, Turker
T, Gulten M, Tunali S.
Lack of correlation between
Helicobacter pylori infection
and autologous serum skin
test in chronic idiopathic
urticaria. Int J Dermatol
2005; 44: 993-5.
(20) Atta AM, Rodrigues
MZ, Sousa CP, Medeiros
Junior M, Sousa-Atta ML.
Autoantibody production
in chronic idiopathic
urticaria is not associated
with Helicobacter pylori
infection. Braz J Med
Biol Res 2004; 37: 13-7.
(21) Fukuda S, Shimoyama
T, Umegaki N, Mikami T,
Nakano H, Munakata A.
Effect of Helicobacter
pylori eradication in
the treatment of Japanese
patients with chronic
idiopathic urticaria.
J Gastroenterol 2004;
39: 827-30.
(22) Di Campli C, Gasbarrini
A, Nucera E, et al. Beneficial
effects of Helicobacter
pylori eradication on
idiopathic chronic urticaria.
Dig Dis Sci 1998; 43:
1226-9.
(23) Buhner S, Reese I,
Kuehl F, Lochs H, Zuberbier
T. Pseudoallergic reactions
in chronic urticaria are
associated with altered
gastroduodenal permeability.
Allergy 2004; 59: 1118-23.
(24) Shiotani A, Okada
K, Yanaoka K, et al. Beneficial
effect of Helicobacter
pylori eradication in
dermatologic diseases.
Helicobacter 2001; 6:
60-5.
(25) Gala Ortiz G, Cuevas
Agustin M, Erias Martinez
P, et al. Chronic urticaria
and Helicobacter pylori.
Ann Allergy Asthma Immunol
2001; 86: 696-8.
(26) Liutu M, Kalimo K,
Uksila J, Savolainen J.
Extraction of IgE-binding
components of Helicobacter
pylori by immunoblotting
analysis in chronic urticaria
patients. Int Arch Allergy
Immunol 2001; 126: 213-7.
(27) Bakos N, Fekete B,
Prohaszka Z, Fust G, Kalabay
L. High prevalence of
IgG and IgA antibodies
to 19-kDa Helicobacter
pylori-associated lipoprotein
in chronic urticaria.
Allergy 2003; 58: 663-7.
(28) Mini R, Figura N,
D'Ambrosio C, et al. Helicobacter
pylori immunoproteomes
in case reports of rosacea
and chronic urticaria.
Proteomics 2005; 5: 777-87.
(29) Greaves MW. Pathophysiology
of chronic urticaria.
Int Arch Allergy Immunol
2002; 127: 3-9.
(30) Farkas H, Gyeney
L, Majthenyi P, Fust G,
Varga L. Angioedema due
to acquired C1-esterase
inhibitor deficiency in
a patient with Helicobacter
pylori infection. Z Gastroenterol
1999; 37: 513-8.
(31) Appelmelk BJ, Simoons-Smit
I, Negrini R, et al. Potential
role of molecular mimicry
between Helicobacter pylori
lipopolysaccharide and
host Lewis blood group
antigens in autoimmunity.
Infect Immun 1996; 64:
2031-40.
(32) Sabroe RA, Fiebiger
E, Francis DM, et al.
Classification of anti-FcepsilonRI
and anti-IgE autoantibodies
in chronic idiopathic
urticaria and correlation
with disease severity.
J Allergy Clin Immunol
2002; 110: 492-9.
(33) Zuberbier T, Henz
BM, Fiebiger E, Maurer
D, Stingl G. Anti-FcepsilonRIalpha
serum autoantibodies in
different subtypes of
urticaria. Allergy 2000;
55: 951-4.
(34) Hizal M, Tuzun B,
Wolf R, Tuzun Y. The relationship
between Helicobacter pylori
IgG antibody and autologous
serum test in chronic
urticaria. Int J Dermatol
2000; 39: 443-5.
(35) Malfertheiner P,
Megraud F, O'Morain C,
et al. Current concepts
in the management of Helicobacter
pylori infection: the
Maastricht III Consensus
Report. Gut 2007; 56:
772-81.
(36) Vakil N, Lanza F,
Schwatrz H, et al. Seven-day
therapy for Helicobacter
pylori in the United States.
Aliment Pharmacol Ther
2004;20:99-107.
(37) Jais M, Baruna S.
Seroprevalence of anti
Helicobacter pylori IgG/IgA
in asymptomatic population
from Delhi. J Commun Dis
2004;36:132-5.
(38) Wedi B, Wagner S,
Werfel T, Manns MP, Kapp
A. Prevalence of Helicobacter
pylori gastritis in chronic
urticaria. Int Arch Allergy
Immunol 1998;116:288-94.
(39) Dauden E, Alionso
IJ, Diez AG. H. pylori
and chronic idiopathic
urticaria. Int J Dermatol
2000;39:446-52.
(40) Valsecchi R, Pigatto
P. Chronic urticaria and
Helicobacter pylori. Acta
Derm Venerol (Stockh)
1998;78:440-2.
(41) Shiotani A, Miyanishi
T, Kamada T, Harumak K.
Helicobacter infection
and allergic diseases:
Epidemiological study
in Japanese University
students. J Gastroenterol
Hepatol 2007 (epub ahead
of print).
(42) Magen E, Mishal J,
Schlesinger M, Scharf
S. Eradication of HP infection
equally improves chronic
urticaria with positive
and negative autologous
serum skin test. Helicobacter
2007;12:567-71.
(43) Zuberbier T. Urticaria
Review. Allergy 2003;58:1224-34.
(44) Zuberbier T, Chantraine-Hess
S, Hartmann K, Czarnetzki
BM. Pseudo allergen-free
diet in treatment of chronic
urticaria: A prospective
study. Acta Derma Venerol
(Stockh) 1995;75:484-7.
|
|
.................................................................................................................

|
| |
|

