Knowledge,
Attitude, Practice And Barriers Of Effective Communication
Skills During Medical Consultation Among General
Practitioners National Guard Primary Health Care
Center,Riyadh, Saudi Arabia
Basmah
Saleh Al-Zahrani (1)
Maryam Fahad Al-Misfer (2)
Ali Mohsen Al-Hazmi (3)
(1) Dr. Basmah Saleh Al-Zahrani, MMBS, SB-FM,
AB-FM
Senior registrar , Family Medicine Unit , King
Khalid University Hospital
Riyadh, Saudi Arabia
(2) Dr. Maryam Fahad Al-Misfer, MMBS, SB-FM,
AB-FM
Assistant trainer and Senior registrar
Department of Family and Community Medicine,
King Khalid University Hospital
Riyadh, Saudi Arabia
(3) Dr.Ali Mohsen Al-Hazmi
Consultant and Assistant professor
Deprtment of Family and Community Medicine,
King Khalid University Hospital
Riyadh, Saudi Arabia
Correspondence:
Dr.Maryam Fahad Al-Misfer
MMBS, SB-FM, AB-FM
Assistant trainer and Senior registrar
Department of Family and Community Medicine,
King Khalid University Hospital
Riyadh, Saudi Arabia
Email:
mfalmisfer@yahoo.com
|
Abstract
Objectives:To assess barriers,
practice attitude and knowledge of primary
health care physicians about communication
skills during medical consultations in
primary health care centers in National
Guard Hospital in Riyadh, Saudi Arabia.
Design:
Cross sectional study
Methodology:
The study was conducted during the
period from November 2009 till July 2010.
Seventy primary care physicians answered
a structured questionnaire about their
knowledge, practice and barrier of effective
communication skills during medical consultations.
Results:
Survey of 70 PHC physicians showed 25(35.7%)
residents, 28(40%) specialized. The majority
of the physicians did receive some form
of training for communication skills (85.7%),
however, they did perceive lack of proper
training (68.5%) as a barrier also. Common
patient barriers to better communication
with patients were different cultural
norms from physicians or different gender
(51.4%). A system related barrier noted
by physicians was lack of time (82.8%).
Mean score of practicing communication
skills was 37.2/60 and mean knowledge
score was 3.31/6 for the physicians in
our study. No relationship between knowledge
and practice was noted in our study but
a positive correlation between age, years
of experience and practicing communication
skills was found ( F-statistic 5.6, p
value 0.006). Practice scores were significantly
different for residents, staff physicians
and specialists. Physicians who were confident
of their communication skills and who
made a concious effort to apply the skills
that they had learned were shown to score
better on practicing these communication
skills, Chi-sq 30.11 p value <0.001,
and Chi-sq. 12.67 p value 0.002, respectively.
Conclusion:
Knowledge of communication skills
can improve with training however having
the knowledge does not affect the practice
of communication skills unless the physician
is self-confident and has the right attitude
of consciously applying that knowledge
in his/her practice and improvement comes
with age and experience.
Key words:
communication skills, barrier, practice,
knowledge, atittude , primary health care
physicians.
|
The expectations of the public from health
care providers have increased over the last
few decades and the majority are familiar with
their rights in the health care system. As a
consequence, it is of high priority that health
care providers have effective communication
skills. It has been well documented that the
doctor-patient relationship is central to the
delivery of high quality medical care. It has
been shown to affect patient satisfaction, to
decrease the use of pain killers, to shorten
hospital stays, to improve recovery from surgery
and a variety of other biological, psychological
and social outcomes [1-4].
Good communication skills are integral to medical
and other healthcare practice. Communication
is important not only to professional-patient
interaction but also within the healthcare team.
The benefits of effective communication include
good working relationships and increased patient
satisfaction. Effective communication may increase
patient understanding of treatment, improve
compliance and lead to improved health outcomes.
It can also make the professional-patient relationship
a more equitable one. Undoubtedly however, there
are barriers to effective communication ranging
from personal attitudes, to the limitations
placed on doctors by the organizational structures
in which they work [5].
In order to deliver effective healthcare, doctors
are expected to communicate competently both
orally and in writing with a range of professionals,
managers, patients, families and carers. Simply
recognizing the need for good communication
skills is not enough; healthcare professionals
must actively strive to achieve good communication
skills by evaluating their own abilities. Education
providers need to ensure that appropriate and
effective training opportunities are available
to doctors to develop and refine such skills
in order to facilitate interaction with patients
and others [5].
Benefits of good communication can be identified
for both doctors and patients.
Benefits for patients
• The doctor-patient relationship is improved.
The doctor is better able to seek the relevant
information and recognize the problems of the
patient by way of interaction and attentive
listening. As a result, the patient's problems
may be identified more accurately [6].
• Good communication helps the patient
to recall information and comply with treatment
instructions thereby improving patient satisfaction
[7, 8]
• Good communication may improve patient
health and outcomes. Better communication and
dialogue by means of reiteration and repetition
between the doctor and patient has a beneficial
effect in terms of promoting better emotional
health, resolution of symptoms and pain control
[9].
• The overall quality of care may be improved
by ensuring that patients' views and wishes
are taken into account as a mutual process in
decision making.
• Good communication is likely to reduce
the incidence of clinical error [6]
Benefits for doctors
• Effective communication skills may relieve
doctors of some of the pressures of dealing
with the difficult situations encountered in
this emotionally demanding profession. Problematic
communication with patients is thought to contribute
to emotional burn-out and low personal accomplishment
in doctors as well as high psychological morbidity
[10]. Being able to communicate competently
may also enhance job satisfaction.
• Patients are less likely to complain
if doctors communicate well. There is, therefore,
a reduced likelihood of doctors being sued.
In all doctor-patient interactions a variety
of communication skills are required for different
phases of the consultation. During the start
of a consultation, doctors must establish a
rapport and identify the reasons for the consultation.
They must go on to gather information, structure
the consultation, build on the relationship
and provide appropriate information [11]. There
is a trend in healthcare on pushing the need
for strong communication skills in medicine.
In relation to communication with patients,
an increasing focus on shared decision making
and communication of risk, are two of the most
important factors [12]. For example, communication
skills can help healthcare staff to explain
the results of epidemiological studies or clinical
trials to individual patients in ways that can
help patients to understand risk [13]. Doctors
can do this more effectively if they develop
relationships with their patients and if they
take into account knowledge and perceptions
of health risks in the general public [14].
Recent research shows that poor communication
between healthcare staff and patients is still
all too common. For example, when the Lothian
Hospitals NHS Trust in Scotland asked patients
for their views on communication issues, they
found that 60 per cent of patients complained
about a lack of involvement in decisions about
their care, 33 per cent said they had been given
no explanation of test results and 31 per cent
said they had no opportunity to talk to the
doctor. Twenty-three per cent complained of
nurses and doctors saying different things [6].
The General Medical Council (GMC) in London
stresses the need for communication skills in
a number of its guidance notes [15-18]. The
GMC recognizes that the communication skills
required throughout a doctor's career are likely
to change. Doctors should review their skills
as part of their continuing professional development,
and take part in educational activities as a
means of maintaining and further developing
their competence [16].
Other medical professional bodies have highlighted
the importance of communication skills and instituted
various approaches for communication skills
education.
Examples of professional endorsement of the
importance of communication skills for doctors:
• Publications from medical organizations,
such as the BMA's board of medical education
report on communication skills and continuing
professional development (1998) [19] and the
Royal College of Physicians' publication Improving
communication between doctors and patients (1997),
[20] have highlighted the importance of communication
skills.
• The General Medical Council's Professional
Linguistic and Assessment Board (PLAB) examination
has separated its language and communication
elements with the latter being assessed through
role play.
• The Academy of Medical Royal Colleges,
in its recommendations for general professional
training, includes communication skills among
the generic skills required of all trainees.
• Royal Colleges include communication
skills assessment in their training. For example,
the Royal College of General Practitioners has
developed formal mechanisms using video recordings
for assessing communication skills in candidates
[3]. The Royal College of Physicians has introduced
communication skills assessment into its training.
The Royal College of Ophthalmologists includes
communication skills in both the basic higher
specialist training curricula and in the Part
3 MRCOphth examination.
• The London Deanery and NHS London have
developed an online interactive educational
program in communication skills for healthcare
professionals, including postgraduate doctors
undertaking the foundation years of training:
www.healthcareskills.nhs.uk.
The potential of communication skills education
There is substantial evidence that communication
skills can be taught, particularly using experiential
methods [21].
To be effective, communication skills teaching
should include [7]:
• Evidence of current deficiencies in communication,
reasons for them, and the consequences for patients
and doctors
• An evidence base for the skills needed
to overcome these deficiencies
• A demonstration of the skills to be learnt
• An opportunity to practice the skills
under controlled and safe conditions
• Constructive feedback on performance
and reflection on the reasons
The potential of communication skills education
There is substantial evidence that communication
skills can be taught, particularly using experiential
methods [21].
To be effective, communication skills teaching
should include [7]:
• Evidence of current deficiencies in communication,
reasons for them, and the consequences for patients
and doctors
• An evidence base for the skills needed
to overcome these deficiencies
• A demonstration of the skills to be learnt
• An opportunity to practice the skills
under controlled and safe conditions
• Constructive feedback on performance
and reflection on the reasons For example, it
has been suggested that most do not include
sufficient information about the training given
to the study participants, making evaluation
difficult [26]. However, there is overwhelming
proof that communication skills in the patient-doctor
relationship can be taught and are learnt [22].
The problem of doctor-patient communication
is more evident in Saudi Arabia for the following
reasons: Firstly, the number of foreign personnel
in health services is rather large [23]. This
workforce communicates with patients and with
one another in a variety of languages different
from the local one. In addition, not much orientation
is given to them on local traditions and the
prevalent health-related beliefs and culture.
Secondly, this manpower deals with a sizeable
sector of consumers, who are themselves expatriate
and speak a variety of languages, and hold health
related traditions and beliefs. This situation
naturally creates a complex environment for
doctor-patient communication. A recent study
from Riyadh [24] alluded to the relationship
between patient satisfaction and doctor-patient
communication. As in other parts of the world,
people in Saudi Arabia are expected to attempt
to find out and understand all aspects of their
health problems [25]. Hence the need to train
and orientate physicians in the skills related
to doctor-patient communication assumes greater
significance. In this regard, several methods
of training, especially for the situation of
Saudi Arabia, can be employed [26-27].
In Saudi Arabia, the acquisition of the skill
of doctor-patient communication hardly exists
in any undergraduate or postgraduate medical
curriculum. There is also paucity of research
in this area. Consequently, it is vital that
comprehensive research be done to clarify the
needs of students and professionals, and outline
the objectives and the modalities of training
in this skill [28].
Research result of study done in KSA, to explore
patient's expectations before consulting their
general practitioners (GPs) and determine the
factors that influence them, showed 74.6% of
the patients preferred Saudi doctors, and 92.6%
would like to have more laboratory tests for
the diagnosis of their illnesses while more
than two thirds of the patients (78.0%) felt
entirely comfortable when talking with GPs about
the personal aspects of their problems and about
half thought that the role of GP was mainly
to refer patients to specialists, while 55.2%
believed that the GP cannot deal with the psychosocial
aspect of organic diseases, and the commonest
reason for consulting GPs was for a general
check up. So, the conclusion was that the GP
has to explore patients' expectations so that
they can either be met or their impracticality
explained. GPs should search for patients' motives
and reconcile this with their own practice.
The GP should be trained to play the standard
role of Primary Care Physician [29].
This
study
attempts
to
explore:
1.
Current
practices
of
communication
skills
of
primary
health
care
physicians
in
health
care
centers
in
National
Guard
Health
Affairs
in
Riyadh.
2.
Main
barriers
that
can
affect
doctor-patient
communications.
3.
Primary
health
care
physicians'
knowledge
about
effective
doctor-patient
communications.
Study
Design:
This
is
a
cross-sectional
study.
Setting:
Held
in
National
Guard
Primary
Health
Care
Centers
in
Riyadh.
Duration
of
Study:
This
study
was
held
during
the
period
from
November
2009
till
July
2010.
Sample
Size:
Seventy
primary
health
care
physicians
participated.
Sampling
Technique:
Survey
questionnaire
was
distributed
to
willing
participants.
Sample
Selection:
All
primary
health
care
physicians
of
different
levels
and
qualifications.
Data
Collection
Procedure:
Data
for
this
study
were
collected
by
questionnaire
which
was
distributed
during
Sunday
morning
professional
education
activity
of
the
department
of
Family
Medicine
and
Primary
Healthcare
in
each
center
for
physicians
and
Half
Day
Release
Course
in
Monday
morning
activity
for
residents.
Data
Collection
Instrument:
Questionnaire
consisted
of
four
sections.
The
first
section
asked
for
physicians'
demographic
data,
educational
items
and
to
rate
their
communication
skills
with
patients.
The
second
section
asked
about
common
barriers
which
can
affect
communication
skills.
The
third
section
asked
about
the
current
practice,
and
the
fourth
asked
about
the
physician's
knowledge
about
communication
skills
by
giving
them
a
sentence
and
asked
about
what
kind
of
skills
that
sentence
indicates.
Ethical
Consideration:
Anonymity
was
maintained
throughout.
The
subjects
received
the
self-administered
questionnaire
with
a
cover
letter
explaining
the
project
and
the
subject's
rights.
The
choice
of
the
items
in
the
questionnaire
was
based
on
the
level
of
communication
skills
a
General
Practitioner
needs.
Data
Analysis
Procedure:
Once
the
data
collection
was
completed,
it
was
checked
and
entered
into
the
computer
using
the
Statistical
Package
for
Social
Sciences
(SPSS),
version
15.
Descriptive
analysis
of
mean,
median
mode,
frequencies
and
percentages
were
carried
out
on
most
of
the
variables,
including,
age,
gender,
self-rating
of
skills,
years
of
experience,
levels
of
experience,
training
history,
communication
skill
practices
and
knowledge
scores.
In
addition,
relationships
were
explored
using
chi-square,
linear
regression,
Kruskal
Wallis
and
Mann
Whitney
where
needed.
A
total
of
70
primary
health
care
physicians
participated
in
the
study.
Table
1
shows,
30
(42.9%)
were
male
and
40
(57.1%)
were
female.
Maximum
age
was
58
years
old
and
minimum
age
26
years.
Fifty-one
(72.9%)
were
Saudi,
19
(27.1%)
were
non-Saudi.
The
physicians
position
were
25(35.7%)
residents,
17(24.3%)
MBBS/MD
and
28(40%)
specialists.
The
maximum
years
of
experience
were
25
years
and
minimum
was
2
years.
Table
1:
Demographic
data
of
participants
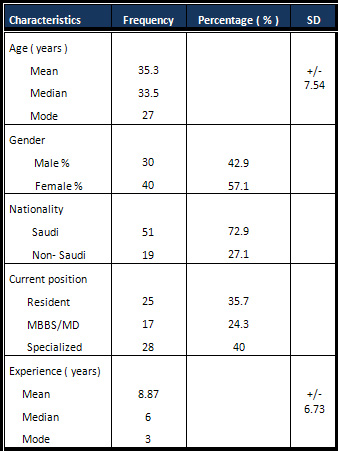
Table
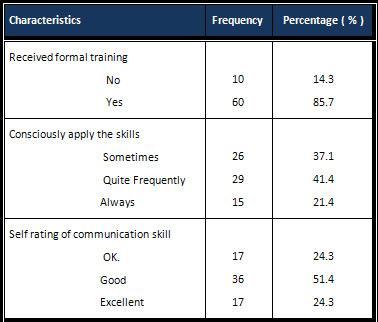
2
shows
that
14.3%
of
the
physicians
did
not
receive
formal
training
about
communication
skills
during
medical
consultations,
while
85.7%
did
receive
formal
training.
Over
two-thirds
of
the
primary
care
physicians
consciously
applied
specific
communication
skills
frequently
in
their
daily
practice.
On
a
self
rating
scale
of
communication
skills
(1-4
scale)
over
75%
of
the
physicians
rated
their
communication
skills
as
good
or
excellent.
Table
2:
Communication
skills:
training
and
attitude
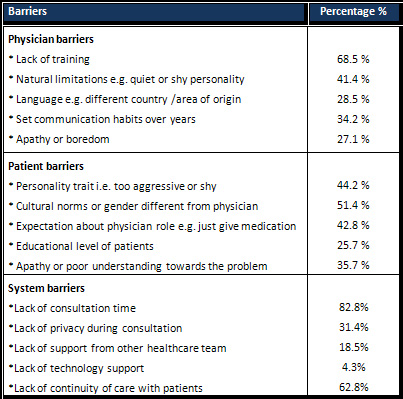
Barriers
of
effective
communication
skills
were
divided
into
three
categories:
physician,
patient
and
system
barriers
[Table
3].
The
two
most
significant
physician
barriers
were
lack
of
formal
training
(68.5%)
and
natural
limitations
e.g.
quiet
or
shy
personality
(41.4%).
The
two
most
significant
patient
barriers
to
communication
skills
reported
by
physicians,
were
cultural
norms
or
gender
different
from
physicians
(51.4%)
and
personality
trait
of
patient,
i.e.
too
aggressive
or
shy
(44.2%).
The
two
most
significant
system
barriers
as
perceived
by
physicians
were
lack
of
consultation
time
(82.8%)
and
lack
of
continuity
of
care
with
patients,
i.e.
patient
seen
by
different
doctor
each
time
(62.8%).
Table
3:
Barriers
to
effective
communication
skills
in
medical
consultation
Click
here
for
Table
4:
Communication
of
skill
practice
pattern
and
PHC
physicians
Table
4
Shows
that
nearly
69%
of
physicians
rarely
or
sometimes
involved
the
patient
in
decision
making;
another
70%
rarely
or
sometimes
discussed
goals
of
consultation
with
their
patients
or
used
'pause
or
silence'
in
communicating
with
their
patients.
Around
2/3rds
of
physicians
rarely
or
sometimes
inquire
about
the
person
accompanying
the
patient.
For
female
patients
there
were
73.2%
of
female
physicians
who
rarely
or
sometimes
felt
the
need
to
ask
their
female
patients
to
remove
their
face-cover
in
daily
practice
to
assess
their
facial
expressions
better.
Table
5:
Communication
skills
knowledge
score
percentages
of
physicians
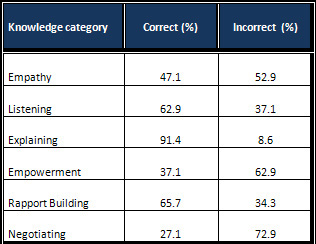
In
Table
5
the
majority
of
empathy,
empowerment
and
negotiating
knowledge
were
answered
incorrectly
while
the
majority
of
listening,
explaining
and
building
rapport
knowledge
were
answered
correctly.
Figure
1:
Distribution
of
practice
scores
among
physicians
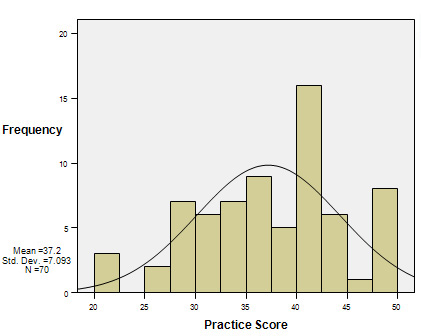
The
total
maximum
score
of
practice
questions
was
60.
Figure
1
shows
mean
of
practice
score
37.2,
SD
+/-
7.093,
maximum
score
49
and
minimum
score
20.
Questions
#
13
&
17
were
excluded
from
the
total
score
(See
Table
4).
For
each
question
the
value
ranged
from
1-4.
Total
score
for
each
physician
was
added
and
all
scores
are
presented
in
Figure
1.
Figure
2:
Distribution
of
knowledge
scores
among
physicians
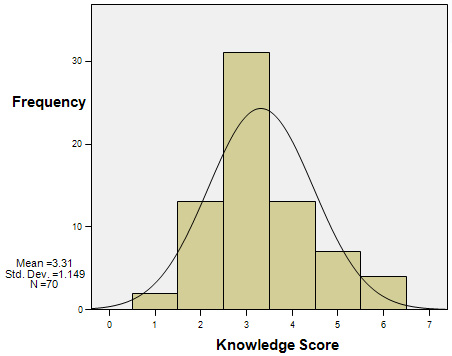
The
total
score
of
the
knowledge
questions
was
6.
If
a
physician
answered
a
question
correctly
one
score
was
awarded.
Thirty-one
(44.3%)
physicians
scored
3
out
of
6.
Figure
3:
Relationship
between
knowledge
and
practice
scores
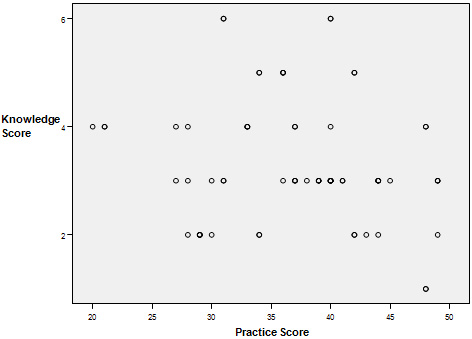
Figure
3
shows
no
relationship
between
score
of
knowledge
and
practice
of
communication
skills
based
on
linear
regression.
Figure
4:
Relation
between
Age
and
Practice
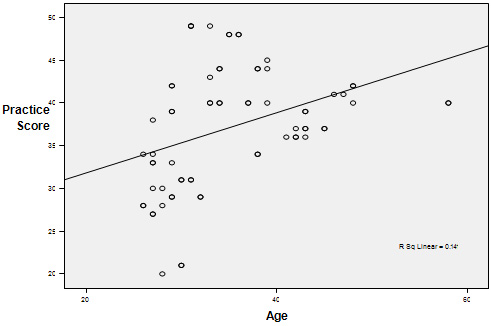
Figure
5:
Relation
between
Years
of
Experience
and
practice
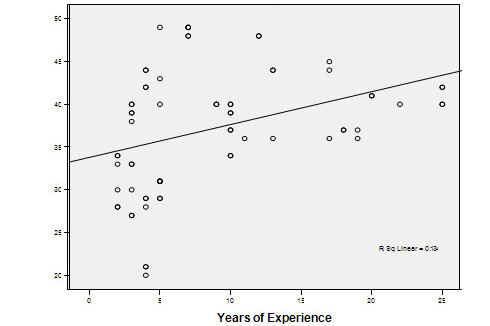
Figures
4
&
5
show
that
age
of
physician
and
years
of
experience
are
positively
correlated
to
practice
scores.
Linear
regression
of
age
and
years
of
experience
with
practice
scores
yielded
an
R
Square
0.143,
F
statistic
5.602
and
P
value
0.006.
Table
6:
Relationship
of
practice
scores
&
communication
skill
values
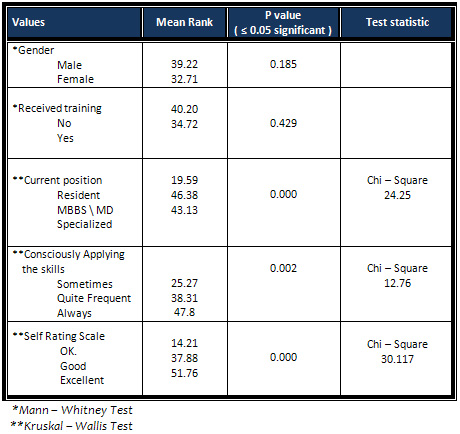
The
score
of
practicing
communication
skills
was
found
to
be
not
significantly
different
based
on
gender
of
physicians.
Using
Kruskal-Wallis
Test
it
showed
that
communication
skills
practice
scores
were
significantly
different
between
resident,
MBBS/MD
and
specialists
[Table
6].
Table
7:
Relationship
of
knowledge
scores
&
specific
variables
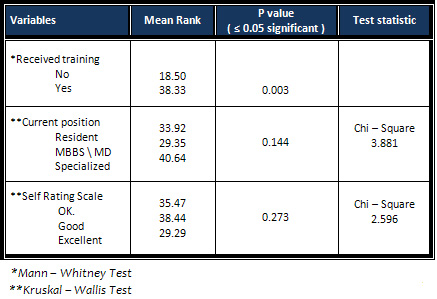
The
score
of
knowledge
of
communication
skills
was
significantly
different
based
on
whether
the
physicians
received
training
or
not
[Table
7],
however
there
was
no
statistically
significant
difference
between
the
knowledge
scores
on
the
basis
of
current
position,
self-confidence
of
practicing
skills
or
application
of
communication
skills
consciously.
Multiple
comparisons
was
done
using
Post
Hoc
Tukey
test
between
practice
scores
and
current
position
of
participants.
It
showed
there
is
a
real
difference
between
communication
skills
practice
score
of
residents
with
that
of
MBBS/MD
or
specialized
physicians
but
there
was
no
difference
between
MBBS/MD
practice
score
and
specialized
physicians.
Applying
communication
skills
consciously
was
influenced
by
the
current
position
of
physicians;
most
residents
in
a
sample
(25)
applied
their
communication
skills
rarely
or
infrequently
whereas
23
of
the
28
specialized
physicians
applied
their
skills
quite
frequently,
Chi-square
15.505
and
P
value
0.004.
The
residents
were
less
confident
of
their
communication
skills,
while
MBBS/MD
physicians
and
specialized
physicians
rated
their
communication
skills
as
good
and
excellent,
chi-square
13.754
and
P
value
0.008.
This
study
provides
information
not
previously
available
from
National
Guard
primary
health
care
physicians
on
the
knowledge,
attitude,
practice
and
barriers
of
effective
communication
skills
during
medical
consultation.
The
distribution
of
population
was
almost
equal
between
male
(42.9%)
and
female
(57.1%),
the
majority
of
them
were
Saudis
(72.9%),
between
residents
(35.7%),
specialized
(40%)
and
staff
physicians
(24.3%).
Average
years
of
experience
in
primary
care
ranged
between
2-25
years.
Most
of
the
physicians
did
receive
formal
training
of
communication
skills
in
our
study
(Table
2).
Communication
skills
training
has
been
embedded
in
the
curriculum
of
graduate
medical
and
post-graduate
trainings
for
over
15
years
in
some
parts
of
the
world
[5].
Over
forty
percent
of
physicians
applied
communication
skills
frequently
and
51.4%
rated
themselves
as
good
communicators
(Table
2).
Most
of
the
physicians
thought
that
lack
of
training
(68.5%),
cultural
norms
or
gender
difference
between
patient
and
doctors
(51.4%),
and
lack
of
time
(82.8%)
are
the
main
barriers
to
apply
effective
communication
skills
with
patients.
In
our
study,
one
of
the
main
patient
related
barriers,
as
perceived
by
the
physicians,
was
different
cultural
norms
or
gender
from
that
of
the
physician.
There
is
one
study
that
showed
the
majority
of
patient's
preferred
Saudi
doctors,
suggesting
that
doctor-patient
communication
is
much
easier
when
both
patient
and
doctor
come
from
the
same
culture
[29].
In
the
same
study
most
patients
expected
GPs
to
spend
some
time
explaining
the
nature
of
their
illnesses
and
the
results
of
tests
done
[29].
This
is
consistent
with
the
findings
of
other
studies
[30]
and
this
study,
as
most
physicians
answered
correctly
the
knowledge
question
about
explaining
to
the
patient
in
detail,
as
an
important
communication
skill
(Table
5).
A
study
conducted
to
assess
the
impact
of
two
communication
skills
training
programs
on
the
evolution
of
patients'
anxiety
following
a
medical
consultation
found
no
significant
difference
was
observed.
Results
of
that
study
confirm
results
of
other
studies
that
have
shown
that
some
reassurance
may
produce
anxiety
and
have
suggested
that
communication
skills
are
probably
efficient
if
physicians
discuss
their
patients'
concerns
in
depth
by
using
some
basic
communication
screening
questions
[31].
In
this
study
using
non-verbal
cues
to
communicate
with
patients
were
obviously
rarely
and
sometimes
used
(Table
4).
In
other
studies
they
found
that
patients
offer
clues
that
present
opportunities
for
physicians
to
express
empathy
and
understand
patients'
lives.
In
both
primary
care
and
surgery,
physicians
tend
to
bypass
these
clues,
missing
potential
opportunities
to
strengthen
the
patient-physician
relationship.
Research
on
teaching
communication
skills
demonstrates
that
physicians
can
learn
to
modify
their
communication
style
[32-34].
Despite
widespread
interest
in
the
effects
of
physician
gender
on
the
care
process,
the
literature
describing
these
effects
is
small
[35],
and
in
this
study
there
were
no
differences
between
male
and
female
physicians
in
practicing
communication
skills.
It
was
observed
in
this
study
that
there
was
no
correlation
between
knowledge
and
practice
of
communication
skills
(Figure
3)
suggesting
a
gap
between
knowledge
and
practice.
It
was
also
noted
that
the
physicians
who
consciously
applied
the
communication
skills
in
their
practice,
scored
better
in
daily
practice
of
these
skills
with
their
patients.
The
physician
may
have
knowledge
but
if
he
did
not
make
a
deliberate
effort
to
apply
that
knowledge
in
his
practice,
it
did
not
show
in
his
actual
practice.
Most
residents
received
training
of
communication
skills
during
their
program
but
they
seemed
to
apply
these
skills
in
their
daily
practice
to
a
lesser
degree
than
the
MBBS/MD
and
specialized
physicians
(Table
6).
Communication
skill
training
is
very
important
to
have
knowledge
of
skills
but
having
a
good
knowledge
did
not
affect
the
practice
if
the
physician
did
not
have
the
attitude
of
applying
that
knowledge
in
the
practice
(Table
7).
Specialized
and
MBBS/MD
physicians
were
more
confident
in
their
self
rating
of
communication
skills,
while
the
majority
of
residents
evaluated
their
communication
skills
with
lesser
self-confidence.
This
translated
into
better
practice
scores.
Figure
4
and
5
show
there
is
a
strong
relation
between
age
and
years
of
experience
in
the
medical
field
with
practicing
of
communication
skills.
Years
of
practice
was
found
to
be
a
larger
predictor
of
practicing
communication
skills
when
compared
to
age,
however
both
factors
had
significant
overlap,
suggesting
that
with
increasing
age
and
experience
in
work,
physicians
practiced
their
communication
skills
more.
A
study
showed
that
the
level
of
communication
skills
and
the
content
of
the
consultation
with
regard
to
psychosocial
issues,
patient
concerns
and
the
informing
and
planning
of
procedures
(with
a
representative
patient
in
a
general
practice
setting)
among
graduate
medical
students
are
significantly
correlated;
that
means
having
the
knowledge
of
communication
skills
is
important
[36],
however
in
this
study,
age
and
years
of
experience
were
more
important
than
having
good
knowledge
only.
It
means
that
training
is
important
but
having
self
confidence
and
a
genuine
desire
to
apply
that
knowledge
are
valuable
in
practicing
communication
skills,
which
certainly
improves
with
age
and
experience.
There
are
four
limitations
of
this
study
which
deserve
emphasis:
1.
Small
sample
size.
2.
Study
was
done
among
primary
health
care
physicians
in
National
Guard
which
cannot
be
generalized
to
PHC
physicians
in
Saudi
Arabia.
3.
Majority
of
the
sample
was
Saudi
and
35.7%
were
residents.
4.
Only
six
categories
evaluated
the
knowledge
of
physicians.
This
study
suggests
that
knowledge
base
in
communication
skills
can
improve
with
training
however
having
the
knowledge
of
good
communication
with
patients
does
not
influence
the
practice
of
communication
skills
unless
the
physician
is
self-confident
and
has
the
right
attitude
of
consciously
applying
that
knowledge
in
his/her
practice.
Lastly,
communication
skills
improve
with
age
and
experience.
1.
Younger
physicians
need
to
put
more
emphasis
on
the
use
of
communication
skills;
having
the
knowledge
is
not
sufficient.
2.
Involve
the
less
expert
physician
in
a
teaching
clinic
or
increase
the
number
of
simulated
clinics
during
the
training
of
communication
skills
program
and
improving
the
continuity
of
care
between
physicians
and
their
patients
will
show
good
outcomes
in
improving
the
application
of
those
skills.
3.
How
can
doctors
best
continue
to
develop
their
skills,
apply
them
within
their
daily
work,
survive
emotionally,
and
feel
more
satisfied?
How
can
persistent
behavioral,
perceptual,
and
personal
changes
be
produced?
Self
learning
and
self
monitored
feedback,
distance
learning,
and
serial
workshops
seem
to
be
promising
approaches
for
qualified
doctors.
4.
Finally,
it
is
my
hope
that
the
findings
will
help
in
planning
a
strategy
for
improving
services,
making
effective
communication
skills
attitude
more
acceptable
and
believable
in
the
PHC
sitting
in
our
community
to
improve
patient
care
in
all
aspects.
1.
Haidet
P
,
Dians
JE,
Paterniti
DA,
Hechtel
L,
Chang
T,
Tseng
E,
Rogers
JC.
Medical
student
attitudes
toward
the
doctor-patient
relationship.
Med
Educ.
2002;36:568-574.
2.
Cegala
DJ,
Lenzmeier
Broz
S.
Physician
communication
skill
training:
a
review
of
theoretical
backgrounds,
objectives
and
skills.
Med
Educ
2002,
36(11):1004-1016.
3.
Brown
JB,
Boles
M,
Mullooly
JP,
Levinson
W:
Effect
of
clinician
communication
skills
training
on
patient
satisfaction.
A
randomized,
controlled
trial.
Ann
Intern
Med
1999,
131(11):822-829.
4.
Ong
LM,
de
Haes
JC,
Hoos
AM,
Lammes
FB:
Doctor-patient
communication:
a
review
of
the
literature.
Soc
Sci
Med
1995,
40(7):903-918.
5.
British
Medical
Association
(2004)
Communication
skills
education
for
doctors
an
update.
London:
BMA.
6.
Centre
for
Change
and
Innovation
(2003).
Talking
matters:
developing
the
communication
skills
of
doctors.
Edinburgh:
Scottish
Executive.
7.
Maguire
P
&
Pitceathly
C
(2002).
Key
communication
skills
and
how
to
acquire
them.
BMJ
325:
697-700.
8.
Hulsman
R
et
al
(2002).
The
effectiveness
of
a
computer-assisted
instruction
programme
on
communication
skills
of
medical
specialists
in
oncology.
Medical
Education
36:
125-34
9.
Meryn
S
(1998).
Improving
doctor-patient
communication.
BMJ
316:1922-30.
10.
Feinmann
J
(2002).
Brushing
up
on
doctors'
communication
skills.
The
Lancet.
360:
1572.
11.
Gull
SE
(2002).
Communication
skills:
recognizing
the
difficulties.
The
Obstetrician
and
Gynecologist.
4:107-9.
12.
Spencer
JA
&
Silverman
J
(2004).
Communication
education
and
assessment:
taking
account
of
diversity.
Medical
Education.
38:
116-8.
13.
Sedgwick
P
&
Hall
A
(2003).
Teaching
medical
students
and
doctors
how
to
communicate
risk.
BMJ.
327:
694-5.
14.
Alaszewski
A
&
Horlick-Jones
T
(2003).
How
can
doctors
communicate
information
about
risk
more
effectively?
BMJ.
327:
728-30.
15.
The
General
Medical
Council
(2002).
Tomorrow's
doctors:
recommendations
on
undergraduate
medical
education.
London:
GMC.
16.
General
Medical
Council
(2001).
Good
medical
practice.
London:
GMC.
17.
General
Medical
Council
(1997)
.The
new
doctor.
London:
GMC.
18.
General
Medical
Council
(1998).
The
early
years.
London:
GMC.
19.
British
Medical
Association
(1998).
Communication
skills
and
continuing
professional
development.
London:
BMA.
20.
Royal
College
of
Physicians
of
London
(1997).
Improving
communication
between
doctors
and
patients.
London:
RCP.
21.
Roter
DL,
Larson
S
&
Shintzky
H
et
al
(2004).
Use
of
an
innovative
video
feedback
technique
to
enhance
communication
skills
training.
Medical
Education.
38:
145-7.
22.
Aspegren
K
(1999)
Teaching
and
learning
communication
skills
in
medicine
-
a
review
with
quality
grading
of
articles.
Medical
Teacher.
21:
563-70.
23.
Ministry
of
Health.
Annual
Health
Report.
Riyadh:
Alhilal
House
press;
1418H.
24.
Weis
R,
Stuker
R.
When
patients
and
doctors
don't
speak
the
same
language:
concepts
of
interpretation
practice.
Soz
Preventmed
1999;44(6):257-63.
25.
Saeed
AA,
Mohammed
BA,
Magzoub
ME,
Al-Doghaither
AH.
Satisfaction
and
correlates
of
patient's
satisfaction
with
physicians'
services
in
primary
health
care
centers.
Saudi
Med
J
2001;
22(3):
262-7.
26.
Dube
CE,
O'Donnell
JF,
Novack
DH.
Communication
skills
for
preventive
intervention.
Acad
Med
2000;
75(7
suppl):S45-54.
27.
Hongladarom
S,
Phaosavasdi
S,
Tneepanichskul
S,
Tannirandon
Y,
Wilde
H,
Prukspong
C.
Humanistic
learning
in
medical
curriculum.
Med
Assoc
Thai
2000;
83(8):969-74.
28.
Ahmed
G.
Elzubier.
Doctor-patient
communication:
a
skill
needed
in
Saudi
Arabia.
Journal
of
Fm
&
Community
Medicine
2002;
9(1):30-35.
29.
Khalid
A.
Bin
Abdulrahman.
What
do
patient's
expect
of
their
general
practitioners?
Journal
of
Fm
&
Community
Medicine
2003;
10(1):39-46.
30.
Williams
S,
Weinman
J,
and
Dale
J,
Newman
S.
Patient
expectations:
what
do
primary
care
patients
want
from
the
GP
and
how
far
does
meeting
expectations
affect
patient
satisfaction.
Fam
Pract
1995;
12
(2):
193-201.
31.
Stark
D,
Kiely
M,
Smith
A
et
al.
Reassurance
and
the
anxious
cancer
patient.
Br
J
Cancer
2004;
91:893-899.
32.
Platt
FW,
Keller
VF.
Empathic
communication:
a
teachable
and
learnable
skill.
J
Gen
Intern
Med.
1994;
9:222-226.
33.
Beckman
HB,
Frankel
RM,
Kihm
J,
Kulesza
G,
Geheb
OR.
Measurement
and
improvement
of
humanistic
skills
in
first
year
trainees.
J
Gen
Intern
Med.
1990;
5:42-45.
34.
Roter
DL,
Hall
JA,
Kern
DE,
Barker
LR,
Cole
KA,
Roca
RP.
Improving
physicians'
interviewing
skills
and
reducing
emotional
distress:
a
randomized
clinical
trial.
Arch
Intern
Med.
1995;
155:1877-1884.
35.
Debra
L.
Roter,
Dr.PHJudith
A.
Hall,
PhD
Yutaka
Aoki,
MS,
MHS.
Physician
gender
effects
in
medical
communication.
JAMA
2002;
288:756-764.
36.
Tore
G,
Per
V
et
al.
Observed
communication
skills:
how
do
they
relate
to
the
consultation
content?
A
nation-wide
study
of
graduate
medical
students
seeing
a
standardized
patient
for
a
first-time
consultation
in
general
practice
setting.
BMC
Medical
Education
2007,
7:43-52.
|

